Avicenna J Dent Res. 14(1):39-43.
doi: 10.34172/ajdr.2022.07
Case Report
Conservative Dental Management of a Patient With Amelogenesis Imperfecta Under Oral Sedation: A Case Report
Leila Eftekhar 1  , Hosna Ebrahimi Zadeh 2
, Hosna Ebrahimi Zadeh 2  , Khashayar Sanjari 3, *
, Khashayar Sanjari 3, * 
Author information:
1Assistant Professor, Department of Pediatric Dentistry, Faculty of Dentistry, Alborz University of Medical Sciences, Karaj, Iran
2Assistant Professor, Department of Restorative Dentistry, Faculty of Dentistry, Shahid Beheshti University of Medical Sciences, Tehran, Iran
3Assistant Professor, Department of Pediatric Dentistry, Faculty of Dentistry, Iran University of Medical Sciences, Tehran, Iran
*
Corresponding author: Khashayar Sanjari, Assistant Professor, Department of Pediatric Dentistry, Faculty of Dentistry, Iran University of Medical Sciences, Tehran, Iran, Tel:+989122986587, Email:
Khashayarsanjari@gmail.com
Abstract
Amelogenesis imperfecta (AI) is a rare hereditary developmental disease that has a significant effect on the enamel structure. Both primary and permanent dentition could be affected by this condition. The pivotal characteristics are loss of the tooth structure, wear of enamel, and exposed dentinal areas at the occlusal surface of posterior teeth. AI may be inherited in autosomal dominant, autosomal recessive, or X‐linked types. Treatments of AI cases should be initiated in childhood and continue into adolescence. Considering that AI is a rare and heterogeneous condition, the dental team faces various difficulties regarding choosing the appropriate treatment plan. The oral rehabilitation of patients with AI is a challenging condition that needs a multidisciplinary approach. Many treatment options have been reported for solving cosmetic and restorative problems in AI cases. The conservative treatment plan in this hypoplastic-hypomature AI case included esthetic rehabilitation with a sequential method, innovative non-invasive pulp-therapy methods, and dental restorations under oral sedation. The written consent for the treatments was obtained after consultation with the child and his parents.
Keywords: Amelogenesis imperfecta, Conscious sedation, Dental enamel hypoplasia, Tooth hypomineralization
Copyright and License Information
© 2022 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Eftekhar L, Ebrahimi Zadeh H, Sanjari K. Conservative dental management of a patient with amelogenesis imperfecta under oral sedation: a case report. Avicenna J Dent Res. 2022; 14(1):39-43. doi:10.34172/ajdr.2022.07
Background
Amelogenesis imperfecta (AI) is an uncommon hereditary developmental disease which has a crucial impact on the structure of enamel (1). Both primary and permanent teeth can be influenced by this condition. The pivotal characteristics of this disease include loss of the tooth structure, wear of enamel, and exposed dentinal areas at the occlusal surface of posterior teeth. Hypoplasia and enamel degradation could lead to cosmetic issues, tooth hypersensitivity, predilection to caries formation, and vertical dimension decreases (2,3). AI may be inherited in autosomal dominant, autosomal recessive, or X-linked types (4). In addition, it has 3 major types (i.e., hypoplastic, hypomatured, and hypocalcified) depending on the stages of the tooth formation process (5).
Treatments of AI cases should be initiated at childhood and continue into adolescence (6). Given that AI is a rare and heterogeneous condition, the dental team encounters a wide variety of difficulties with respect to selecting an accurate treatment plan (7). Patients’ rehabilitation with AI is a challenging condition that requires the use of a multidisciplinary approach. Various treatment alternatives have been reported for solving cosmetic problems and restorative treatments in AI cases (8,9).
The conservative treatment plan in this hypoplastic-hypomature AI case consisted of esthetic rehabilitation with a sequential method, innovative non-invasive pulp therapy methods, and dental restorations under mild oral sedation.
Case Report
Medical and Dental History
A 10 years old boy with the chief complaint of tooth pain and esthetic demands was referred to the Department of Pediatric Dentistry, Zanjan Dental School. The tooth sensitivity led to discomfort during regular drinking and eating.
He was dissatisfied with the presence of spots on anterior teeth (Figure 1). The medical history of the patient included a Choledochal cyst and clubfoot. The general physical condition was normal and his vital signs were within a normal range. The examination of cardiovascular, respiratory, and neural systems did not demonstrate any specific symptoms. The child has never visited the dentist before.

Figure 1.
Hypoplastic-hypomature Maxillary and Mandibular Anterior Teeth.
.
Hypoplastic-hypomature Maxillary and Mandibular Anterior Teeth.
Conservative and Preventive Management of the Overall Oral Health Condition
Recommendations for improving oral hygiene were made, including the daily use of casein phosphopeptide-amorphous calcium phosphate (MI Paste; RecaldentTM) in a pea-size (10) to induce the buffering capacity of the saliva with calcium and phosphate. Daily consumption of 5 g of xylitol gum (Hager & Werken GmbH & Co. KG, Duisburg, Germany) three times a day was also prescribed to reduce the risk of caries (11). Finally, oxalate desensitizer (BisBlock, BISCO, Inc, Schaumburg, IL, USA) was applied for 30 seconds and rinsed to diminish tooth sensitivity (12).
Conservative Behavior Management
The child was considered negative on Frankl’s Rating Scale. At the first visit, the “Tell Show Do” approach was applied to decrease anxiety. Audiovisual distraction (as virtual reality) was utilized but it was not effective. Due to the known needle phobia in the child, the treatments requiring anesthesia were performed under mild oral sedation. All stages of treatment were performed under the supervision of an experienced anesthesiologist, and vital signs were monitored carefully. Parents were asked to keep the child NPO for 6 hours. Oral melatonin 0.3 mg/kg (Vegetarian Formula, Vitane Pharmaceuticals Pvt. Ltd., NY, USA) dissolved in the fruit juice was prescribed 1 hour before treatment initiation (13). The child reported no pain or discomfort during the injection and no adverse reactions during pulp therapy.
Conservative Esthetic Treatments
The written consent for the treatments was obtained after consultation with the child and his parents. Bleaching was applied to the second maxillary left incisor to diminish the contrast between white spots and unaffected areas of the tooth. In addition, 35% hydrogen peroxide-based bleaching material (Whiteness HP Maxx, FGM, Joinville, SC, Brazil) was employed over the buccal surface of the tooth 3 times and remained on the tooth for 15 minutes each time. In the next session, hypoplastic spots were treated with microabrasion. The tooth was isolated by a rubber dam, and the abrasive paste (Opalustre, Ultradent Products, South Jordan, UT, USA), comprising of silicon carbamide microparticulate paste and 6.6% hydrochloric acid, was applied as well. Resin infiltration therapy (Icon, DMG Products, Hamburg, Germany) was performed 2 weeks later (14). Further, 15% HCL was utilized for 2 minutes, and then rinsed off with water spray for 30 seconds and underwent drying. Ethanol was used for 30 seconds followed by air-drying. ICON-Infiltrant was applied and remained on the buccal surface of the tooth for 3 minutes. The excess resin was removed by a cotton roll and then cured for 40 seconds (Figure 2).
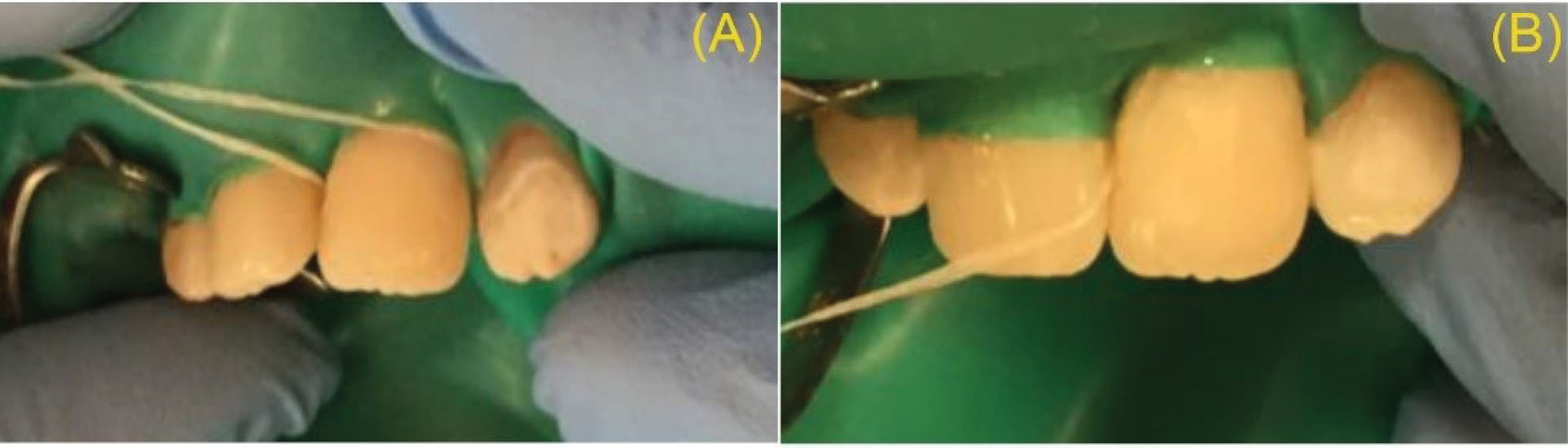
Figure 2.
Before (A) and Instantly After (B) Resin Infiltration (ICON-Infiltrant) of Maxillary Lateral Incisor.
.
Before (A) and Instantly After (B) Resin Infiltration (ICON-Infiltrant) of Maxillary Lateral Incisor.
The appearance of other maxillary and mandibular incisors was improved by composite veneers (Herculite Ultra, enamel shade [Kerr Corporation, Orange, CA USA], Figure 3). Direct composite restorations could conceal tooth discolorations and hypoplastic spots and ameliorate dental esthetics. It needs less or no preparation to protect the tooth structure. The child and his parents were extremely happy and satisfied with the cosmetic result.

Figure 3.
Composite Veneers of Maxillary and Mandibular Incisors.
.
Composite Veneers of Maxillary and Mandibular Incisors.
Conservative Pulp Treatments
In the first upper and lower right molars, indirect pulp capping was considered according to the amount of caries in the teeth. To reduce the sensation of pain during anesthesia, the cartridge was heated to 42 °C (15). Then, 1.4 mL of 4% articaine cartridge with 1: 100 000 epinephrine (Septanest N., Septodont, France) was used for more effective anesthesia. Photodynamic therapy (PDT) with 50 mW power at 60 seconds with 660 nm wavelength was applied to reduce the amount of mutants and lactobacillus in the remaining leathery dentin (Hager and Werken GmbH and Co. Duisburg, Germany). In this tooth, Theracal (Bisco, Schaumburg, IL, USA) was the capping material of choice.
Due to the spread of caries to the pulp borders, partial pulpotomy was considered in the first left upper and lower molars (Figure 4). The capping material of choice in this tooth was Biodentine (Septodont, Saint-Maur-des-Fossés, France). A gentle tapping was performed before opening a Biodentine capsule. To mix the powder, five drops of liquid were dispensed into the capsule, which was triturated for 30 seconds. The mixture was placed into the pulp chamber, and the setting reaction was completed in 12 minutes (16).

Figure 4.
Partial Pulpotomy of Maxillary Left Molar Using Biodentine.
.
Partial Pulpotomy of Maxillary Left Molar Using Biodentine.
Cervical pulpotomy was performed for both upper second primary molars using Biodentine. All maxillary, mandibular primary, and permanent molars were restored by stainless steel crowns.
Conservative Orthodontic Treatment
A cephalometric radiograph (Figure 5) analysis revealed a hyperdivergent clockwise rotation of jaw bases and confirmed skeletal open bite. To reduce the problem, trans-palatal arch (TPA) was considered for the patient to facilitate maxillary molar intrusion. Additionally, to control vertical dimension, a lingual arch was employed in the mandible (Figure 6). This conservative treatment approach was considered to simplify future comprehensive orthodontic treatments.

Figure 5.
Lateral Cephalometric Analysis Indicated Skeletal Open Bite.
.
Lateral Cephalometric Analysis Indicated Skeletal Open Bite.

Figure 6.
(A) Occlusal View of Maxillary and Mandibular Arch Before Treatment and (B) Occlusal View of Maxillary and Mandibular Arch After Oral Rehabilitation, TPA of Maxillary Arch for Molar Intrusion and Lingual Arch of Mandibular Arch for Vertical Control. Note. TPA: Trans-palatal arch.
.
(A) Occlusal View of Maxillary and Mandibular Arch Before Treatment and (B) Occlusal View of Maxillary and Mandibular Arch After Oral Rehabilitation, TPA of Maxillary Arch for Molar Intrusion and Lingual Arch of Mandibular Arch for Vertical Control. Note. TPA: Trans-palatal arch.
Discussion
AI is a dental anomaly comprising of hereditary disorders that influence the quality and/or quantity of the enamel (17). AI management could be disputing because of enamel fragility, extended pulp horns, and pulp chambers in children and young adults and severe tooth sensitivity. This condition leads to a lack of self-esteem, anxiety, and social dysfunction (18,19). AI may induce crucial restorative and occasional orthodontic challenges for practitioners (20). The management of AI cases depends on the severity of the symptoms, type of dentition, age, and the chief complaint of the patient. Numerous dental treatments have been suggested for the management of AI patients, including surgical crown lengthening and metal-ceramic-fixed dental prostheses (21), and composite rehabilitation followed by orthodontic treatment (22).
In this case report, the dental treatments of an AI child were performed with a non-invasive approach. The main difference between this case report and similar ones is the conservative approach in all dental treatments. Ordinary, dental treatments for children with known phobias are performed under general anesthesia (23), but sedation has been successfully applied due to the conservative aspects of the treatments in this case. It should be noted that passive or active restraint was not applied in any stages of dental treatments. To the best of our knowledge, this is the first case report utilizing oral sedation in the management of an AI case.
In most cases, invasive methods such as all-ceramic crowns have been used to treat cosmetic problems in AI cases (24,25). All-ceramic veneers can be prescribed when skeletal growth and soft tissue development are complete. Given that the child is 10 years old in this case, and the age of completion of growth is 18-20 years, full mouth fixed prosthetic restoration could not be chosen to improve the esthetic condition of the child (26). Previously, the sequential method has been employed in case reports, but this technique has been used in adults in most cases (27,28). The innovation of this report case, compared to other case reports, is that sequential minimally invasive techniques were successfully applied in a 10 years old patient.
Enamel deficiency makes teeth extremely sensitive to thermal and contact stimuli. Composite resin restorations are a solution to this problem as they protect the remaining structure. After the restoration of all teeth with a direct composite resin, the patient no longer had esthetic complaints and could restore his normal eating habits. Rizzo reported a similar successful esthetic rehabilitation of an AI case by direct composite resin in a 38 years old patient (29).
Another superiority of this case report to similar AI case reports was the use of PDT for indirect pulp capping (IPC). PDT is a conservative technique that applies a low-level laser to cease the growth of Streptococcus mutans (30). Based on the result of this study, de Oliveira et al also concluded that PDT could be a suitable choice for the conservative management of dental caries (31).
In this case, conservative partial pulpotomy was used instead of cervical pulpotomy in permanent open apex teeth. Additionally, in this case, Biodentine was successfully applied for partial pulpotomy and could provoke the formation of a more continuous mineralized dentinal bridge with a low-level pulp response compared to calcium hydroxide (32). This material is more consistent with the conservative concept of the present study in comparison with calcium hydroxide. According to our knowledge, this is the first case report using Biodentine in an AI case.
Conclusions
Children and adolescents with AI have several oral problems. Management of dental conflicts in these children is possible with non-invasive methods. The use of innovative conservative dental treatment methods could provide appropriate clinical results for patients and establish relaxation during treatment (Figure 7).
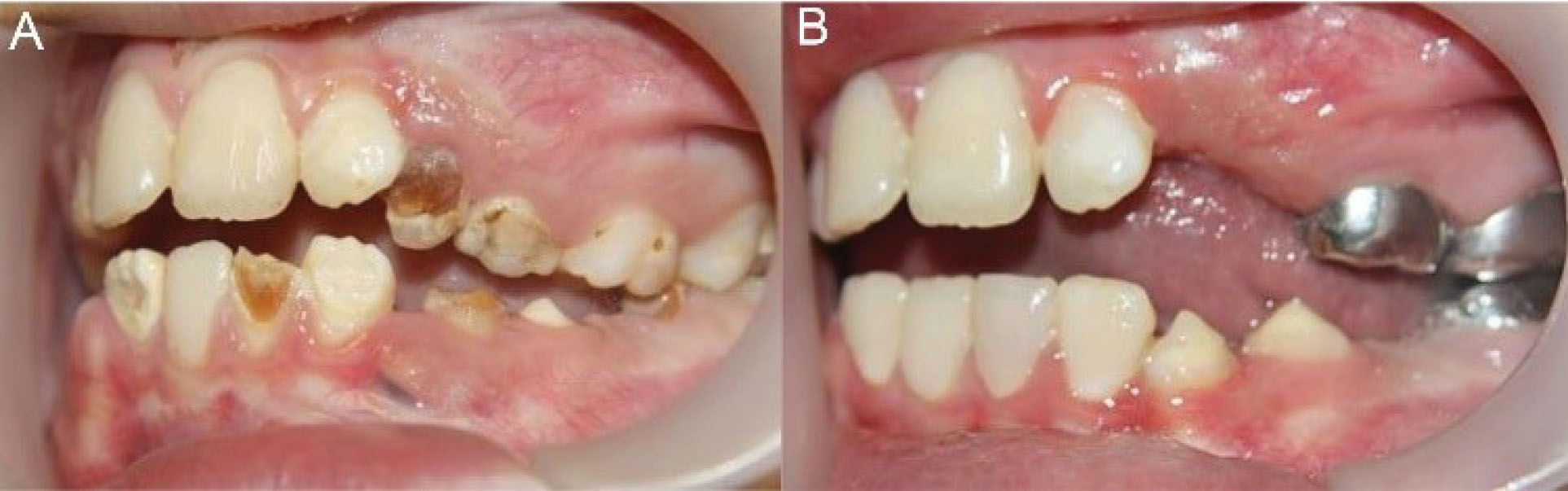
Figure 7.
Lateral View of (A) Before and (B) After Full Mouth Rehabilitation.
.
Lateral View of (A) Before and (B) After Full Mouth Rehabilitation.
Authors’ Contribution
LE and HE contributed in case treatment, KHS contributed in manuscript preparation.
Conflict of Interest Disclosures
The authors declare that they have no conflict of interests.
Ethical Statement
Informed consent was obtained from the patient’s parents for publication of the report.
Funding
None.
References
- Ardu S, Duc O, Krejci I, Perroud R. Amelogenesis imperfecta: a conservative and progressive adhesive treatment concept. Oper Dent 2013; 38(3):235-41. doi: 10.2341/11-437-s [Crossref] [ Google Scholar]
- Kamble VD, Parkhedkar RD. Multidisciplinary approach for restoring function and esthetics in a patient with amelogenesis imperfecta: a clinical report. J Clin Diagn Res 2013; 7(12):3083-5. doi: 10.7860/jcdr/2013/6665.3860 [Crossref] [ Google Scholar]
- Quandalle C, Boillot A, Fournier B, Garrec P, M DLD-M, Kerner S. Gingival inflammation, enamel defects, and tooth sensitivity in children with amelogenesis imperfecta: a case-control study. J Appl Oral Sci 2020; 28:e20200170. doi: 10.1590/1678-7757-2020-0170 [Crossref] [ Google Scholar]
- Aldred MJ, Savarirayan R, Crawford PJ. Amelogenesis imperfecta: a classification and catalogue for the 21st century. Oral Dis 2003; 9(1):19-23. doi: 10.1034/j.1601-0825.2003.00843.x [Crossref] [ Google Scholar]
- Witkop CJ, Jr Jr. Amelogenesis imperfecta, dentinogenesis imperfecta and dentin dysplasia revisited: problems in classification. J Oral Pathol 1988; 17(9-10):547-53. doi: 10.1111/j.1600-0714.1988.tb01332.x [Crossref] [ Google Scholar]
- Ergun G, Ataol AS. An interdisciplinary approach for hypoplastic amelogenesis imperfecta: a case report. Open Dent J 2018; 12:466-75. doi: 10.2174/1874210601812010466 [Crossref] [ Google Scholar]
- Adorno-Farias D, Ortega-Pinto A, Gajardo P, Salazar A, Morales-Bozo I, Werlinger F. Diversity of clinical, radiographic and genealogical findings in 41 families with amelogenesis imperfecta. J Appl Oral Sci 2019; 27:e20180359. doi: 10.1590/1678-7757-2018-0359 [Crossref] [ Google Scholar]
- Kwok-Tung L, King NM. The restorative management of amelogenesis imperfecta in the mixed dentition. J Clin Pediatr Dent 2006; 31(2):130-5. doi: 10.17796/jcpd.31.2.b575277016661476 [Crossref] [ Google Scholar]
- Strauch S, Hahnel S. Restorative treatment in patients with amelogenesis imperfecta: a review. J Prosthodont 2018; 27(7):618-23. doi: 10.1111/jopr.12736 [Crossref] [ Google Scholar]
- Dashper SG, Catmull DV, Liu SW, Myroforidis H, Zalizniak I, Palamara JE. Casein phosphopeptide-amorphous calcium phosphate reduces Streptococcus mutans biofilm development on glass ionomer cement and disrupts established biofilms. PLoS One 2016; 11(9):e0162322. doi: 10.1371/journal.pone.0162322 [Crossref] [ Google Scholar]
- Milgrom P, Ly KA, Rothen M. Xylitol and its vehicles for public health needs. Adv Dent Res 2009; 21(1):44-7. doi: 10.1177/0895937409335623 [Crossref] [ Google Scholar]
- Firouzmandi M, Valipour F, Roshanzamir M, Mobaleghi T. The effect of oxalate-based desensitizers on the microleakage and shear bond strength of resin modified glass ionomer. J Clin Exp Dent 2017; 9(10):e1183-e8. doi: 10.4317/jced.52946 [Crossref] [ Google Scholar]
- Ansari G, Fathi M, Fallahinejad Ghajari M, Bargrizan M, Eghbali A. Oral melatonin versus midazolam as premedication for intravenous sedation in pediatric dental patients. J Dent (Tehran) 2018; 15(5):317-24. [ Google Scholar]
- Shahroom NSB, Mani G, Ramakrishnan M. Interventions in management of dental fluorosis, an endemic disease: a systematic review. J Family Med Prim Care 2019; 8(10):3108-13. doi: 10.4103/jfmpc.jfmpc_648_19 [Crossref] [ Google Scholar]
- Aravena PC, Barrientos C, Troncoso C, Coronado C, Sotelo-Hitschfeld P. Effect of warming anesthetic on pain perception during dental injection: a split-mouth randomized clinical trial. Local Reg Anesth 2018; 11:9-13. doi: 10.2147/lra.s147288 [Crossref] [ Google Scholar]
- Eftekhar L, Ashraf H, Jabbari S. Management of invasive cervical root resorption in a mandibular canine using Biodentine as a restorative material: a case report. Iran Endod J 2017; 12(3):386-9. doi: 10.22037/iej.v12i3.16668 [Crossref] [ Google Scholar]
- Pousette Lundgren G, Karsten A, Dahllöf G. Oral health-related quality of life before and after crown therapy in young patients with amelogenesis imperfecta. Health Qual Life Outcomes 2015; 13:197. doi: 10.1186/s12955-015-0393-3 [Crossref] [ Google Scholar]
- Bouvier D, Duprez JP, Pirel C, Vincent B. Amelogenesis imperfecta--a prosthetic rehabilitation: a clinical report. J Prosthet Dent 1999; 82(2):130-1. doi: 10.1016/s0022-3913(99)70144-7 [Crossref] [ Google Scholar]
- Patel M, McDonnell ST, Iram S, Chan MF. Amelogenesis imperfecta-lifelong management Restorative management of the adult patient. Br Dent J 2013; 215(9):449-57. doi: 10.1038/sj.bdj.2013.1045 [Crossref] [ Google Scholar]
- Ayers KM, Drummond BK, Harding WJ, Salis SG, Liston PN. Amelogenesis imperfecta--multidisciplinary management from eruption to adulthood Review and case report. N Z Dent J 2004; 100(4):101-4. [ Google Scholar]
- Labidi A, Bekri S, Mabrouk Y, Ben Mustapha J, Omezzine M, Ghoul-Mazgar S. Amelogenesis imperfecta with Class III malocclusion, reduced crown size and decreased OVD: a multi-disciplinary management and a 5-year follow-up. Clin Case Rep 2020; 8(8):1440-4. doi: 10.1002/ccr3.2874 [Crossref] [ Google Scholar]
- Abd Alraheam I, Donovan T. Management of amelogenesis imperfecta in an adult patient: a short review and clinical report. Br Dent J 2020; 229(4):239-43. doi: 10.1038/s41415-020-1990-z [Crossref] [ Google Scholar]
- Taskinen H, Kankaala T, Rajavaara P, Pesonen P, Laitala ML, Anttonen V. Self-reported causes for referral to dental treatment under general anaesthesia (DGA): a cross-sectional survey. Eur Arch Paediatr Dent 2014; 15(2):105-12. doi: 10.1007/s40368-013-0071-2 [Crossref] [ Google Scholar]
- Büchi D, Fehmer V, Sailer I, Wolleb K, Jung R. Minimally invasive rehabilitation of a patient with amelogenesis imperfecta. Int J Esthet Dent 2014; 9(2):134-45. [ Google Scholar]
- Setien VJ, Roshan S, Nelson PW. Clinical management of discolored teeth. Gen Dent 2008; 56(3):294-300. [ Google Scholar]
- Wagner DM, Chung CH. Transverse growth of the maxilla and mandible in untreated girls with low, average, and high MP-SN angles: a longitudinal study. Am J Orthod Dentofacial Orthop 2005; 128(6):716-23. doi: 10.1016/j.ajodo.2004.09.028 [Crossref] [ Google Scholar]
- Oliveira A, Felinto LT, Francisconi-Dos-Rios LF, Moi GP, Nahsan FPS. Dental bleaching, microabrasion, and resin infiltration: case report of minimally invasive treatment of enamel hypoplasia. Int J Prosthodont 2020; 33(1):105-10. doi: 10.11607/ijp.6232 [Crossref] [ Google Scholar]
- Bezerra-Júnior DM, Silva LM, de Moura Martins L, Cohen-Carneiro F, Pontes DG. Esthetic rehabilitation with tooth bleaching, enamel microabrasion, and direct adhesive restorations. Gen Dent 2016; 64(2):60-4. [ Google Scholar]
- Rizzo NSP, da Cunha LF, Sotelo BV, Gonzaga CC, Correr GM, Gaião U. Esthetic rehabilitation with direct composite resin in a patient with amelogenesis imperfecta: a 2-year follow-up. Case Rep Dent 2019; 2019:8407025. doi: 10.1155/2019/8407025 [Crossref] [ Google Scholar]
- Mirfasihi A, Malek Afzali B, Ebrahimi Zadeh H, Sanjari K, Mir M. Effect of a combination of photodynamic therapy and chitosan on Streptococcus mutans (an in vitro study). J Lasers Med Sci 2020; 11(4):405-10. doi: 10.34172/jlms.2020.64 [Crossref] [ Google Scholar]
- de Oliveira AB, Ferrisse TM, Marques RS, de Annunzio SR, Brighenti FL, Fontana CR. Effect of photodynamic therapy on microorganisms responsible for dental caries: a systematic review and meta-analysis. Int J Mol Sci 2019; 20(14):3585. doi: 10.3390/ijms20143585 [Crossref] [ Google Scholar]
- Sanjari K, Bayani M, Ebrahimi Zadeh H. Conservative dental management of a patient with Epidermolysis bullosa A case report. Pediatr Dent J 2020; 30(3):245-50. doi: 10.1016/j.pdj.2020.06.001 [Crossref] [ Google Scholar]