Avicenna J Dent Res. 13(1):38-41.
doi: 10.34172/ajdr.2021.07
Case Report
Dental Management of Peripheral Giant Cell Granuloma in an 8-Year-Old Boy: A Case Report
Arghavan Kamali Sabeti 1, Niloofar Entezari Moghaddam 2, *, Fariba Naderi 2
Author information:
1DDS, Assistant Professor of Pediatric Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran.
2DDS, Postgraduate Student of Pediatric Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran
*
Correspondence to Niloofar Entezari Moghaddam, Tel: 00989123899278, Email:
Niloufal2@gmail.com
Abstract
Peripheral giant cell granuloma (PGCG) or the so-called giant cell epulis is the most common oral giant cell lesion. It normally appears as a soft tissue purple-red nodule. This lesion is certainly not a true neoplasm, but in nature, it may be reactive, thought to be stimulated by local irritation or trauma. Nonetheless, the exact cause is definitely not understood well. In appearance, lesions vary from smooth, uniformly outlined masses to irregularly developed, multilobed surface indentation protuberances. Margin ulcerations are occasionally observed as well. The lesions are painless, differ in size, and can cover many teeth. It may be a lesion on the gingiva or alveolar crest that is sessile or pedunculated, common with respect to the molars and incisors and occurs in reaction to the local response.
Keywords: Giant cell lesion, Multinucleated giant cells, Peripheral giant cell granuloma, Maxilla
Copyright and License Information
© 2021 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Kamali Sabeti A, Entezari Moghaddam N, Naderi F. Dental management of peripheral giant cell granuloma in an 8-year-old boy: a case report. Avicenna J Dent Res. 2021;13(1):38-41. doi: 10.34172/ajdr.2021.07.
Background
Gingival overgrowth seems to be the most common clinical finding, and reactive hyperplasia also represents its link to dental plaque as a consequence of inflammatory gingival disease.
Irritation fibroma (IF), pyogenic granuloma (PG), peripheral ossifying fibroma (POF), and peripheral giant cell granuloma (PGCG) are non-neoplastic.
Gingival enlargements are known as hyperplastic reactive lesions, most of which are of similar clinical appearance.
The PGCG is the most frequently observed giant cell lesion appearing as an extra-osseous purple red soft tissue nodule consisting of multinucleated giant cells in a mononuclear stromal cell background and extravasates red blood cells. This lesion is possibly not present as a true neoplasm but may be reactive in nature (1).
Although it has been assumed that the initiating stimulus was due to local irritation or trauma, the cause is not recognized definitely well. A peripheral giant cell “reparative” granuloma has been labeled, but it has not been proven whether it is truly reparative, and the existence of its osteoclastic activity remains doubtful (2).
PGCG is the widespread overgrowth of gingiva with uncertain pathogenicity. Similar to POF, the occurrence of this lesion is likely to be responsible for local irritants. Histologically, this lesion consists of “edematous, mitotically active, the proliferation of loose connective tissues, and numerous multinuclear giant osteoclast-like cells” (3). There may be additional deposition of hemosiderin with bleeding areas, multiple dilated vessels, chronic inflammatory cell infiltration, and bone formation (3). Oral mucosal overgrowths, particularly PGCG and POF, share histological features with varying amounts of giant cells and focal osteogenesis, including abnormal connective tissue proliferation (4). However, PGCG is composed of relatively more immature and loose components compared to POF.
Case Presentation
An 8-year-old boy complained of a gingival mass in the posterior maxilla. After examination, a steadily expanding gingival mass with a pink surface was observed in the region of unerupted tooth #15. The lesion was first noted a month ago. However, it has recently shown a rise in size, and the parents have not been informed about this problem due to the child’s fear. The parents of the child were highly worried and assumed that the lesion could be a malignant tumor.
The patient had no history of cardiovascular disease, allergies, systemic disorders, surgery, hospitalization, or substance use. The lesion had a fibrous quality, was solid to the touch, and was about 13 mm at its greatest diameter. The lesion was found on the attached gingiva. The patient had relatively poor oral hygiene in the mixed dentition stage (Figure 1). The lymph nodes were fine under palpation. With no clicking sounds, the temporomandibular joint and the mouth opening range were fine. There was no indication of intrabony pathology associated with the soft tissue lesion in the panoramic and periapical radiographs of the patient (Figure 2).

Figure 1.
Clinical Appearance of the Lesion.
.
Clinical Appearance of the Lesion.
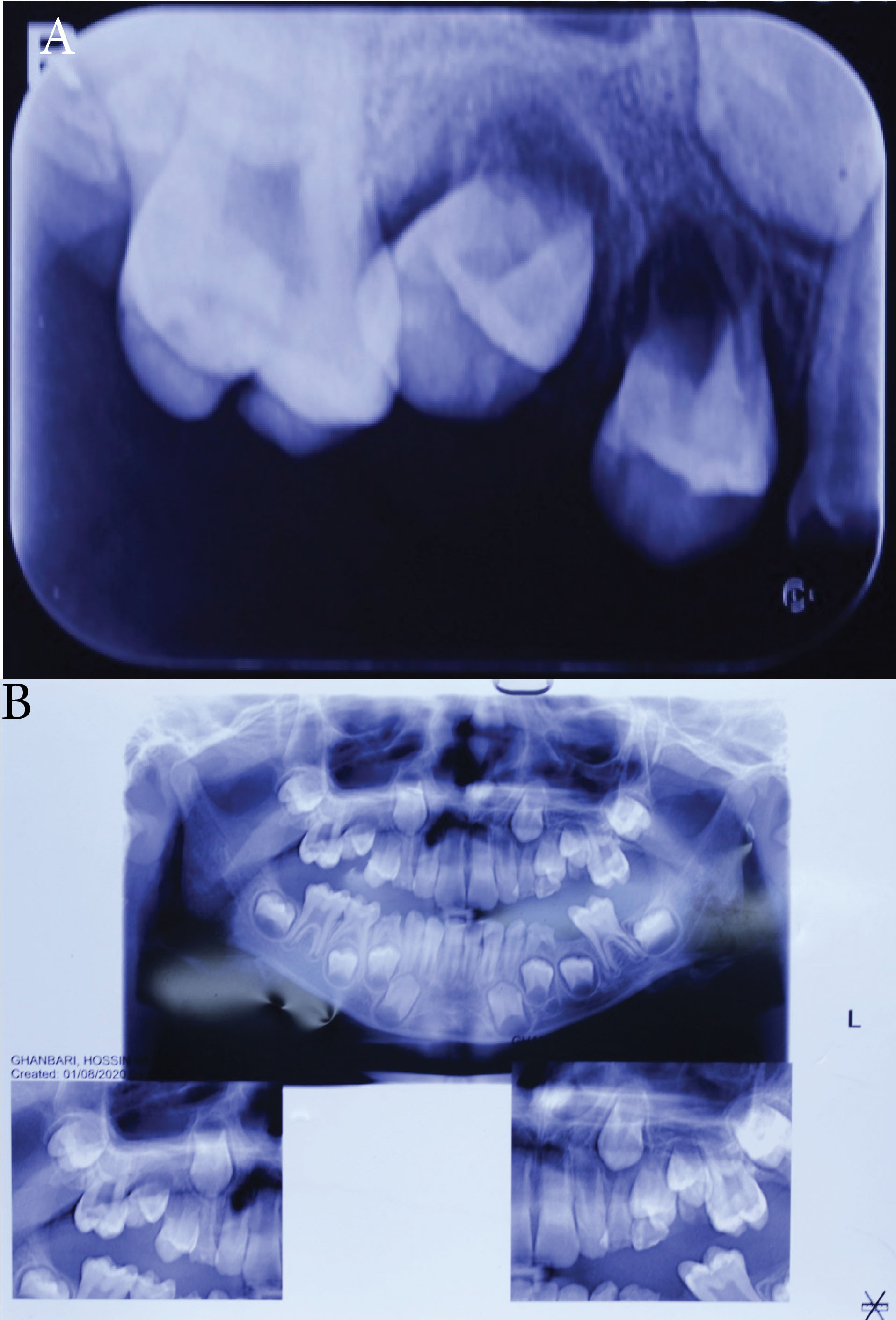
Figure 2.
Periapical (A) and Panoramic (B) Radiographs.
.
Periapical (A) and Panoramic (B) Radiographs.
Differential diagnoses included PGCG, PG, IF, eruption cyst, and POF following a full review. The patient was subjected to an excisional biopsy, and a #15 blade and a surgical spoon-shaped curette were used to cut the lesion down to the periosteum (Figure 3 and Figure 4). Then, the specimen was sent to the pathologist. The microscopic sections showed the squamous epithelium of the oral mucosa. Multinucleated giant cells were detected in the background of spindle-shaped mesenchymal cells, reactive bone formation focal points, and mild to moderate chronic inflammatory cell infiltration. Hemosiderin pigmentation and red blood cell extravasation have also been observed in certain regions. However, no evidence of malignancy was found in this specimen. PGCG was confirmed by the pathological characteristics of the lesion as the final diagnosis for histopathological analysis. Due to poor oral hygiene, the patient underwent regular follow-up although he refused to undergo elective treatment but due to dental phobia (Figures 5 and Figure 6).
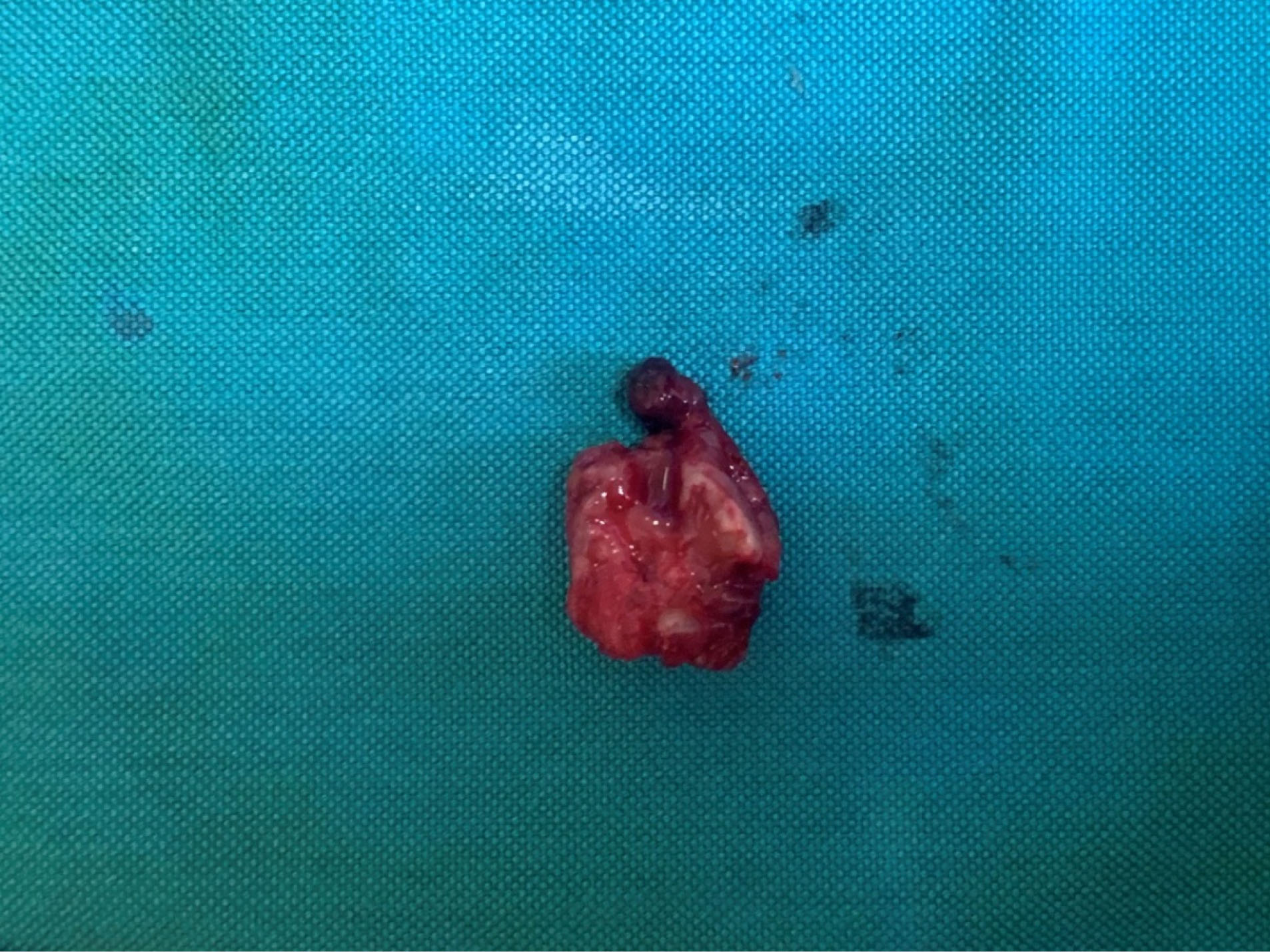
Figure 3.
Excision of Mass.
.
Excision of Mass.
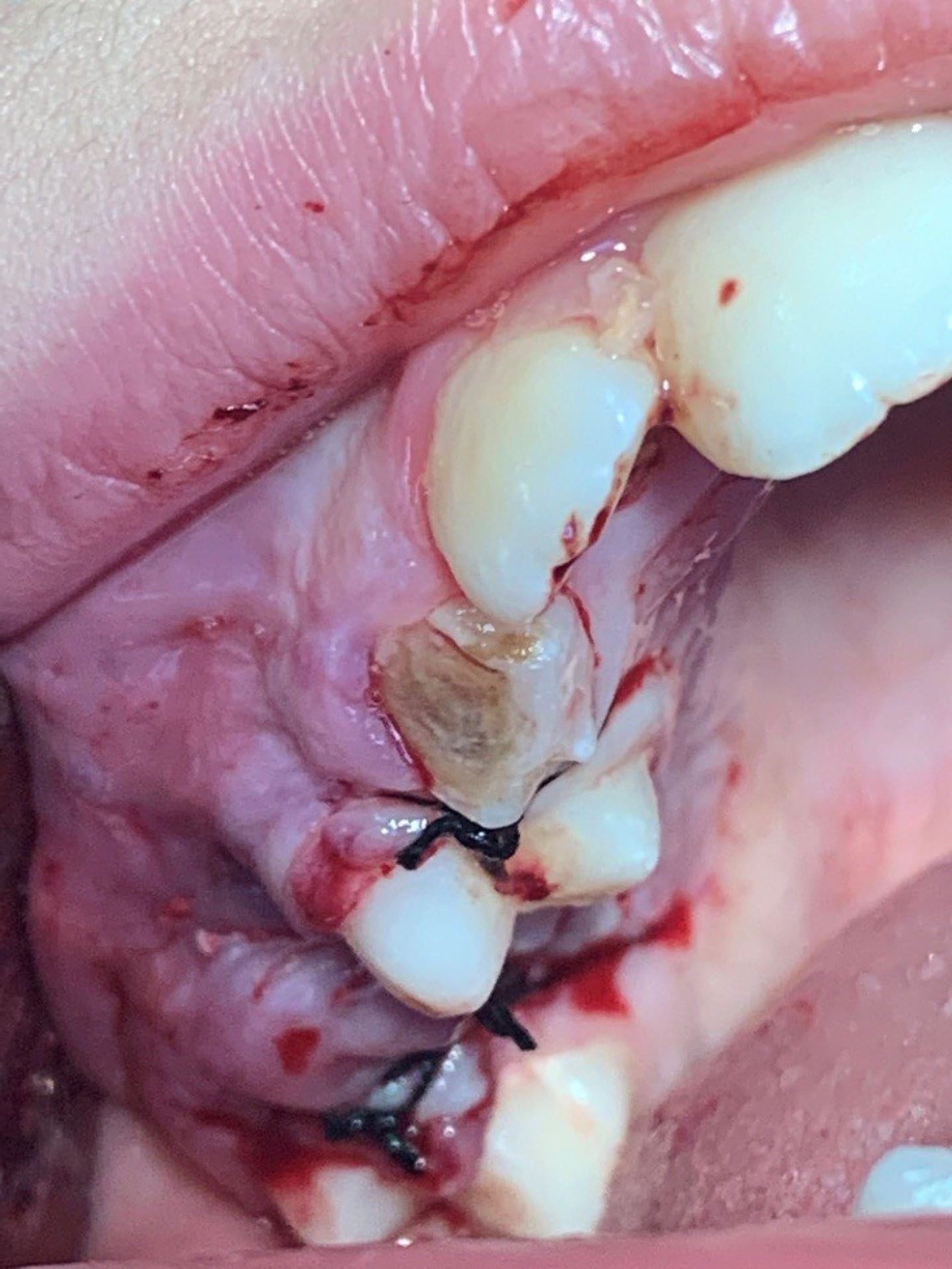
Figure 4.
Immediate Postoperative View.
.
Immediate Postoperative View.

Figure 5.
One Month Follow-up.
.
One Month Follow-up.

Figure 6.
One Year Follow-up: Intraoral View (A) and Periapical Radiograph Showing Root Formation (B).
.
One Year Follow-up: Intraoral View (A) and Periapical Radiograph Showing Root Formation (B).
Discussion
The etiology and composition of giant cell epulis (PGCG) appear to be unclear. Several theories have been previously suggested to clarify the existence of multinucleated giant cells, including the hypothesis that they were osteoclasts left from the physiological resorption of teeth or a reaction to periosteum injury. There is good evidence that these cells are osteoclasts because they have been shown to have calcitonin receptors and have been able to excavate bones in vitro (2).
The PGCG occurs during life, with peaks of incidences during the mixed years of dentition (4) and in the age range of 30-40 years old. In addition, it is more common among women (60%). The mandible is significantly more frequently affected compared to the maxilla (6,7). Lesions may become huge and some may reach the size of 2 cm. The clinical appearance is similar to that of the more prevalent PG. However, the PGCG is often more bluish-purple compared to the bright red of a standard PG. The PGCG associated with dental implants has recently been reported as well (8).
PGCG tends to have a rapid growth rate in children compared to other reactive oral lesions, to be more aggressive with interproximal crest region penetration and bone resorption, to interfere with adjacent teeth eruption, to produce mild to moderate tooth movement, and to have several recurrences (9).
It is clinically distinguished from the fibrous and vascular epulis by PGCG characteristics. It is presented as a firm, smooth, bright pedunculated, or sessile nodule with different sizes varying from small papules to expanded masses although they are typically less than 20 mm in diameter with a color ranging from dark red to purple or blue, usually with an ulcerated surface (9).
Conclusions
For its management, an accurate diagnosis of gingival overgrowth through clinical, radiographic, and histopathological examinations is critical. Care is required because of the rapid growth pattern and the propensity for resorbing the bone with the subsequent movement of the tooth in addition to removing etiological causes, surgical excision of the growth, including its foundation. Finally, a normal post-surgical follow-up is important for preventing growth recurrences.
Conflict of Interest Disclosures
The authors announce that there is no conflict of interests in the publication of this manuscript.
Ethical Statement
The authors published photos of the patient after obtaining his parents consent.
Authors’ Contribution
AK supervised the research. NE and FN performed surgery and co-wrote the paper.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Barrett AW. Oral Oncology. In: Neville BW, Damm DD, Allen CM, Bouquot JE, eds. Oral and Maxillofacial Pathology. WB Saunders Company; 2002.
- Tandon PN, Gupta SK, Gupta DS, Jurel SK, Saraswat A. Peripheral giant cell granuloma. Contemp Clin Dent 2012; 3(Suppl 1):S118-21. doi: 10.4103/0976-237x.95121 [Crossref] [ Google Scholar]
- Salum FG, Yurgel LS, Cherubini K, De Figueiredo MA, Medeiros IC, Nicola FS. Pyogenic granuloma, peripheral giant cell granuloma and peripheral ossifying fibroma: retrospective analysis of 138 cases. Minerva Stomatol 2008; 57(5):227-32. [ Google Scholar]
- Prasad S, Reddy SB, Patil SR, Kalburgi NB, Puranik RS. Peripheral ossifying fibroma and pyogenic granuloma. Are they interrelated? N Y State Dent J 2008; 74(2):50-2. [ Google Scholar]
- Chadwick BL, Crawford PJ, Aldred MJ. Massive giant cell epulis in a child with familial cyclic neutropenia. Br Dent J 1989; 167(8):279-81. doi: 10.1038/sj.bdj.4806999 [Crossref] [ Google Scholar]
- Katsikeris N, Kakarantza-Angelopoulou E, Angelopoulos AP. Peripheral giant cell granuloma Clinicopathologic study of 224 new cases and review of 956 reported cases. Int J Oral Maxillofac Surg 1988; 17(2):94-9. doi: 10.1016/s0901-5027(88)80158-9 [Crossref] [ Google Scholar]
- Giansanti JS, Waldron CA. Peripheral giant cell granuloma: review of 720 cases. J Oral Surg 1969; 27(10):787-91. [ Google Scholar]
- Hirshberg A, Kozlovsky A, Schwartz-Arad D, Mardinger O, Kaplan I. Peripheral giant cell granuloma associated with dental implants. J Periodontol 2003; 74(9):1381-4. doi: 10.1902/jop.2003.74.9.1381 [Crossref] [ Google Scholar]
- Nekouei A, Eshghi A, Jafarnejadi P, Enshaei Z. A review and report of peripheral giant cell granuloma in a 4-year-old child. Case Rep Dent 2016; 2016:7536304. doi: 10.1155/2016/7536304 [Crossref] [ Google Scholar]