Avicenna J Dent Res. 12(4):120-125.
doi: 10.34172/ajdr.2020.24
Original Article
Effects of Low-Level Diode Laser on the Level of Interleukin 1-Beta in the Gingival Crevicular Fluid and the Incidence of Gingivitis Caused by the Use of Orthodontic Separators: A Randomized Clinical Trial
Sepideh Soheilifar 1  , Sara Soheilifar 2, Shayesteh Hatami 3, Farshid Vahdatinia 4, Vahid Molabashi 5, Mehrdad Hajiloui 6, Pouria Teymouri 7, *
, Sara Soheilifar 2, Shayesteh Hatami 3, Farshid Vahdatinia 4, Vahid Molabashi 5, Mehrdad Hajiloui 6, Pouria Teymouri 7, * 
Author information:
1Assistant Professor, Department of Orthodontics, Implant Research Center, Hamedan University of Medical Sciences, Hamadan, Iran.
2Periodontist, Private Office.
3General dentist, Kermanshah, Iran.
4General Dentist, Dental Implants Research Center, Dental School, Hamadan University of Medical Sciences, Hamadan, Iran.
5Associate Professor of Orthodontic Department, Dental School, Hamadan University of Medical Sciences, Hamadan, Iran.
6Department of Immunology, School of Medicine, Hamedan University of Medical Science, Hamedan, Iran.
7General Dentist, Resident of Oral and Maxillofacial Surgery, Hamadan University of Medical Sciences, Hamadan, Iran.
Abstract
Background: In recent years, there has been an increased tendency for using dental lasers for the treatment of soft tissue problems. The aim of this study was to evaluate the effect of low-level diode laser (980 nm) on the level of interleukin 1 beta (IL-1β) in the gingival crevicular fluid (GCF) and the incidence of initial gingivitis caused by the use of orthodontic separators.
Methods: In this randomized clinical trial, 30 patients, who were beginning a fixed orthodontic treatment without gingivitis, were randomly assigned to control and diode laser radiation (980 nm wavelength, 3 J of energy, a density of 3 J/cm2, a power of 0.2 W, and at a distance of 1 cm away from the tissue for 15 seconds on the buccal and palatal sides of the tooth) groups. The gingival index (GI) and bleeding on probing (BOP) were measured at the beginning of the study and one week after the treatment. The level of IL-1β was evaluated using an enzyme-linked immunosorbent assay at the beginning of the study and one week after the placement of the separator. Finally, the inter-group and intra-group statistical analyses were performed using independent and paired t tests, and P<0.05 was considered as the significance level.
Results: The evaluation of clinical variables in the entire mouth showed a slight clinical improvement in the experimental group although there was no significant difference between the two groups. No significant difference was observed between intra-group and inter-group evaluations of clinical indices in the studied specific teeth. Eventually, no difference was found between the two groups in terms of IL-1β changes.
Conclusions: In general, the single-diode laser radiation session is not effective in the treatment of gingivitis in patients undergoing orthodontic treatment. Thus, it is recommended to perform frequent laser radiation sessions in further studies.
Keywords: Laser, Gingivitis, Orthodontic devices, Proinflammatory cytokines, Interleukin 1 β, Separator
Copyright and License Information
© 2020 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Soheilifar S, Soheilifar S, Vahdatinia F, Hatami S Molabashi V, Hajiloui M, Teymouri P. Effects of low-level diode laser on the level of interleukin 1-beta in the gingival crevicular fluid and the incidence of gingivitis caused by the use of orthodontic separators: a randomized clinical trial. Avicenna J Dent Res. 2020;12(4):120-125. doi: 10.34172/ ajdr.2020.24.
Background
Highlights
-
Gingival inflammation is a usual problem in fixed orthodontics.
-
Low-level laser therapy has been introduced to reduce the rate of inflammation.
-
Single-diode laser radiation session is not effective for the treatment of gingivitis in patients undergoing orthodontic treatment.
-
It is recommended to perform frequent laser radiation sessions in further studies.
inflammation is a common occurrence in orthodontic treatment to the use of mechanical forces for tooth displacement. Blood flow changes in periodontal tissues after applying mechanical forces during orthodontic treatments, ultimately leading to inflammation in these tissues. After the onset of these inflammations, mediators such as histamines, enkephalins, dopamines, serotonins, prostaglandin E2 (PGE2), and leukotrienes are released, thus leading to hyperalgesia to pain (1-7). One of the causes of inflammation is the accumulation of food debris that can be due to gingivitis (8). The first manifestation of gingivitis is observed in the form of vascular changes, including the expansion of the capillaries and increased blood flow. These changes occur in response to the microbial stimulation of resident cells, followed by the stimulation of endothelial cells. This stage of gingivitis is called an initial lesion (9). The existence of an orthodontic elastomeric separator can cause gingivitis as an initial lesion. Food stuck between teeth, water absorption, the gap between teeth and the disuse of dental floss can be considered as the causes of gingivitis in these patients (10). In their study, Giannopoulou et al found that the placement of an elastomeric separator could increase the inflammatory cytokines of interleukin 1beta (IL-1β), substance P, and PGE2 in the gingival crevicular fluid (GCF) from 1 hour to 7 days later (11). It is recommended to improve plaque control methods through the use of practices such as electric toothbrushes, use of ozonated irrigation water, and mouthwashes such as chlorhexidine and various interdental cleansing aids in order to prevent gingivitis during the orthodontic treatment. The patient’s lack of cooperation leads to the failure of the above-mentioned methods in some patients (12-15). Among the available methods, some researchers suggested using low-level laser therapy to reduce the rate of inflammation (16). Low-level lasers affect the activity of bone cells, and previous research reported an increase in superficial osteoblastic cells and osteoid thickness in the irradiated region (17). Therefore, this study aimed to investigate the effect of low-level laser radiation (980 nm diode) on the level of IL-1β in the gingival sulcus and initial gingivitis caused by the use of orthodontic separators.
Materials and Methods
The current split-mouth double-blind randomized clinical trial study was performed in the Dentistry Faculty, Hamedan during 2016-2017 after being registered at the Iranian Center for Clinical Trials with the code of IRCT2017011620523N2. Considering the specified inclusion and exclusion criteria, specimens were randomly selected from fixed orthodontic patients aged 18-30 years old and an elastomeric separator was placed (Table 1). After explaining the study procedure and obtaining informed consent from the patients, a trained person recorded the buccal gingival condition of the first maxillary molar and later recorded the gingival condition based on the gingival index (GI) and bleeding on probing (BOP).
Table 1.
Inclusion and Exclusion Criteria of the Study
|
Inclusion Criteria
|
Exclusion Criteria
|
| The patient’s informed consent to enter the study |
Coagulation disorders, autoimmune diseases, and acute and chronic infections based on the patient’s medical history |
| The absence of active periodontal disease (probe depth less than 4 mm and the absence of BOP in maxillary first molar) |
Patients undergoing immunosuppressive treatments, radiation therapy, and antibiotic therapy |
| Lack of a systemic disease |
Patients treated with corticosteroids and nonsteroidal anti-inflammatory drugs |
| The presence of maxillary first molars and having a firm contact with the adjoining teeth |
Pregnant women and smokers |
| Patients with an index plaque less than 30% |
Patients undergoing periodontal therapy and continuous intake of chlorhexidine mouthwash |
Note. BOP: Bleeding on probing.
Then, the plaque was removed and the region was isolated with a cotton roll on each side of the maxillary arch. To collect the GCF, Meta Biomed Sterile paper points (30 mm, Korea) were placed in the gingival sulcus. The paper point was guided until feeling resistance in the gingival sulcus and then remained in the above site for 30 seconds. They were immediately placed in 1.5 cc microtubes containing phosphate buffer saline and transferred to the laboratory within 1 hour at -40 °C. Next, elastomeric separators (Dentaurum, Germany) were placed between the mesial and distal surfaces of the maxillary first molar using the forceps separator and without causing a trauma in such a way that one side of the separator was more gingival than the contact area and the other side was more occlusal compared to the contact area. Then, one side of the patient was placed in the laser group and the other side in the control group using the simple random sampling method and based on the numbers in the Opaque pocket. It should be noted that patients were unaware of the side that was supposed to undergo laser radiation.
Laser Group
The laser diode radiation was performed on the buccal and palatal sides at a wavelength of 980 nm, 3 J, the density of 3 J, power of 0.2 W, and 1 cm away from the gum tissue for 15 seconds (laser tip diameter of 1 cm). Eye protection glasses were given to the patient and the operator during radiation therapy, and the radiation was performed in a closed room.
Control Group
The control group received the placebo irradiation in the buccal and palatal surfaces for 15 seconds in such a way that it did not differ from the laser group except for turning off the laser light. The patient referred a week later to remove the separator and continue the orthodontic treatment. GI and BOP were measured and GCF was collected again. The patients were requested to immediately refer for the replacement of the separator if it was displaced during the week. In case of non-referral, the patient was removed from the specimens. GI and BOP were calculated by the same person who performed the measurements at the beginning of the study.
To measure GI, one number was assigned to the gingivitis of each tooth, including0, 1, 2, and 3 denoting a complete absence of the inflammation signs, a slight change in the color of the superficial tissue, inflammation visibility, and the risk of BOP, respectively. In addition, number 3 referred to severe gingivitis and a tendency to spontaneous bleeding. It should be noted that numbers were recorded for each side.
To measure the BOP, a periodontal probe of 1 mm should be placed in the facial and lingual sulcus and it should be moved from the distal to the mesial side. After probing each quadrant, the presence or absence of BOP was investigated in the above-mentioned sites.
Measuring the Level of IL Inflammatory Factor
Considering that the evaluator was unaware of patient grouping, the inflammatory factor levels of IL were measured by enzyme-linked immunosorbent assay.
The frequency of numbers was calculated in the two groups in the previous and next steps in terms of BOP and GI status, and the chi-square test was used to calculate the difference between the two groups in the previous and next steps. The P < 0.05 was considered as the significance level.
Results
The current study was performed on 37 patients. Of these, 3, 2, and 2 patients were excluded due to removal of the separator, periodontal inflammation, and the lack of attending the laser radiation session, respectively.
Figure 1 displays patients’ demographic information. This research was conducted on 17 women and 13 men with an average age of 22.8 years old.
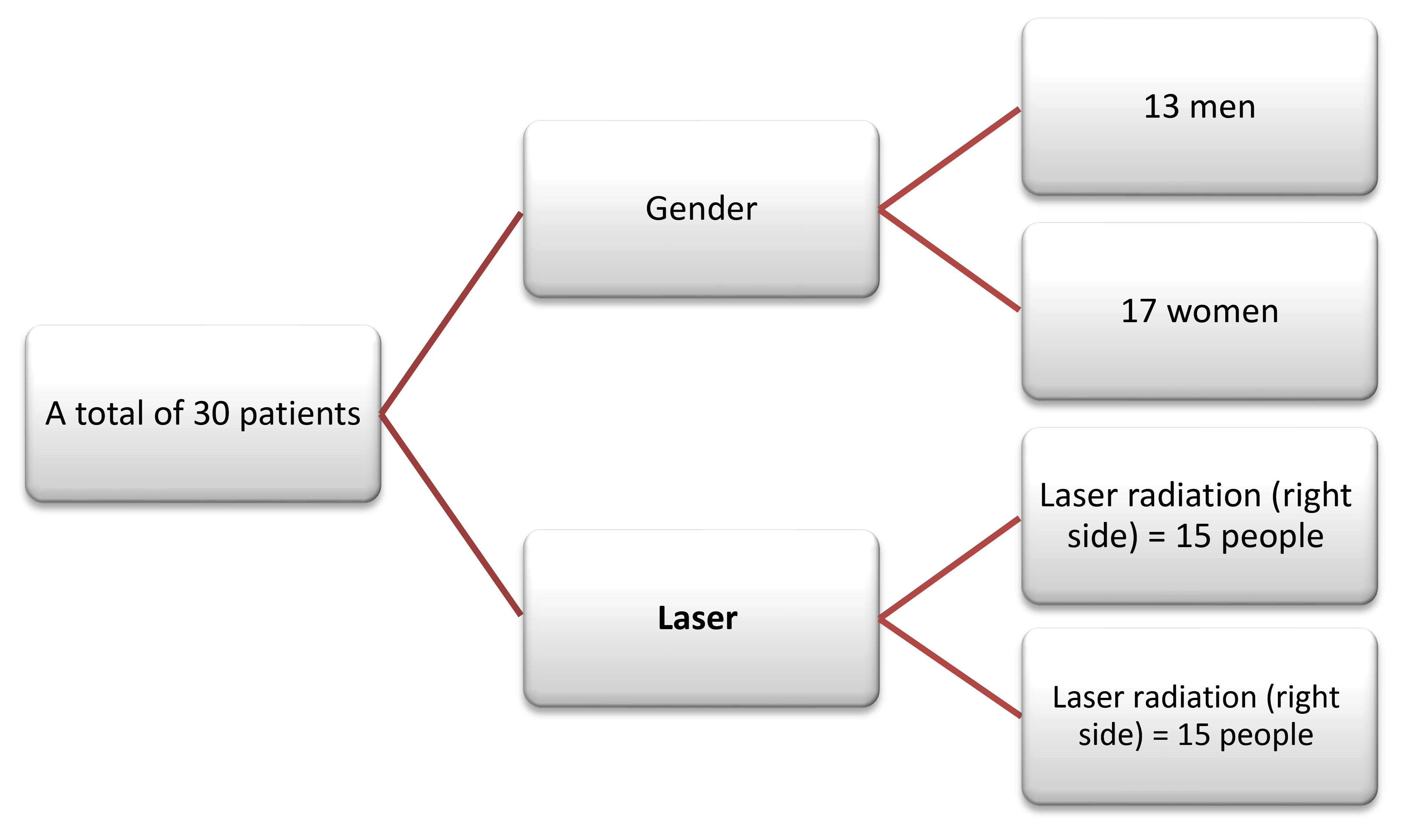
Figure 1.
Demographic Information of Patients.
.
Demographic Information of Patients.
Table 2 presents the results of the Chi-square test on the gingival condition before and after radiation in the two groups based on GI.
Table 2.
GI-Based Comparison of the Inflammation Rate in the 2 Groups Before and 1 Week After the Placement of a Separator Using the Chi-square Test
|
|
|
Laser
|
Non-laser
|
Results of Chi-square Test
|
|
Number
|
%
|
Number
|
%
|
| The inflammation rate before the placement of the separator |
No inflammation (0) |
23 |
76.7 |
22 |
73.3 |
χ2=0.099
df =2
P value = 0.952 |
| At the gum level (1) |
6 |
20.0 |
7 |
23.3 |
| Evident inflammation (2) |
1 |
3.3 |
1 |
3.3 |
| Severe inflammation |
0 |
0 |
0 |
0 |
| The inflammation rate after the placement of the separator |
No inflammation |
20 |
66.7 |
18 |
60.0 |
χ2= 1.15
df = 2
P value = 0.562 |
| At the gum level |
10 |
33.3 |
11 |
36.7 |
| Evident inflammation |
0 |
0 |
1 |
3.3 |
| Severe inflammation |
0 |
0 |
0 |
0 |
Note. GI: Gingival index.
The results of the chi-square test on BOP before and after radiation in the 2 groups are provided in Table 3.
Table 3.
Comparison of BOP in the 2 Groups Before and 1 Week After the Placement of the Separator Using the Chi-square Test
|
|
|
Laser
|
Non-laser
|
Results of Chi-square Test
|
|
Number
|
%
|
Number
|
%
|
| BOP before the placement of the separator |
No |
29 |
96.6 |
28 |
93.3 |
χ2=0.0000
df = 1
P value = 1.000 |
| Yes |
1 |
3.3 |
2 |
6.66 |
| BOP after the placement of the separator |
No |
30 |
100 |
29 |
96.6 |
χ2= 2.07
df = 1
P value = 0.150 |
| Yes |
0 |
0 |
1 |
3.3 |
Note. BOP: Bleeding on probing.
Table 4 summarizes the mean GCF volume collected in the 2 groups within 1 week and the results of the paired t test. Based on the results, the GCF volume has changed in both groups although the difference was not statistically significant in any of the 2 groups.
Table 4.
Comparison of the Mean GCF Volume Collected in the 2 Groups Before and 1 Week After the Placement of the Separator Using Paired T test
|
Collected GCF
|
Mean ± SD Before Laser Radiation
|
Mean ± SD After Laser Radiation
|
P
value
|
| Experimental group |
0.0±09.11 |
0.0± 78.053 |
0.334 |
| Control group |
0.0±06.03 |
0.0± 95.10 |
0.227 |
Note. GCF: Gingival crevicular fluid; SD: Standard deviation.
Table 5 lists the mean IL level of the GCF in the two groups within one week and the results of the paired t test.
According to the obtained data, the IL-1β content of the GCF decreased slightly in the control group while increasing in the experimental group after a week. However, these changes were not statistically significant in the two groups. There was no significant difference between the two groups in terms of GCF volume changes in two stages (mean difference: 0.048, P > 0.834). Further, no significant difference was found between the two groups regarding IL-1β changes in two stages (mean difference: 3.83, P < 0.748). Eventually, no significant difference was observed between the two groups in terms of IL-1β changes (IL-1β/volume of collected GCF collected, mean change: 0.1, P < 0.629).
Table 5.
Comparison of the Mean IL-1β Collected in the 2 Groups Before and 1 Week After the Placement of the Separator Using the Paired t test
|
Level of IL-1β
|
Mean ± SD Before Laser Radiation
|
Mean ± SD After Laser Radiation
|
P
value
|
| Experimental group |
18.13 ± 56.7 |
17.15 ± 47.96 |
0.764 |
| Control group |
15.11 ± 82.46 |
18.15 ± 56.85 |
0.467 |
Note. IL-1β: Interleukin-1beta; SD: standard deviation.
Discussion
The results of this study showed no significant difference between the two groups in terms of the evaluation of the clinical indices of the mouth. There were no changes in the clinical variables in both groups after one week. Based on the assessment of the studied specific teeth, BOP and GI did not show any significant changes in either of the two experimental and control groups, and there was no significant difference between the two groups although GI changes improved in the experimental group. Moreover, no significant intergroup changes were observed in these teeth, which is in line with the results of Dudic et al and Giannopoulou et al (11,18) Dudic et al placed one separator in the mesial region of the molar teeth and the opposite molar was selected as the control. Giannopoulou et al also placed one separator in the mesial and distal roots of the molar on one side, and the other molar was selected as the control. In other words, there was no significant difference between the experimental and control groups of the present study and the two above mentioned studies in terms of the clinical status of periodontal structures one week after the placement of the orthodontist separator. However, GI represented a continuous increase of 4 weeks in the study by Johnson et al (19) In addition to creating a mechanical barrier to adherence to oral hygiene, all oral hygiene practices including brushing and flossing were stopped in this study. Furthermore, the mechanical barrier covered several teeth in the form of a buccal shield. The differences in the development of gingivitis and hygiene practices can be the reason for the difference between the two studies. Moreover, Zhang et al concluded that there were no changes in the clinical appearance of gums despite changes in the biomarkers 3 days without oral hygiene (10).
In this study, the amount of the collected GCF and the IL-1β in the GCF did not change significantly in the control group within 7 days. Pro-inflammatory cytokines are often produced by active macrophages and interact with the upregulation of inflammatory reactions. Specific proximal cytokines such as IL-1β, IL-6, and tumor necrosis factor-α (TNF-α) have been shown to play a role in pathologic pain (10). In addition, it has been found that IL-1β can be involved in the onset of bone remodeling during orthodontic tooth movements by activating osteoclasts or secreting PGE2 (11). No change was observed in the IL-1β of the control group of the present study, which is inconsistent with the results of studies conducted by Dudic et al and Giannopoulou et al (11,18). Based on the findings of Dudic et al, the level of IL-1β, PGE2) continuously demonstrated a significant increase from 1 minute after the placement of the separator up to 1 week later (18). The findings of Giannopoulou et al revealed that IL-1β levels increased during the first 24 hours although somewhat decreased until the 7th day (11). This finding could justify the results of the present study because the level of IL was measured before the placement of the separator and after 1 week in this study. According to Giannopoulou et al, the lack of a significant decrease in the level of abovementioned IL does not necessarily indicate a change in the level of this substance within one week (11). Additionally, Dudic et al believed that considering the healthy clinical appearance of gums and the time-consuming nature of the cytokine production process, immediate changes in the cytokines level can be partly due to an immediate and increasing rise in the GCF volume (18). Samuaels et al, and Last et al reported a significant increase in the GCF volume during the orthodontic treatment due to inflammation and dental movements (20,21). However, the results of the present study, similar to those of Uematso et al, showed no significant change in the GCF volume, which could be one of the reasons for the lack of changes in the level of IL-1β in the gingival sulcus. The lack of any change in the level of IL-1β in the above-mentioned study, which was performed on patients undergoing fixed orthodontic treatment, highlights the role of the GCF volume in the IL-1β level (22).The contradictory results on GCF changes in various studies can be due to differences in the applied methods for measuring the level of the collected GCF.
There are two general methods for GCF collection including suction and absorption. The suction method can cause trauma and changes in the absorbed volume. The absorption method is a simpler and less invasive method and is more widely used accordingly. This method is performed using various tools. The standard method is to use a Periopaper adsorbent to absorb a liquid and Periotron device in order to measure the absorbed volume (23). In the present study, the paper cone was used instead of Periopaper to absorb GCF and to calculate the GCF volume later. In this study, the volume of the collected GCF and the IL-1β of GCF did not change significantly during the 7 days. In addition, there was no significant difference between both experimental and control groups in terms of changes in IL-1β levels. These results contradict those of Löe et al, Safavi et al and Teymouri et al (8,24,25) Safavi et al studied the effect of a low-level helium-neon laser on the expression of IL-1β, TNF-α, interferon-α, TGF-B, and basic fibroblast growth factor genes of rat gums. In this article, the low-level laser was able to suppress the expression of the inflammatory cytokine gene and reduce the amount of swelling, inflammation, and the time for wound healing (24). The differences observed in the type of the laser (diode vs. helium-neon), the frequency of radiation (1 dose vs. 2-3 doses), the method of cytokine analysis (examination of the cytokine in the gingival sulcus vs. examination of the gene expression), the nature of inflammation (inflammation induced by the orthodontic forces vs. inflammation caused by gum cutting) and the type of specimen (human vs. rat) can cause such a difference.
One of the strengths of the present study is its triple-blind design, meaning that the patient, the statistical analyst, and the individual performing the measurements were unaware of the patients’ grouping. This design has a significant impact on reducing the bias in measurements and result evaluation. The split-mouth design of the study, along with considering one mouth side as a control eliminates interpersonal differences in the results.
Conclusions
Based on the findings of the current study, the separator does not necessarily lead to increased gingivitis and inflammatory biomarkers in the first week. Additionally, taking into account the limitations of the present study, the radiation of a single low-level dose laser had no effect on the inflammation status and the studied biomarkers after using the separator.
Conflict of Interest Disclosures
There is no conflict of interests.
Ethical Statement
All the patients and their representative authorities signed the informed consent form. This study follows the Declaration of Helsinki on medical protocols and ethics. The Research and Medical Ethics Committee of Hamedan University of Medical Sciences approved the study protocol with the code of IR.UMSHA.REC.1395.461.
Authors’ Contribution
SS: Conceptualization, Methodology; SS: Conceptualization, Project administrationl; SH: Data Curation, Investigation; FV: Writing - original draft;VM: Conceptualization, Methodology; MH: Data Curation, Laboratory testing; PT: Validation, Writing- editing draft.
Funding
this study was funded by Hamadan University of Medical Sciences
References
- Acharya S, Goyal A, Utreja AK, Mohanty U. Effect of three different motivational techniques on oral hygiene and gingival health of patients undergoing multibracketed orthodontics. Angle Orthod 2011; 81(5):884-8. doi: 10.2319/112210-680.1 [Crossref] [ Google Scholar]
- Alfuriji S, Alhazmi N, Alhamlan N, Al-Ehaideb A, Alruwaithi M, Alkatheeri N. The effect of orthodontic therapy on periodontal health: a review of the literature. Int J Dent 2014; 2014:585048. doi: 10.1155/2014/585048 [Crossref] [ Google Scholar]
- Bollen AM, Cunha-Cruz J, Bakko DW, Huang GJ, Hujoel PP. The effects of orthodontic therapy on periodontal health: a systematic review of controlled evidence. J Am Dent Assoc 2008; 139(4):413-22. doi: 10.14219/jada.archive.2008.0184 [Crossref] [ Google Scholar]
- Ize-Iyamu IN, Saheeb BD, Edetanlen BE. Comparing the 810nm diode laser with conventional surgery in orthodontic soft tissue procedures. Ghana Med J 2013; 47(3):107-11. [ Google Scholar]
- Eid HA, Assiri HA, Kandyala R, Togoo RA, Turakhia VS. Gingival enlargement in different age groups during fixed orthodontic treatment. J Int Oral Health 2014; 6(1):1-4. [ Google Scholar]
- Stanfeld J, Jones J, Laster L, Davidovitch Z. Biochemical aspects of orthodontic tooth movement I Cyclic nucleotide and prostaglandin concentrations in tissues surrounding orthodontically treated teeth in vivo. Am J Orthod Dentofacial Orthop 1986; 90(2):139-48. doi: 10.1016/0889-5406(86)90046-6 [Crossref] [ Google Scholar]
- Vandevska-Radunovic V. Neural modulation of inflammatory reactions in dental tissues incident to orthodontic tooth movement A review of the literature. Eur J Orthod 1999; 21(3):231-47. doi: 10.1093/ejo/21.3.231 [Crossref] [ Google Scholar]
- Löe H, Theilade E, Jensen SB. Experimental gingivitis in man. J Periodontol 1965; 36(3):177-87. doi: 10.1902/jop.1965.36.3.177 [Crossref] [ Google Scholar]
- Lindhe J, Hamp S, Löe H. Experimental periodontitis in the beagle dog. J Periodontal Res 1973; 8(1):1-10. doi: 10.1111/j.1600-0765.1973.tb00735.x [Crossref] [ Google Scholar]
- Zhang J, Kashket S, Lingström P. Evidence for the early onset of gingival inflammation following short-term plaque accumulation. J Clin Periodontol 2002; 29(12):1082-5. doi: 10.1034/j.1600-051x.2002.291206.x [Crossref] [ Google Scholar]
- Giannopoulou C, Dudic A, Kiliaridis S. Pain discomfort and crevicular fluid changes induced by orthodontic elastic separators in children. J Pain 2006; 7(5):367-76. doi: 10.1016/j.jpain.2005.12.008 [Crossref] [ Google Scholar]
- Dhingra K, Vandana KL. Management of gingival inflammation in orthodontic patients with ozonated water irrigation--a pilot study. Int J Dent Hyg 2011; 9(4):296-302. doi: 10.1111/j.1601-5037.2011.00506.x [Crossref] [ Google Scholar]
- Hohoff A, Stamm T, Kühne N, Wiechmann D, Haufe S, Lippold C. Effects of a mechanical interdental cleaning device on oral hygiene in patients with lingual brackets. Angle Orthod 2003; 73(5):579-87. doi: 10.1043/0003-3219(2003)073<0579:eoamic>2.0.co;2. [Crossref] [ Google Scholar]
- Kossack C, Jost-Brinkmann PG. Plaque and gingivitis reduction in patients undergoing orthodontic treatment with fixed appliances-comparison of toothbrushes and interdental cleaning aids A 6-month clinical single-blind trial. J Orofac Orthop 2005; 66(1):20-38. doi: 10.1007/s00056-005-0344-4 [Crossref] [ Google Scholar]
- Borutta A, Pala E, Fischer T. Effectiveness of a powered toothbrush compared with a manual toothbrush for orthodontic patients with fixed appliances. J Clin Dent 2002; 13(4):131-7. [ Google Scholar]
- Mizutani K, Musya Y, Wakae K, Kobayashi T, Tobe M, Taira K. A clinical study on serum prostaglandin E2 with low-level laser therapy. Photomed Laser Surg 2004; 22(6):537-9. doi: 10.1089/pho.2004.22.537 [Crossref] [ Google Scholar]
- Cruz DR, Kohara EK, Ribeiro MS, Wetter NU. Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: a preliminary study. Lasers Surg Med 2004; 35(2):117-20. doi: 10.1002/lsm.20076 [Crossref] [ Google Scholar]
- Dudic A, Kiliaridis S, Mombelli A, Giannopoulou C. Composition changes in gingival crevicular fluid during orthodontic tooth movement: comparisons between tension and compression sides. Eur J Oral Sci 2006; 114(5):416-422. doi: 10.1111/j.1600-0722.2006.00387.x [Crossref] [ Google Scholar]
- Johnson TC, Reinhardt RA, Payne JB, Dyer JK, Patil KD. Experimental gingivitis in periodontitis-susceptible subjects. J Clin Periodontol 1997; 24(9 Pt 1):618-625. doi: 10.1111/j.1600-051x.1997.tb00238.x [Crossref] [ Google Scholar]
- Samuels RH, Pender N, Last KS. The effects of orthodontic tooth movement on the glycosaminoglycan components of gingival crevicular fluid. J Clin Periodontol 1993; 20(5):371-377. doi: 10.1111/j.1600-051x.1993.tb00375.x [Crossref] [ Google Scholar]
- Last KS, Stanbury JB, Embery G. Glycosaminoglycans in human gingival crevicular fluid as indicators of active periodontal disease. Arch Oral Biol 1985; 30(3):275-281. doi: 10.1016/0003-9969(85)90045-7 [Crossref] [ Google Scholar]
- Uematsu S, Mogi M, Deguchi T. Interleukin (IL)-1 beta, IL-6, tumor necrosis factor-alpha, epidermal growth factor, and beta 2-microglobulin levels are elevated in gingival crevicular fluid during human orthodontic tooth movement. J Dent Res 1996; 75(1):562-567. doi: 10.1177/00220345960750010801 [Crossref] [ Google Scholar]
- de Alencar FG Silva, Gomes SC. Validation of an alternative absorbent paper for collecting gingival crevicular fluid. R Periodontia 2009; 19(3):85-90. [ Google Scholar]
- Safavi SM, Kazemi B, Esmaeili M, Fallah A, Modarresi A, Mir M. Effects of low-level He-Ne laser irradiation on the gene expression of IL-1beta, TNF-alpha, IFN-gamma, TGF-beta, bFGF, and PDGF in rat’s gingiva. Lasers Med Sci 2008; 23(3):331-335. doi: 10.1007/s10103-007-0491-5 [Crossref] [ Google Scholar]
- Teymouri F, Farhad SZ, Golestaneh H. The Effect of Photodynamic Therapy and Diode Laser as Adjunctive Periodontal Therapy on the Inflammatory Mediators Levels in Gingival Crevicular Fluid and Clinical Periodontal Status. J Dent (Shiraz) 2016; 17(3):226-232. [ Google Scholar]