Avicenna J Dent Res. 14(2):53-57.
doi: 10.34172/ajdr.2022.10
Original Article
Effect of Low-Level Laser Therapy on Trismus, Facial Swelling, and Pain Following Surgical Extraction of Impacted Lower Third Molars
Omid Soltaninia 1  , Leila Gholami 2, Hadi Hashemzehi 1, Javad Feradmal 3, Mehdi Parvan 4, Navid Rangzan 4, Amir Najafi 1, *
, Leila Gholami 2, Hadi Hashemzehi 1, Javad Feradmal 3, Mehdi Parvan 4, Navid Rangzan 4, Amir Najafi 1, * 
Author information:
1Assistant Professor of Oral and Maxillofacial Surgery, Department of Oral and Maxillofacial, School of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran
2Dental Researcher Center, Department of Periodontics, School of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran
3Department of Biostatistics, School of Health, Hamadan University of Medical Sciences, Hamadan, Iran
4Resident of Oral and Maxillofacial Surgery, Department of Oral and Maxillofacial, School of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran
*
Corresponding author: Amir Najafi,Assistant Professor of Oral and Maxillofacial Surgery, Department of Oral and Maxillofacial, School of Dentistry, Hamadan Email:
dr_amn69@yahoo.com
Abstract
Background: Light amplification by the stimulated emission of radiation (laser) is currently used as a therapy method for decreasing inflammation followed by oral surgeries. Therefore, the present study aimed at evaluating the effect of using diode low-power laser irradiation (photobiomodulation) on the amount of pain, swelling, and trismus due to latent mandibular third molar surgery (surgical removal of latent mandibular third molars).
Methods: In this double-blind randomized clinical trial study, 16 individuals with latent mandibular third molars with an identical condition were selected. The teeth were randomly assigned to two groups of laser irradiated intervention group and a non-irradiated control group. A 940 nm diode laser with an output power of 200 mW and an energy density of 12 J/cm2 was applied for 60 seconds at a distance of 1 cm three intraoral points and an extraoral point. The distance between incisal edges of upper and lower central teeth, the horizontal distance between corners of lips and auricle (LE), the vertical distance between the outer canthus of the eye and the mandibular angle (EA), and pain visual analogue scale were measured before surgery and two and seven days after surgery.
Results: There was no statistically significant difference between the two groups regarding EA and LE before intervention and on days 2 and 7 after intervention (P>0.05). However, the pain score was significantly higher before intervention (3.31±0.7 vs. 2.38±0.8, P=0.001) and on day 2 after intervention (6.5±1.32 vs. 4.5±0.97, P<0.001) in the control group. On day 7, a higher maximum jaw opening (MJO) was observed in the intervention group (40.68±5.76 vs. 36.81±4.35, P=0.04).
Conclusions: Adjunctive diode laser photobiomodulation after third molar surgery was associated with a significant reduction in pain and trismus.
Keywords: Laser therapy, Pain, Swelling, Maximum mouth opening, Photobiomodulation
Copyright and License Information
© 2022 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Soltaninia O, Gholami L, Hashemzehi H, Feradmal J, Parvan M, Rangzan N, et al. Effect of low-level laser therapy on trismus, facial swelling, and pain following surgical extraction of impacted lower third molars. Avicenna J Dent Res. 2022; 14(2):53-57. doi:10.34172/ajdr.2022.10
Introduction
One of the most common surgeries in the oral cavity is the extraction of impacted third molars which is usually performed under local anesthesia (1). Although the surgical process is not extensive regarding the trauma to the bone and soft tissue and the anatomical position of the area, it can lead to considerable inflammation and post-surgical complications for the patient (2). Moreover, due to physiological changes that occur (e.g., bleeding, swelling, stiffness, and pain), the quality of life of the patients decreases, and their activities such as eating and talking could be disrupted for about one week (3).
Light amplification by the stimulated emission of radiation (laser) is electromagnetic radiation, which has coherence, monochromaticity, and unidirectional properties unlike usual light. Different laser radiations are categorized based on their wavelength and absorbance in tissue, which may result in different applications. High-power laser radiations are usually used in surgeries, dermatology, and ophthalmology, while low-power laser radiations have such action as a bio-modulator, and many studies showed the effect of low-level laser therapy on cells and improving wound healing, decreasing pain, and facilitating the inflammation process (4-8). Moreover, its effects in dentistry have been assessed on dentinal sensitivity, temporomandibular problems, paresthesia of the lower jaw nerve due to trauma, herpetic ulcer healing, and the like (9-12).
So far, different methods have been used to reduce post-surgical complications of impacted third molar extraction such as the use of corticosteroids, non-steroidal anti-inflammatory drugs, drain, and low-power lasers (13-16). However, using low-power lasers is recommended due to their negligible side effects (17).
Since the results of available studies on photobiomodulation effects on pain, swelling, and trismus after impacted third molars surgical extraction are different, and different wavelengths and irradiation protocols play an important role (18-23), the present study was designed to assess the effect of using a 940 nm adjunctive laser irradiation on pain, swelling, and trismus after surgical extraction of the impacted mandibular third molars.
Materials and Methods
This double-blind randomized clinical trial study was conducted on 16 patients from volunteers referring to the Oral and Maxillofacial Surgery Department for surgical extraction of their impacted mandibular third molars. The inclusion criteria were a maximum age of 25 years and having a bilateral third molar tooth with equal latency type based on the classifications by Pell (24). The study was approved by the Research Ethics Committee of Hamadan University, and all patients signed an informed consent form for participation in the study.
Before surgery, maximum jaw opening (MJO) as well as the distance between incisal edges of upper central incisor and lower central incisor were measured. Likewise, the horizontal distance between lip commissure and tragus (LE) and the vertical distance between the outer canthus of the eye and mandibular angle (EA) were measured using Silk Sutures and recorded in millimeters for each patient.
A mandibular third molar tooth of one side was randomly allocated to each patient in the intervention group (laser radiation), and the other was assigned to the patients in control group (placebo irradiation). The teeth were removed at a two-week interval. Lower alveolar and buccal nerve anesthesia were achieved using 2 capsules of Lidocaine with 1:100000 epinephrine concentration. For all patients, a triangular flap was established to provide the required visibility and access. After surgery, the flap areas were closed using Silk Sutures, version 3.0 (Supa, Tehran, Iran).
In the intervention group, a continuous wave with 940 nm (Epic 10, Biolase, USA) diode laser with an output power of 200 Mw was irradiated for 60 seconds at a distance of 1cm from the tissue to achieve a 12 J/cm2 energy density on three intraoral points on the mandibular raphe, the sutures, and the buccal vestibular area of the surgical site. An extraoral site 1cm above the mandibular border at the origin of the master muscle was also irradiated with the same setting. The irradiation was performed in two sessions: immediately after surgery and 48 hours after laser. In the control group, a laser that was not turned on was applied in a completely similar manner. All surgeries were performed by an experienced oral and maxillofacial surgeon.
To decrease the possibility of wound infection, a 500 mg amoxicillin capsule was used every 8 hours for one week, and a chlorhexidine 0.2% mouthwash was prescribed for each patient twice a day for one week. The patients were allowed to use acetaminophen analgesics if needed but had to write down the number of pills used.
The distances measured before surgery were measured again two and seven days after surgery. Measurements were performed by an individual who was blinded to control and intervention groups. Moreover, for measuring pain level, a visual analogue scale was used at the defined time points after surgery (after elimination of anesthesia, and 1, 2, and 7 days after surgery). For this purpose, the patients were asked to score their pain rate from 1 to 10. Collected data were entered into SPSS version 24 software and analyzed using an independent T-test and Man-Whitney test. Further, the significance level was considered less than 0.05.
Results
Initially, a total of 23 patients were enrolled in the study. Considering the inclusion and exclusion criteria, 7 patients were excluded, and 16 patients were included in the final analysis (8 males and 8 females). The mean age was 21.45 ± 2.64 s(Range 19-25) years.
The comparison of EA, LE, pain, and MJO between the intervention and control groups is presented in Table 1 and Figure 1. As it can be observed, EA measurements indicated no statistically significant difference between the two groups before intervention and on days 2 and 7 after intervention (P > 0.05). Pain in both groups on day 2 increased and afterward declined by day 7 after intervention. However, the pain score was significantly higher immediately after surgery (3.31 ± 0.7 vs. 2.38 ± 0.8, P = 0.001) and on day 2 after intervention (6.5 ± 1.32 vs. 4.5 ± 0.97, P< 0.001) in the control group compared with the intervention group.
Table 1.
Comparison of EA, Pain, MJO, and LE Between the Intervention and Control Groups
|
Index
|
Time
|
Intervention Group
|
Control Group
|
P Value
|
| EA |
Immediately after surgery |
105.93 ± 6.39 |
105.63 ± 6.35 |
0.89 |
| Day 2 |
109.19 ± 6.94 |
110.63 ± 6.59 |
0.55 |
| Day 7 |
106.06 ± 6.52 |
106.76 ± 6.53 |
0.77 |
| Pain score |
Immediately after surgery |
2.38 ± 0.8 |
3.31 ± 0.7 |
0.001* |
| Day 2 |
4.5 ± 0.97 |
6.5 ± 1.32 |
< 0.001* |
| Day 7 |
1.5 ± 0.89 |
2.43 ± 1.89 |
0.08* |
| MJO |
Before intervention |
45.94 ± 5.58 |
45.38 ± 5.67 |
0.78 |
| Day 2 |
34.5 ± 6.79 |
30.5 ± 6 |
0.09* |
| Day 7 |
40.68 ± 5.76 |
36.81 ± 4.35 |
0.04* |
| LE |
Before intervention |
108.68 ± 6.03 |
108.12 ± 6.52 |
0.8 |
| Day 2 |
111.5 ± 6.06 |
115.75 ± 6.33 |
0.06* |
| Day 7 |
109.75 ± 5.95 |
109.75 ± 6.67 |
1 |
Note. MJO: Maximum jaw opening; LE: Horizontal distance between lip commissure and tragus; EA: Vertical distance between outer canthus of eye and mandibular angle.
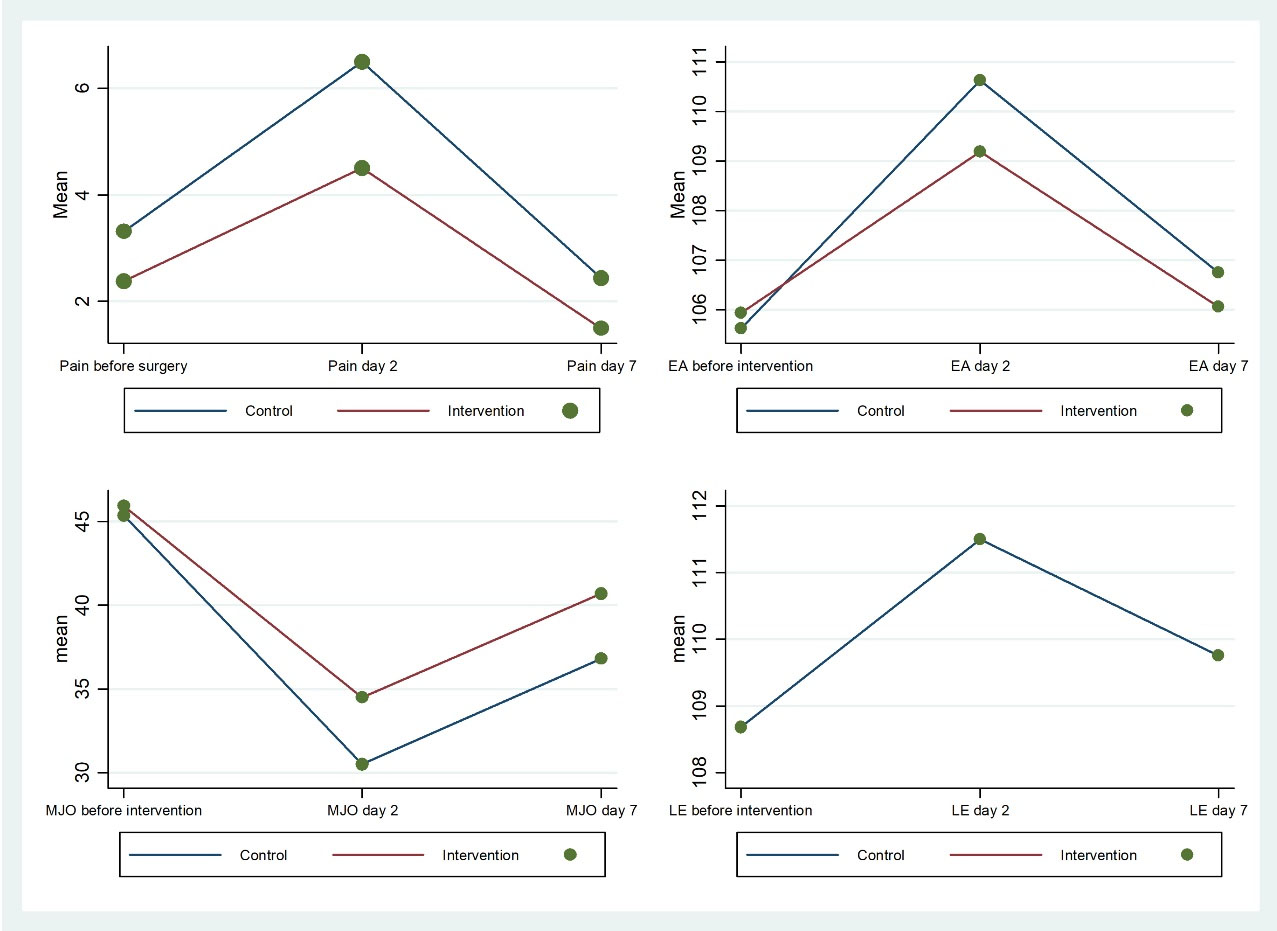
Figure 1.
Graphical Presentation of Comparison of EA, Pain, MJO, and LE Between the Intervention and Control Groups. Note. MJO: Maximum jaw opening; LE: Horizontal distance between lip commissure and tragus; EA: Vertical distance between outer canthus of eye and mandibular angle.
.
Graphical Presentation of Comparison of EA, Pain, MJO, and LE Between the Intervention and Control Groups. Note. MJO: Maximum jaw opening; LE: Horizontal distance between lip commissure and tragus; EA: Vertical distance between outer canthus of eye and mandibular angle.
MJO in both groups, after a slight decrease on day 2, increased on day 7 after the intervention in both groups. However, only on day 7 after intervention, this index was significantly higher in the intervention group (40.68 ± 5.76 vs. 36.81 ± 4.35, P = 0.04). Further, there was no significant difference in terms of the score of LE between the two groups immediately after surgery as well as 2 and 7 days after intervention (P > 0.05).
Discussion
This randomized clinical trial was conducted to investigate the effect of diode laser on the amount of pain, trismus, and swelling caused by latent mandibular third molar surgery. Different methods are available to measure the amount of swelling in the face. For example, in the study by Alan et al different rates of post-surgical swelling were found using 3-D scans of patients (25). However, in some previous studies, contact and direct measurements have been utilized (26,27). The current study also evaluated the amount of swelling by measuring the horizontal distance between the corners of lips and auricle and the vertical distance between the outer canthus of the eye and the mandibular angle.
Previous studies have shown that the amount of pain reached its maximum 3-5 hours after surgery, lasted for about 2-3 days, and then reduced until the seventh day (28). The results of the current study also revealed that on the seventh day, when the amount of pain greatly reduced, no difference was found between the two groups, but on the second day after the surgery when we expect the maximum pain, laser radiation significantly reduced pain reported by patients.
In previously conducted studies on the effect of laser on latent mandibular third molar surgery, the first laser to be studied was the He-Ne laser, which had no significant effect on pain and swelling after surgery in a study conducted by Carrillo et al but improved the amount of trismus significantly after one week (29).
The most common laser used in studies is the diode laser. In two separate studies, Markovic et al found that the use of diode laser (AlGaAs) wavelength /setting significantly improved the pain of patients as well as the amount of swelling that occurred after latent wisdom teeth surgery (20,21). In a study by Maria et al, patients with two latent mandibular third molars after surgery had one side under a low-power diode laser with a wavelength of 810 nm, power of 0.5 W, and density of 5 J/cm2, and it was observed that the use of diode laser did not have a significant effect on the amount of pain, swelling, and trismus caused by latent mandibular third molar surgery (30). In a study by Raiesian et al selected 44 patients with latent mandibular third molar surgery and examined the effects of low-power diode laser radiation with wavelength of 980 nm, power of 1.8 watts, and energy density of 18 J/cm2. The results showed that the use of diode laser had a significant effect on pain reduction after mandibular third molar surgery, but no significant effect was reported for the amount of swelling induced by surgery (27). Similarly, the results of the present study indicated that the use of diode laser had a significant effect on the reduction of pain and trismus following the latent mandibular third molar surgery. Compared to previous studies, it can be concluded that the radiation characteristics used (i.e., radiation wavelength and energy) could contribute to the difference in reported results.
Differences in irradiation protocols may also play a role in the variations in outcomes. In this study, we used a laser immediately after surgery and 48 hours after later. Røynesdal et al evaluated the effect of diode laser radiation before and after surgery on the amount of pain, trismus, and swelling, observing that laser radiation did not have a significant effect (31).
Some studies, in addition to the intraoral application, applied a laser extraorally similar to the design of the present study. For example, Aras and Güngörmüş used a diode laser both inside and outside the mouth and observed that the amount of trismus and swelling in the patients reduced significantly after 2 and 7 days (18). In another study, Aras and Güngörmüş addressed the effect of diode low-power laser inside and outside the mouth on the amount of trismus and swelling after latent mandibular third molar surgery. These were in accordance with the findings of the present study. These findings may indicate that the use of adjunctive low-power laser irradiation extraorally may have a greater effect on the reduction of swelling and trismus (19). However, Alam et al used extraoral application of diode laser immediately and 2 days after surgery, finding no significant laser-induced effects, except for the reported pain on the seventh day (25). In the present study, we used a different protocol; in other words, the laser was used immediately after surgery and 48 hours later, intraorally and extraorally on the site of the Masseter muscle, and the results indicated the positive effects on reduction of trismus measured via MJO.
In the current study, to reduce confounding factors, patients with a similar bilateral latent mandibular third molar and degree of surgical difficulty were studied in a double-blinded split-mouth design.
The obtained results demonstrated a positive effect of adjunctive low power laser photobiomodulation on the complications of latent mandibular third molar surgery. These results may be due to the underlying mechanism of action of low-level laser therapy on synthesizing and releasing endorphins, increasing the threshold for pain tolerance, and blocking neurons, which can reduce pain sensation. Moreover, improved postoperative inflammation and swelling can be achieved by increasing the number and diameter of lymphatic vessels, reducing vascular permeability, as well as controlling inflammatory mediators such as PGE, IL-6, and IL-10 (32-36).
Conclusions
According to the results of the current study, adjunctive intraoral and extraoral diode laser photobiomodulation significantly reduced pain and trismus after latent mandibular third molar surgery.
Authors’ Contribution
All authors equally contributed to the design and implementation of the research, analysis of the results, and writing the article.
Conflict of Interest Disclosures
The authors declare that they have no conflict of interests.
Ethical Statement
The present study was approved by the Ethics Committee of the Hamadan University of Medical Sciences and was performed in accordance with the Declaration of Helsinki. Moreover, all patients expressed their willingness to participate in the study (IR.UMSHA.REC.1396.471).
References
- Leonard MS. Removing third molars: a review for the general practitioner. J Am Dent Assoc 1992; 123(2):77-8. doi: 10.14219/jada.archive.1992.0041 [Crossref] [ Google Scholar]
- Sisk AL, Mosley RO, Martin RP. Comparison of preoperative and postoperative diflunisal for suppression of postoperative pain. J Oral Maxillofac Surg 1989; 47(5):464-8. doi: 10.1016/0278-2391(89)90278-4 [Crossref] [ Google Scholar]
- Miloro M, Ghali G, Larsen P, Peterson LJ, Waite P. Peterson’s Principles of Oral and Maxillofacial Surgery. PMPH-USA; 2004.
- Viegas VN, Abreu ME, Viezzer C, Machado DC, Filho MS, Silva DN. Effect of low-level laser therapy on inflammatory reactions during wound healing: comparison with meloxicam. Photomed Laser Surg 2007; 25(6):467-73. doi: 10.1089/pho.2007.1098 [Crossref] [ Google Scholar]
- Heravi F, Moradi A, Ahrari F. The effect of low level laser therapy on the rate of tooth movement and pain perception during canine retraction. Oral Health Dent Manag 2014; 13(2):183-8. [ Google Scholar]
- Parirokh M, Dabiri S, Bahrampour A, Homayon Zadeh M, Eghbal MJ. Effect of low power laser on incisional wound healing. Iran Endod J 2006; 1(4):157-60. [ Google Scholar]
- Moosavi H, Maleknejad F, Sharifi M, Ahrari F. A randomized clinical trial of the effect of low-level laser therapy before composite placement on postoperative sensitivity in class V restorations. Lasers Med Sci 2015; 30(4):1245-9. doi: 10.1007/s10103-014-1565-9 [Crossref] [ Google Scholar]
- Park JJ, Kang KL. Effect of 980-nm GaAlAs diode laser irradiation on healing of extraction sockets in streptozotocin-induced diabetic rats: a pilot study. Lasers Med Sci 2012; 27(1):223-30. doi: 10.1007/s10103-011-0944-8 [Crossref] [ Google Scholar]
- Parker S. Low-level laser use in dentistry. Br Dent J 2007; 202(3):131-8. doi: 10.1038/bdj.2007.75 [Crossref] [ Google Scholar]
- Ozen T, Orhan K, Gorur I, Ozturk A. Efficacy of low level laser therapy on neurosensory recovery after injury to the inferior alveolar nerve. Head Face Med 2006; 2:3. doi: 10.1186/1746-160x-2-3 [Crossref] [ Google Scholar]
- Fikácková H, Dostálová T, Navrátil L, Klaschka J. Effectiveness of low-level laser therapy in temporomandibular joint disorders: a placebo-controlled study. Photomed Laser Surg 2007; 25(4):297-303. doi: 10.1089/pho.2007.2053 [Crossref] [ Google Scholar]
- Marsilio AL, Rodrigues JR, Borges AB. Effect of the clinical application of the GaAlAs laser in the treatment of dentine hypersensitivity. J Clin Laser Med Surg 2003; 21(5):291-6. doi: 10.1089/104454703322564505 [Crossref] [ Google Scholar]
- Mocan A, Kişnişci R, Uçok C. Stereophotogrammetric and clinical evaluation of morbidity after removal of lower third molars by two different surgical techniques. J Oral Maxillofac Surg 1996; 54(2):171-5. doi: 10.1016/s0278-2391(96)90441-3 [Crossref] [ Google Scholar]
- Walsh LJ. Walsh LJThe current status of low level laser therapy in dentistryPart 1Soft tissue applications. Aust Dent J 1997; 42(4):247-54. doi: 10.1111/j.1834-7819.1997.tb00129.x [Crossref] [ Google Scholar]
- Mehrabi M, Allen JM, Roser SM. Therapeutic agents in perioperative third molar surgical procedures. Oral Maxillofac Surg Clin North Am 2007; 19(1):69-84. doi: 10.1016/j.coms.2006.11.010 [Crossref] [ Google Scholar]
- Buyukkurt MC, Gungormus M, Kaya O. The effect of a single dose prednisolone with and without diclofenac on pain, trismus, and swelling after removal of mandibular third molars. J Oral Maxillofac Surg 2006; 64(12):1761-6. doi: 10.1016/j.joms.2005.11.107 [Crossref] [ Google Scholar]
- Kumar N, Prasad K, Ramanujam L, K R, Dexith J, Chauhan A. Evaluation of treatment outcome after impacted mandibular third molar surgery with the use of autologous platelet-rich fibrin: a randomized controlled clinical study. J Oral Maxillofac Surg 2015; 73(6):1042-9. doi: 10.1016/j.joms.2014.11.013 [Crossref] [ Google Scholar]
- Aras MH, Güngörmüş M. The effect of low-level laser therapy on trismus and facial swelling following surgical extraction of a lower third molar. Photomed Laser Surg 2009; 27(1):21-4. doi: 10.1089/pho.2008.2258 [Crossref] [ Google Scholar]
- Aras MH, Güngörmüş M. Placebo-controlled randomized clinical trial of the effect two different low-level laser therapies (LLLT)--intraoral and extraoral--on trismus and facial swelling following surgical extraction of the lower third molar. Lasers Med Sci 2010; 25(5):641-5. doi: 10.1007/s10103-009-0684-1 [Crossref] [ Google Scholar]
- Marković AB, Todorović L. Postoperative analgesia after lower third molar surgery: contribution of the use of long-acting local anesthetics, low-power laser, and diclofenac. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 102(5):e4-8. doi: 10.1016/j.tripleo.2006.02.024 [Crossref] [ Google Scholar]
- Markovic A, Todorovic L. Effectiveness of dexamethasone and low-power laser in minimizing oedema after third molar surgery: a clinical trial. Int J Oral Maxillofac Surg 2007; 36(3):226-9. doi: 10.1016/j.ijom.2006.10.006 [Crossref] [ Google Scholar]
- Fernando S, Hill CM, Walker R. A randomised double blind comparative study of low level laser therapy following surgical extraction of lower third molar teeth. Br J Oral Maxillofac Surg 1993; 31(3):170-2. doi: 10.1016/0266-4356(93)90118-g [Crossref] [ Google Scholar]
- Amarillas-Escobar ED, Toranzo-Fernández JM, Martínez-Rider R, Noyola-Frías MA, Hidalgo-Hurtado JA, Serna VM. Use of therapeutic laser after surgical removal of impacted lower third molars. J Oral Maxillofac Surg 2010; 68(2):319-24. doi: 10.1016/j.joms.2009.07.037 [Crossref] [ Google Scholar]
- Pell GJ. Impacted mandibular third molars: classification and modified techniques for removal. Dent Digest 1933; 39:330-8. [ Google Scholar]
- Alan H, Yolcu Ü, Koparal M, Özgür C, Öztürk SA, Malkoç S. Evaluation of the effects of the low-level laser therapy on swelling, pain, and trismus after removal of impacted lower third molar. Head Face Med 2016; 12(1):25. doi: 10.1186/s13005-016-0121-1 [Crossref] [ Google Scholar]
- Eshghpour M, Ahrari F, Takallu M. Is low-level laser therapy effective in the management of pain and swelling after mandibular third molar surgery? J Oral Maxillofac Surg 2016;74(7):1322.e1-1322.e8. 10.1016/j.joms.2016.02.030.
- Raiesian S, Khani M, Khiabani K, Hemmati E, Pouretezad M. Assessment of low-level laser therapy effects after extraction of impacted lower third molar surgery. J Lasers Med Sci 2017; 8(1):42-5. doi: 10.15171/jlms.2017.08 [Crossref] [ Google Scholar]
- Lago-Méndez L, Diniz-Freitas M, Senra-Rivera C, Gude-Sampedro F, Gándara Rey JM, García-García A. Relationships between surgical difficulty and postoperative pain in lower third molar extractions. J Oral Maxillofac Surg 2007; 65(5):979-83. doi: 10.1016/j.joms.2006.06.281 [Crossref] [ Google Scholar]
- Carrillo JS, Calatayud J, Manso FJ, Barberia E, Martinez JM, Donado M. A randomized double-blind clinical trial on the effectiveness of helium-neon laser in the prevention of pain, swelling and trismus after removal of impacted third molars. Int Dent J 1990; 40(1):31-6. [ Google Scholar]
- López-Ramírez M, Vílchez-Pérez MA, Gargallo-Albiol J, Arnabat-Domínguez J, Gay-Escoda C. Efficacy of low-level laser therapy in the management of pain, facial swelling, and postoperative trismus after a lower third molar extraction A preliminary study. Lasers Med Sci 2012; 27(3):559-66. doi: 10.1007/s10103-011-0936-8 [Crossref] [ Google Scholar]
- Røynesdal AK, Björnland T, Barkvoll P, Haanaes HR. The effect of soft-laser application on postoperative pain and swelling A double-blind, crossover study. Int J Oral Maxillofac Surg 1993; 22(4):242-5. doi: 10.1016/s0901-5027(05)80646-0 [Crossref] [ Google Scholar]
- Hawkins D, Abrahamse H. Phototherapy—a treatment modality for wound healing and pain relief. Afr J Biomed Res 2007; 10(2):99-109. [ Google Scholar]
- Boschi ES, Leite CE, Saciura VC, Caberlon E, Lunardelli A, Bitencourt S. Anti-Inflammatory effects of low-level laser therapy (660 nm) in the early phase in carrageenan-induced pleurisy in rat. Lasers Surg Med 2008; 40(7):500-8. doi: 10.1002/lsm.20658 [Crossref] [ Google Scholar]
- Hagiwara S, Iwasaka H, Okuda K, Noguchi T. GaAlAs (830 nm) low-level laser enhances peripheral endogenous opioid analgesia in rats. Lasers Surg Med 2007; 39(10):797-802. doi: 10.1002/lsm.20583 [Crossref] [ Google Scholar]
- Sakurai Y, Yamaguchi M, Abiko Y. Inhibitory effect of low-level laser irradiation on LPS-stimulated prostaglandin E2 production and cyclooxygenase-2 in human gingival fibroblasts. Eur J Oral Sci 2000; 108(1):29-34. doi: 10.1034/j.1600-0722.2000.00783.x [Crossref] [ Google Scholar]
- Chow RT, David MA, Armati PJ. 830 nm laser irradiation induces varicosity formation, reduces mitochondrial membrane potential and blocks fast axonal flow in small and medium diameter rat dorsal root ganglion neurons: implications for the analgesic effects of 830 nm laser. J Peripher Nerv Syst 2007; 12(1):28-39. doi: 10.1111/j.1529-8027.2007.00114.x [Crossref] [ Google Scholar]