Avicenna J Dent Res. 14(1):44-46.
doi: 10.34172/ajdr.2022.08
Case Report
Minimum Visit Management of a Localized Anterior Crossbite: A Report of a Dental Emergency Treatment During COVID-19 Pandemic
Majid Mahmoudzadeh 1  , Maryam Salehzadeh 2, *
, Maryam Salehzadeh 2, * 
Author information:
1Associate Professor, Department of Orthodontics, Hamadan University of Medical Sciences, Hamadan, Iran
2Postgraduate Student of Orthodontics, Hamadan University of Medical Sciences, Hamadan, Iran
*
Corresponding author: Maryam Salehzadeh, School of Dentistry, Hamedan University of Medical Sciences, Hamedan, Iran Post Code: 6517838695. Tel:+989123892733, Email:
mm.salehzadeh@gmail.com
Abstract
During the very first months of the pandemic, the importance of deferring elective dental treatment and limiting dental care to cases of true emergency was highlighted by authorities. This paper reports a case of lateral tooth luxation that occurred in a young woman after an epileptic seizure. Adhering to governmental guidelines regarding dental care during the pandemic, we managed this case, requiring minimum chair side and dental visits with a simple mandibular removable plate in 6 weeks.
Keywords: Corrective orthodontics, Subluxation, Emergency care, Coronavirus SARS
Copyright and License Information
© 2022 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Mahmoudzadeh M, Salehzadeh M. Minimum visit management of a localized anterior crossbite: a report of a dental emergency treatment during covid-19 pandemic. Avicenna J Dent Res. 2022; 14(1):44-46. doi:10.34172/ajdr.2022.08
Background
Traumatic dental injury is among frequent dental emergencies and its reported prevalence is about 10% to more than 50%. Both youngsters and adults suffer traumatic injuries. According to many publications, children and adolescents are the major affected groups (1-3), but some surveys reported a higher frequency in adults (4,5). It can vary from a minor, non-diagnosed enamel crack to the most severe form, namely, avulsion.
Tooth luxation is defined as the displacement of a tooth in the alveolus resulting from acute trauma. It can be in the intrusive, extrusive, or lateral direction. The possible pulpal sequel is pulp canal obliteration, necrosis, or physiologic healing. Lateral luxation is the buccolingual displacement of the tooth and may involve alveolar fractures (6). Lateral luxation can cause the crossbite of the interested tooth, and further dental interference and trauma from occlusion can lead to its early loss (7).
Treatment options include manual repositioning with digital pressure or the use of orthodontic forces. An epileptic seizure results from temporary brain dysfunction and is one of the common neurological disorders (8). Oro-facial trauma is common after epileptic attacks, and half of the sufferers have experienced at least one case of oral trauma. Soft tissue injury is more common, but a tooth crack or fracture occurs to a significant percentage (9).
The current paper reports a case of lateral luxation, which occurred after a seizure attack in a young woman. A dental emergency was treated in the COVID-19 pandemic. The orthodontic force corrected the crossbite in 6 weeks.
Case Report
History and Diagnosis
A few months after the onset of the pandemic, a 25-year-old woman attended the Orthodontic Department of Hamadan University of Medical Sciences with the chief complaint of upper central incisor mobility.
She had been diagnosed with epilepsy at age 15 and was on medication (carbamazepine 100 mg) since then to control the situation. Recently, not experiencing seizures, she had escaped some doses of the prescription. She had an attack 1 week prior to her visit. Then, she recognized the more inferior position and increased mobility of the right central incisor.
Grade-3 mobility of that central incisor and lateral luxation of the right lateral mandibular incisor, and a localized crossbite in that region were found upon clinical examinations (Figure 1). Tooth #42 was vital. Radiologic examinations revealed severe root resorption of the upper central incisors (more than half of the root), while no root or alveolar fracture was diagnosed regarding #41 (Figure 2).

Figure 1.
Occlusal and Lateral View of the Subluxated Tooth.
.
Occlusal and Lateral View of the Subluxated Tooth.
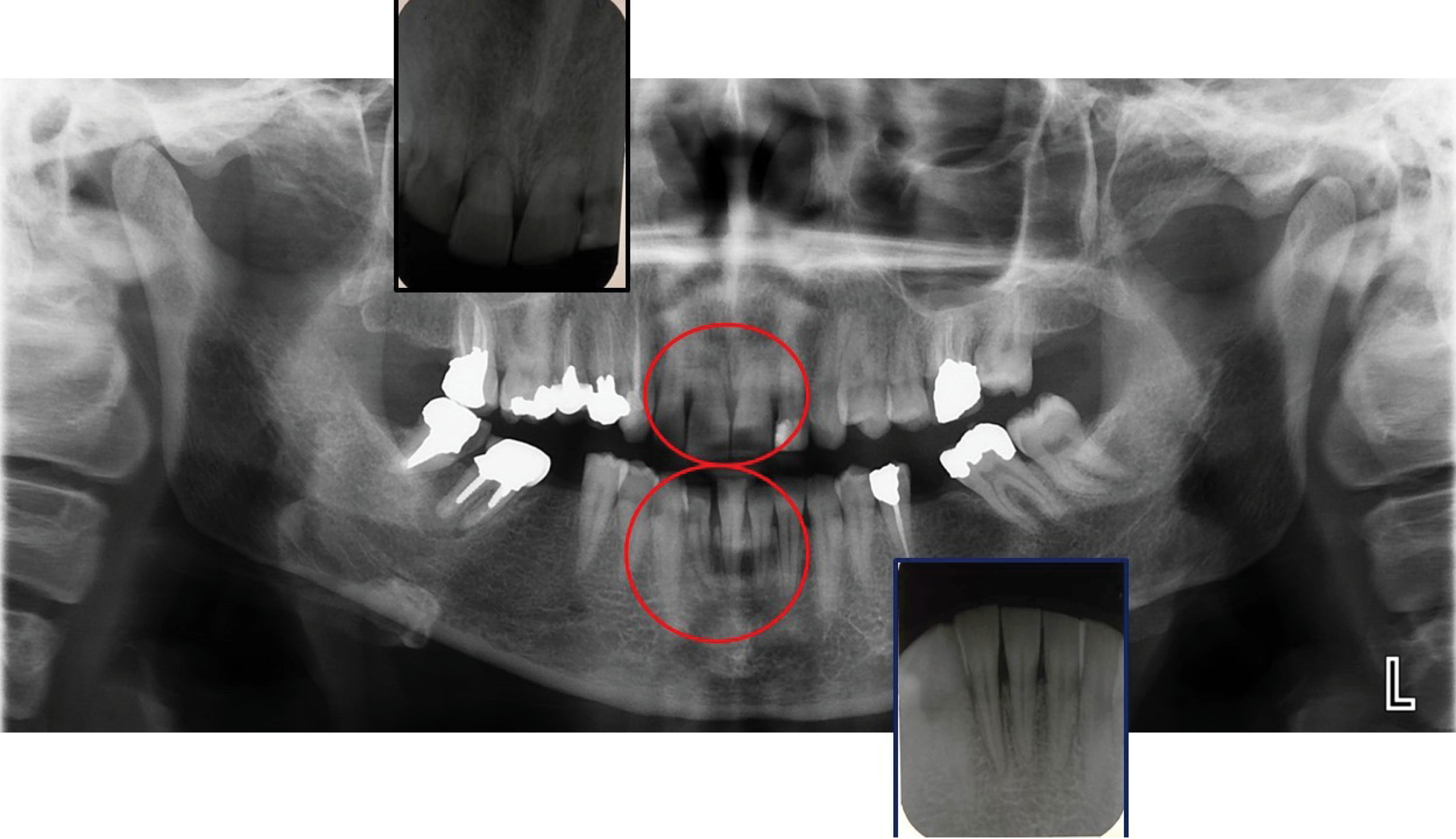
Figure 2.
Panoramic and Peri-apical Views of Interested Regions
.
Panoramic and Peri-apical Views of Interested Regions
She had a class-I dental relationship with normal overjet and overbite. Further, she had pre-extracted both mandibular first molars, and the left third molar had a deep carious lesion. Therefore, the problem list was prepared as follows:
-
Localized anterior crossbite (#42) due to lateral luxation
-
Supra-occlusion and mobility of #11 and #21
Treatment Objective
The primary objective of our treatment was to eliminate the trauma and occlusal interference caused by the crossbite. It was also aimed at adjusting occlusion and improving the prognosis of #11.
Treatment Alternatives
-
For the laterally luxated tooth, we could manually displace the tooth. For this purpose, we had to put a lingually directed pressure on the tooth and stabilize it with orthodontic wire; it could further traumatize the already damaged periodontal apparatus because of the uncontrolled force.
-
Lingually directed orthodontic force could be used to gradually guide the tooth and eliminate the crossbite. In this manner, we could apply light and controlled force permitting simultaneous physiologic healing of the periodontal tissue. Hence, this was our treatment of choice.
For the right central incisor, we consulted with the periodontology department about the prognosis. It had a poor prognosis possibly due to previous traumatic injury, thus we decided to grind the incisal edge to prevent further occlusal trauma and follow that tooth.
Both fixed and removable appliances could apply light-controlled forces. The removable appliance was chosen due to several reasons as follows:
-
The advantage of simultaneously incorporating an acrylic bite in the plate to free the affected tooth of occlusal forces and facilitate the orthodontic movement (10).
-
Less chair time and lesser aerosol production; as this patient was treated during the COVID-19 pandemic, and these issues are considered more important than any other time.
-
Less cost and simplicity
Appliance Design
A mandibular acrylic plate was designed with two Adams clasps on the second molars for retention, a labial bow that delivered the active force and an acrylic bite plate with 3 mm of thickness.
Results
At the delivery session, we adjusted the plate and activated the labial bow by squeezing the vertical loops. We assured the bow position to be lingual to the traumatized teeth and instructed the patient to labially grab the bow to direct lingual force over the tooth.
The patient was referred to a neurology specialist for a complete medical work-up. After 6 weeks, we visited the patient. The tooth was in a normal position with physiologic mobility (Figure 3) and no sign of pulp injury was visible. Finally, she had not experienced attacks during the period.

Figure 3.
Post-treatment Occlusal View.
.
Post-treatment Occlusal View.
Discussion
During the first months of the COVID-19 outbreak, when we faced this patient, elective dental and orthodontic treatment were prohibited by the governmental authorities, and orthodontic treatment was limited to cases where immediate care would prevent further harm to the patient. In this case, the luxated tooth was in continuous occlusal trauma, which was an indication of immediate management. To minimize the risk of viral transmission, we followed all provided guidelines, namely, patient and clinic personnel screening at the entrance, minimum staff, hand hygiene, povidone iodine mouthrinse, and complete personnel protective equipment use.
The recommended treatment for lateral luxation is manual repositioning; however, it risks further damage to the tooth’s supporting structure and is occasionally impossible if there is a delay between the accident and the patient’s visit (6).
Orthodontic extrusion of intrusive luxation injuries is widely practiced in daily treatment, but the use of orthodontic forces for lateral luxation has received less attention.
The physiologic nature of orthodontic forces favors tissue healing, and the light amount of applied forces eliminates sudden uncontrolled force to the affected tooth.
In the reported case in this paper, we could not manually reposition the tooth, therefore, an orthodontic appliance was prescribed to gradually reposition the teeth. It also included a bite plate, which prevented anterior tooth contacts. In addition to facilitating tooth movement, occlusal interference was omitted, helping in healing the periodontal ligament (PDL). When the tooth is guided to its normal position, normal loads contribute to the physiologic reorganization of PDL. Anterior crossbite was corrected in 6 weeks, and minimum chair time and minimum patient visits (2 sessions) were necessary.
Conclusions
Traumatic dental injuries can and do occur in adults and younger ages. Accordingly, it is our professional responsibility to improve our knowledge and skills on different treatment modalities of such cases.
Authors’ Contribution
Both authors contributed equally to the manuscript.
Conflict of Interest Disclosures
The authors declare there is no conflict of interests.
Ethical Statement
Informed consent was obtained from the patient for publication of the report.
References
- Clark D, Levin L. Prognosis and complications of mature teeth after lateral luxation: a systematic review. J Am Dent Assoc 2019; 150(8):649-55. doi: 10.1016/j.adaj.2019.03.001 [Crossref] [ Google Scholar]
- Levin L, Day PF, Hicks L, O’Connell A, Fouad AF, Bourguignon C. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: general introduction. Dent Traumatol 2020; 36(4):309-13. doi: 10.1111/edt.12574 [Crossref] [ Google Scholar]
- Namdev R, Jindal A, Bhargava S, Bakshi L, Verma R, Beniwal D. Awareness of emergency management of dental trauma. Contemp Clin Dent 2014; 5(4):507-13. doi: 10.4103/0976-237x.142820 [Crossref] [ Google Scholar]
- Brunner F, Krastl G, Filippi A. Dental trauma in adults in Switzerland. Dent Traumatol 2009; 25(2):181-4. doi: 10.1111/j.1600-9657.2008.00752.x [Crossref] [ Google Scholar]
- Kaste LM, Gift HC, Bhat M, Swango PA. Prevalence of incisor trauma in persons 6-50 years of age: United States, 1988-1991. J Dent Res 1996; 75 Spec No:696-705. doi: 10.1177/002203459607502s09 [Crossref] [ Google Scholar]
- Spinas E, Pipi L, Mezzena S, Giannetti L. Use of orthodontic methods in the treatment of dental luxations: a scoping review. Dent J (Basel) 2021; 9(2):18. doi: 10.3390/dj9020018 [Crossref] [ Google Scholar]
- Arikan V, Sari S. Using composite resin inclined plane for the repositioning of a laterally luxated primary incisor: a case report. Eur J Dent 2011; 5(1):117-20. [ Google Scholar]
- Gawlak D, Łuniewska J, Stojak W, Hovhannisyan A, Stróżyńska A, Mańka-Malara K. The prevalence of orodental trauma during epileptic seizures in terms of dental treatment - Survey study. Neurol Neurochir Pol 2017; 51(5):361-5. doi: 10.1016/j.pjnns.2017.06.004 [Crossref] [ Google Scholar]
- Nonato ER, Borges MA. Oral and maxillofacial trauma in patients with epilepsy: prospective study based on an outpatient population. Arq Neuropsiquiatr 2011; 69(3):491-5. doi: 10.1590/s0004-282x2011000400016 [Crossref] [ Google Scholar]
- Roy AS, Singh GK, Tandon P, De N. An interim bite raiser. Int J Orthod Milwaukee 2013; 24(2):63-4. [ Google Scholar]