Avicenna J Dent Res. 12(4):112-119.
doi: 10.34172/ajdr.2020.23
Original Article
Effectiveness of Preoperative Chlorhexidine Mouthwash on Pain After Lower Posterior Teeth Removal: A Randomized, Double-Blind Clinical Trial
Abbas Haghighat 1  , Shaqayeq Ramezanzade 2, *
, Shaqayeq Ramezanzade 2, * 
Author information:
1Associate Professor, School of Dentistry, Isfahan University of Medical Science, Isfahan, Iran.
2Private Dental Practice, Tehran, Iran.
Abstract
Background: Pain is one of the most common complications after tooth extraction and pain control is a crucial part of the procedure. The purpose of this study was to investigate the influence of 0.2% (w/v) chlorhexidine (CHX) gluconate mouth rinse on the severity of post-extraction pain.
Methods: A prospective, randomized, double-blind trial was conducted among 170 subjects. Subjects were instructed to rinse with 15 mL of CHX mouth rinse (study group) or placebo (control group) 0.5 to 1 hour before extraction. Post-operative pain was evaluated considering the number of taken rescue analgesics and using a visual analog scale (VAS) that each case completed 6, 12, 24, and 48 hours after the surgery. The Mann-Whitney U test was performed in this regard.
Results: There were no significant differences between the two groups regarding demographic variables (P>0.05). The preoperative use of CHX mouth rinse showed a better performance in mitigating the perceived pain. A significant difference in the pain level (P=0.001) was found only at the 6th hour postoperatively although there was no significant difference in the pain level between the two groups (P>0.05) at all other times (12th, 24th, 48th hours). The total number of analgesics that were taken by the study group was significantly lower compared to the control group (P=0.042).
Conclusions: The preoperative CHX mouth rinse could be a beneficial choice for reducing pain after simple tooth extractions.
Keywords: Pain, Chlorhexidine, Tooth extraction, Mouth wash
Copyright and License Information
© 2020 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Haghighat A, Ramezanzade S. Effectiveness of preoperative chlorhexidine mouthwash on pain after lower posterior teeth removal: a randomized, double-blind clinical trial. Avicenna J Dent Res. 2020;12(4):112-119. doi: 10.34172/ ajdr.2020.23.
Background
Highlights
-
Pain is one of the most common and important complications after tooth removal procedures
-
Preprocedural rinsing with CHX has a profound and sustained effect on diminishing the bacterial load of the oral cavity
-
The effectiveness of preoperative CHX mouth rinse in controlling postoperative pain might be attributed to its antibacterial activity.
-
Preoperative use of CHX mouth rinse before simple tooth extraction significantly mitigated the perceived pain at the sixth hour after extraction.
Patients may experience pain after simple tooth extraction. Its intensity varies between different cases (1) and mostly peaks within the first 24 hours post-extraction then drops gradually (2).
Pain is one of the most common and important complications after tooth removal procedures and pain control is a key part of the practice (3,4). Methods advocated for this purpose include systemic analgesic intake (5), positioning analgesic dressings, a single-dose preoperative dexamethasone (6), and the use of different pharmaceutical options in form of a gel and mouth rinse, and the like (7-11). Chlorhexidine (CHX) as a biguanide antiseptic has a broad spectrum of activity against Gram-positive and Gram-negative organisms, oral aerobes, and anaerobes. It has general good tolerability while creating no resistance (12-14).
It has been shown that preoperative rinsing with CHX gluconate mouthwash reduces the salivary bacteria count (15).
According to some studies, poor oral hygiene accompanies greater pain and analgesic consumption following operation (16,17). Likewise, the systemic consumption or local implantation of antibiotics might ameliorate the following pain (18-20).
These observations indicate that plaque adhered to teeth and bacteria probably trigger postoperative pain mechanisms and are associated with a higher probability of postoperative complications including pain.
Thus, CHX could be associated with a lesser probability of postoperative pain due to its antiseptic quality. In addition, the majority of the published work concerns the role of CHX on the incidence of dry socket (9,11), and the potential therapeutic effect of CHX on postsurgical pain is an entire missing point in the literature although some previous studies have partially addressed this issue with conflicting evidence. It has been reported that intra-alveolar CHX placement could reduce postsurgical pain regardless of its dry socket preventive effect (7,8). Nevertheless, the split-mouth design has found it ineffective and argued that the intra-alveolar CHX gel did not significantly alter post-extraction pain (9). The inconclusiveness of the results rationalized further studies for this agent. Although the simple extraction of permanent teeth is one of the most common practices among dentists, all previous studies have focused on perceived pain after the surgical removal of impacted third molars and no study has ever distinguished CHX effects on simple tooth extraction pain.
Accordingly, the present study aimed to investigate the role of CHX on pain and analgesic consumption after simple tooth extraction while controlling for confounders such as dry socket and infection.
The effects of patients’ gender, age, and the number of extracted teeth on pain intensity at different times also were examined based on the aim of the study.
Materials and Methods
This randomized, double-blind, single-center clinical trial was performed at a dental clinic in Isfahan, Iran. After obtaining the approval of the institutional and university ethics board (Ethics code: IR.MUI.RESEARCH.REC.1397.482, IRCT code: IRCT20121223011856N2) and signed detailed informed consent from all patients, they were enrolled in this study.
Study Sample
In general, 170 subjects were randomly selected from patients attending a dental clinic during a 6-month period (between January 2017 and August 2017) for the unilateral simple tooth extraction of one or two mandibular premolar(s) and molar(s) under local anesthesia. The extracted teeth were not in any pain inducing condition such as irreversible pulpitis and the reasons for tooth extraction were mostly as follows:
-
Candidates of full mouth denture (with a few hopeless teeth)
-
Candidates of orthodontic treatments needing tooth extraction
-
Candidates of non-surgical wisdom teeth removal
-
Candidates of oral rehabilitation with dental implants.
Eligibility Criteria
-
Being in the age range of 18-80 years old;
-
Being healthy and not consuming any regular medication;
-
Not having any pain-inducing conditions such as an aching tooth at the time of the surgery;
On the other hand, patients were excluded if they:
-
Were smokers or ingested any medications including oral contraceptives, analgesics, and antibiotics as of 4 days prior to the operation;
-
Had used CHX regularly before the extraction or within 48 hours after the extraction;
-
Had poor oral hygiene based on the simplified oral hygiene index (21);
-
developed wound dehiscence after extraction.
Patient Allocation
Patients were randomly allocated to the treatment or control group based on the flip of a coin. The treatment group received 0.2% CHX gluconate oral rinse (study group) and the placebo solution was given to the control group. The clinician and patients were blind to this trial and had no idea of the provided mouthwash type.
Treatment Protocol
The subjects were given a dark bottle containing 15 mL of either CHX 0.2% or a placebo 0.5 to 1 hour before performing extractions. CHX digluconate is substantively a broad-spectrum antibiotic with high solubility, the mechanism of action of which can be explained by the chemical interaction between the substance and bacterial cell membranes. The placebo contained all ingredients except for CHX. In fact, CHX was substituted with distilled water in the placebo. The patients were supervised to rinse the assigned solutions around their mouths for two minutes before spitting out and asked not to eat or drink up to extraction time. If any supra gingival calculus existed around the tooth to be extracted, it was removed before the irrigation. All extractions were carried out by an expert clinician (with more than five years of experience in dentoalveolar surgery) who used a standard elevator and forceps technique for all cases. The subjects underwent the operation under local anesthesia with one 1.8-mL cartridge of 2% lidocaine and 1:80 000 epinephrine. Acetaminophen 325 was prescribed to be taken as required for pain relief only in the case of excessive pain with a maximum of 8 tablets/day. They were told not to use any analgesics other than those prescribed or any antibiotics. Otherwise, they would be excluded from the study and replaced by new subjects. Patients were advised to seek help from the operator in case of any problem. Subjects would be excluded in case of the incidence of dry socket or infection. The dry was defined as a severe pain accompanied by disintegrated blood clots within the alveolar socket, and infection was defined as the presence of pus. Proper treatment would be offered after excluding the tooth. The data at the initial visit and follow-up calls were recorded by a single clinical examiner. Postoperative care was identical in all cases. The following post-extraction instructions were given to subjects both verbally and written on a piece of paper as “to bite on the gauze for 30-60 minutes following tooth removal. Not to spit, rinse, drink alcoholic beverages, or smoke for the next 72 hours. To empty your mouth passively when necessary”.
Follow-up Protocol
Postoperative pain was assessed by considering several parameters such as the evaluation of pain using a visual analog scale (VAS) and the number of ingested analgesic tablets. A 10-cm horizontal VAS was used, and the leftmost and rightmost ends define no pain (score 0) and worst possible pain (score 10), respectively. Patients’ postoperative pain and analgesic intake were recorded by 4 telephone interviews 6, 12, and 24 and 48 hours after tooth extraction. During each follow-up, the subjects were asked to make the VAS evaluation of their pain. Moreover, patients were asked if they had used any prescribed pain killer and if so, the dosage of medication was recorded as well.
The possible factors affecting post-extraction pain were also recorded, including gender, age, location extraction side (right or left), and extracted teeth quantity (one or two).
Statistical Analysis
All analyses were conducted by the IBM SPSS 22.0 (Chicago, III, SPSS Inc, Chicago, IL). Demographic data were analyzed using the chi-square test and independent t-test. The Kolmogorov-Smirnov test was used to verify the data distribution. Due to the non-normal distribution of data, the Mann-Whitney U test, Kruskal-Wallis test, and Spearman’s rank correlation coefficient were performed to determine which of the variables (i.e., gender, age, and extracted teeth quantity) affected pain intensity. The Mann-Whitney U test was performed to compare the two groups regarding pain intensity and rescue analgesic intake. The statistical significance was considered as P < 0.05.
Results
A total of 170 patients were enrolled in this trial although 19 (11%) of them failed to comply with follow-ups. In addition, 4 (0.02%) cases were excluded due to post-extraction complications (e.g., dry socket and infection) leaving 147 evaluable subjects with 159 extracted teeth (Figure 1). The CHX group consisted of 84 (57%) patients, and the placebo group consisted of 63 (43%) cases. There were no significant differences with respect to extraction difficulty in the two groups.
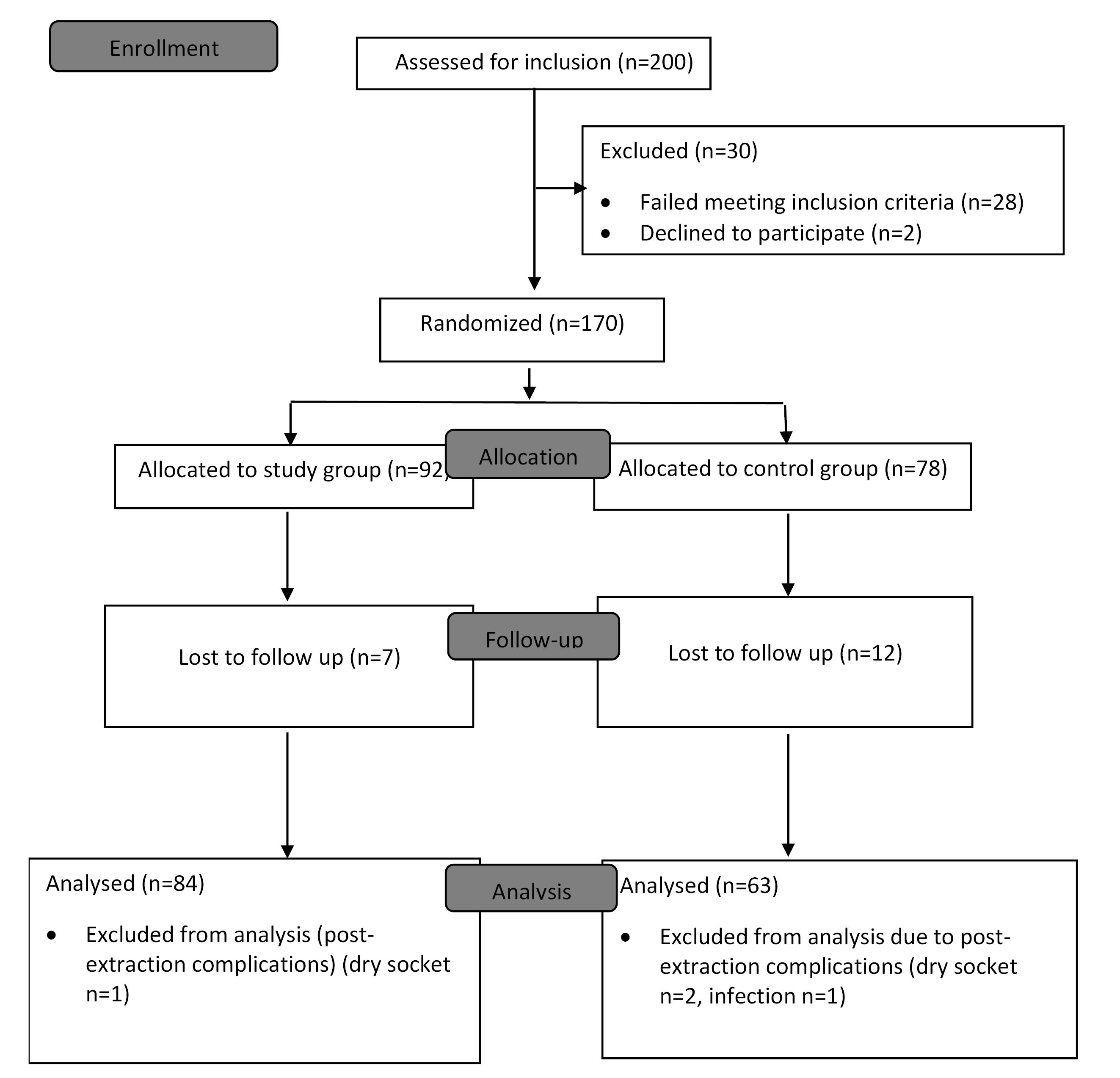
Figure 1.
Study Flow Diagram of Study Participants.
.
Study Flow Diagram of Study Participants.
There were 61 (41.5%) men and 86 (58.5%) women. The mean age of the included patients was 39.55 (in the range of 18-72 years and standard deviation ± 13.18 years). Of all the treated subjects, 76 and 71 cases were on the right and the left sides, respectively. The single teeth were extracted in 89% of cases. With respect to the extracted tooth type, 103 (70%), 39 (26.5%), and 5 (3.5%) of teeth were molars, premolars, and molar and premolar, respectively. Two cases (both of them were single tooth extraction) required supragingival calculus removal, including one in the CHX group and one in the placebo group. The descriptive statistics for the sample are shown in Table 1. Six hours after the extraction, 91.7% and 93.7% of patients in the CHX group and the placebo group reported feeling pain, respectively. These values reduced to 22.6% and 29% at 48 hours post-extraction, respectively. The mean of reported pain as evaluated on VAS in both groups reached its maximum intensity during the first 6 hours after the surgery, and subsequently, reduced steadily over time. Table 2 provides the comparison of pain experienced between the two treatment groups. In comparison with the use of placebo, CHX rinse was found to reduce the suffered pain in the first 48 hours postoperative while the difference in the mean pain score between the two groups was significant only at the first follow-up (P = 0.001) and the data on other times indicated no significant differences. In other words, patients in the CHX group showed a borderline significantly lower amount of pain 24 hours post-extraction (P > 0.05).
Table 1.
Demographic Data of the Study and Control Groups
|
Mouth rinse group
|
-
|
CHX
|
Saline
|
P
value
|
| Sample size |
- |
84 |
63 |
- |
| Age(y), Mean ± SD |
- |
36.25±13.77 |
39.95±12.46 |
.751* |
| Sex, n (%) |
|
|
Male |
38(45.2%) |
23(36.5%) |
.288** |
|
|
Female |
46(56.8%) |
40 (63.5%) |
| Number of Teeth Extracted, n (%) |
|
|
One |
74(88.1%) |
57(90.5%) |
0.646** |
|
|
Two |
10(9.8%) |
6(9.5%) |
Note. CHX: Chlorhexidine; SD: Standard deviation.
* Independent samples t-test
** Chi-square
Table 2.
Data of Pain on 6, 12, 24 and 48 Hours Postoperative
|
|
Case (CHX)
|
Control (Placebo)
|
P
Value
|
|
VAS Pain Intensity
|
VAS Pain Intensity
|
|
Mean ± SD
|
Min
|
Max
|
Mean ± SD
|
Min
|
Max
|
| After 6 hours |
3.22±1.97 |
0 |
8 |
4.47±2.38 |
0 |
9 |
0.001
|
| After 12 hours |
2.16±1.88 |
0 |
7 |
2.68±2.19 |
0 |
9 |
0.175
|
| After 24 hours |
1.03±1.57 |
0 |
8 |
1.46±1.74 |
0 |
7 |
0.054
|
| After 48 hours |
0.33±0.74 |
0 |
4 |
0.57±1.10 |
0 |
4 |
0.300
|
Note. CHX: Chlorhexidine;VAS: Visual analogue scale; Mann-Whitney U test; Min: Minimum; Max: Maximum; SD: Standard deviation.
Most of the analgesics (55.6%) were used during the first 6 hours after the surgery. The comparison of pain experienced between the two treatment groups is shown in Table 3. Patients using the CHX mouthwash preoperatively had a significantly lower total number of applied analgesic (P< 0.05).
Table 3.
Relationship Between the Type of Mouth Rinse and Analgesic Pills Taken on Each Follow-up
|
|
Case (CHX)
|
Control (Placebo)
|
P
Value
|
|
Rescue Medicine Intake
|
Rescue Medicine Intake
|
|
Mean ± SD
|
Min
|
Max
|
Mean ± SD
|
Min
|
Max
|
| After 6 hours |
0.94±0.71 |
0 |
3 |
1.09±0.83 |
0 |
4 |
0.339 |
| After 12 hours |
0.48±0.61 |
0 |
2 |
0.65±0.69 |
0 |
3 |
0.160 |
| After 24 hours |
0.22±0.44 |
0 |
2 |
0.34±0.57 |
0 |
2 |
0.197 |
| After 48 hours |
0.03±0.18 |
0 |
1 |
0.04±0.21 |
0 |
1 |
0.719 |
| Total pills |
1.69±1.42 |
0 |
5 |
2.14±1.69 |
0 |
7 |
0.042 |
Note. CHX:Chlorhexidine; Mann-Whitney U test; Min: Minimum; Max: Maximum; SD: Standard deviation.
Discussion
Pain is an unpleasant experience followed by a stimulus (1). The applied method for measuring pain can affect the results of a clinical study. The use of the VAS has been shown to be a reliable method for pain evaluation, and when properly designed and administered, VAS ensures maximum sensitivity for the measurement of human pain intensity (22,23). Some studies have shown preoperative CHX mouthwash to reduce the incidence of dry socket in simple extractions (24) and the surgical extraction of lower third molars (25,26) although the previous research has paid little attention to the CHX mouthwash pain-reducing effect. Some previous studies have evaluated the effect of CHX on pain after the surgical removal of the third molars, but to the best of our knowledge, this is the first study that presents a detailed analysis of the effect of CHX mouthwash on pain intensity after simple tooth extraction. The use of CHX for postoperative pain alleviation is interesting considering its availability and low cost, along with the negative effects of the excessive use of analgesics after tooth extractions. Likewise, we would like to know if CHX can alleviate the habitual post-extraction pain of healthy sockets regardless of its preventive effects on the pain of the dry socket.
The results of the present study indicated that the preoperative use of CHX mouth rinse before simple tooth extraction significantly mitigated the perceived pain at the sixth hour after extraction (P = 0.01). It also reduced pain at other times although it was not significant (P > 0.05). Based on the results, CHX mouthwash could mitigate pain more effectively in the immediate post-extraction period compared to other times. However, previous studies found CHX effective over a longer period of time after the surgical removal of the third molars (7,8). In addition, a significantly lower number of the total taken rescue analgesics was found in the CHX group in comparison with the placebo group.
A review of the literature suggests that the increased presence of plaque adhered to the teeth may contribute to greater postoperative pain. After extracting 190 impacted third molars, Peñarrocha et al (16) found that poor oral hygiene is associated with higher pain levels and more analgesic intake through the postsurgical period. Similar results were observed by two other studies that investigated that a lower brushing frequency accompanies greater post-surgical pain (17,27). Moreover, there might be a relationship between the magnitude of post-surgical pain and antibiotic prophylaxis whether implanted in the alveolar socket or systemic usage. Likewise, Verbic (18) conducted a preliminary study on 206 patients and concluded that the intra-alveolar implantation of soluble aureomycin tablets lessened the incidence of postoperative pain within the evaluated period (until the seventh day). Such an influence was detectable in some other studies (19,20).
Regarding the intra-alveolar placement of the CHX bioadhesive gel, Haraji et al (7) reported that CHX might decrease postsurgical pain levels for about 10% of potentially tolerable maximum pain in the absence of the dry socket. Similarly, the results of another study revealed that CHX gel could significantly reduce pain intensity, adjusted for its preventive effect on infection and dry sockets (8). Fotos et al (28) reported a 24-48-hour sooner pain alleviation in the CHX site compared to the control site in the same patients. These findings differ from those of Torres-Lagares et al (9), representing no significant influence of intra-alveolar CHX gel on pain after the surgical removal of 30 impacted third molars. However, their study had several shortcomings. First, the sample size was extremely small and insufficient to draw a conclusion. Second, they did not control smoking and contraceptive use. Finally, they were probably unaware of the fact that the pattern of postsurgical pain might depend on the presence/absence of the dry socket (7,16).
MacGregor and Hart (29) assessed the effect of bacteria on postsurgical pain. All sockets produced bacterial growth. Despite detecting and isolating a wide range of organisms from the third molar sockets, they could not find any association between any organism and pain. Thus, they suggested that the deficiencies of the method advocated for microbial culture might be responsible for this failure.
Numerous microbes in and around the socket might lead to the presence of large numbers of cells (e.g., germs and macrophages), products of bacterial activity and bacterial toxins, subsequently, leading to the release of painful inflammatory mediators (30) that trigger the physiopathologic mechanisms of post-extraction pain (31). Preprocedural rinsing with CHX has a profound and sustained effect on diminishing the bacterial load of the oral cavity (32). Hence, the effectiveness of preoperative CHX mouth rinse in controlling postoperative pain might be attributed to its antibacterial activity. Therefore, it is recommended that direct bacteriological studies be conducted to investigate the effect of CHX mouthwash on postoperative pain.
Our results indicated that pain, as evaluated using VAS and analgesic intake, was more intense in the first 6 post-extraction hours for the global group of patients, and subsequently, declined steadily. This finding is in line with almost all previous findings indicating that the highest pain level is experienced at the first postsurgical hours such as the first 6 hours, first 12-24 hours (17), and the first day (7). A likely explanation for differing obtained results in various studies is different types of the applied anesthetic and painkillers (33), as well as variations in surgical difficulty and pain assessment times.
The results of the current study revealed that VAS scores at different times were not significantly correlated with age (Spearman’s correlation coefficient, r~0; P > 0.05). Another study also demonstrated no significant association between age and pain (2). Some studies reported the deteriorating impact of aging on pain (34,35). In contrast, another study found that pain increased in younger patients (36). The effect of age remained inconclusive; therefore, further studies are needed in this regard.
Based on the findings of the present study, there was no significant effect on the number of the extracted teeth (Mann-Whitney U test, P > 0.05), which corroborates with the findings of Al-Khateeb and Alnahar (2) while contradicting those of Levine et al (37), demonstrating that the extent of injury alters patients’ pain perception. Therefore, patients removing 4 impacted wisdom teeth experienced significantly more pain in comparison to those with 2 removed teeth. In our study, the narrow range of the number of the extracted teeth (one or two) could mask such an effect.
In this investigation, females seemed to experience pain to a greater extent than males. The results of the Mann-Whitney U test showed a significant difference in the total number of applied analgesic (P = 0.04) and pain intensity (VAS scores) between males and females on 6, 12, and 24 hours post-extraction (P = 0.02, 0.007, and 0.002, respectively). Most researchers agree that women’s sex hormones, psychologic and sociocultural factors, along with their thinner mandible could render them more sensitive to postoperative pain (2,3,38,39).
This present study was constrained by some shortcomings. Several researchers found CHX bioadhesive gel more efficient than mouthwash and proposed that the intra-alveolar positioning of the gel would allow a more direct action and a more prolonged time of treatment with active substance (9,11). Additionally, the intra-alveolar CHX gel rescues the patient from the most current and troublesome side effect of CHX mouthwash, a brownish discoloration of teeth.
In our study, the pharmaceutical form or the fact that medication was deposited just once might be questionable. Nonetheless, evidence suggests that the absorbed mouth rinse gradually releases and reduces bacterial colonization for up to 24 hours after rinsing with CHX (40,41).
In this study, we did not exactly control oral hygiene before extraction nor during the postoperative period in our subjects. However, patients with poor oral hygiene were excluded from this trial, but this variable has to be taken into account in future studies.
Another issue was the necessity of post-extraction analgesic administration. Some previous studies (7,8) eliminated post-operative analgesics, but this is unacceptable for ethical reasons. Logic would suggest that the use of analgesics may disrupt pain perception thus bias the results. To minimize this effect, we did not prescribe identical painkiller doses for all patients, instead, they were instructed to take medication only in the case of excessive pain.
This study only included the extraction of both premolars and molars of the lower jaw due to the fact that patients had reported similar difficulty in tooth removal and similar pain levels in previous works. The proportion of each tooth type was indicated as well. Cases with more than two extractions were excluded since more than two extractions were reported to affect the amount of pain postoperatively (2).
In our study, cases with wound dehiscence were also excluded since wound dehiscence might compromise the actual effect of the CHX and the healing process, leading to inflammation and subsequent pain.
Like previous works, we districted post-traumatic pain from the pain related to the occurrence of the dry socket by excluding the cases of the dry socket since they are not comparable situations.
Conclusions
In general, our results suggested that CHX might have a therapeutic effect on pain even in the absence of any infection or dry socket.
Conflict of Interest Disclosures
None.
Acknowledgments
This study was financially supported by Isfahan University of Medical Sciences. We acknowledge Dr. A. Sarrami-Foroushani for his valuable contribution.
Ethical Statement
This study was approved by the Research Ethics Committee of Isfahan University of Medical Sciences, Iran (No.: IR.MUI.RESEARCH.REC.1397.482).
Authors’ Contribution
SR: Conceived and designed the analysis; collected the data; contributed data or analysis tools; performed the analysis; wrote the paper. AH: Conceived and designed the analysis, supervised and wrote the paper.
Funding
This research was supported by Isfahan University of Medical Science. Grant No.397642.
References
- Adams G, Wood GD, Hackett AF. Dietary intake and the extraction of third molars: a potential problem. Dent Update 1996; 23(1):31-4. [ Google Scholar]
- Al-Khateeb TH, Alnahar A. Pain experience after simple tooth extraction. J Oral Maxillofac Surg 2008; 66(5):911-7. doi: 10.1016/j.joms.2007.12.008 [Crossref] [ Google Scholar]
- de Santana-Santos T, de Souza-Santos JA, Martins-Filho PR, da Silva LC, de Oliveira e Silva ED, Gomes AC. Prediction of postoperative facial swelling, pain and trismus following third molar surgery based on preoperative variables. Med Oral Patol Oral Cir Bucal 2013; 18(1):e65-70. doi: 10.4317/medoral.18039 [Crossref] [ Google Scholar]
- Phillips C, White RP Jr, Shugars DA, Zhou X. Risk factors associated with prolonged recovery and delayed healing after third molar surgery. J Oral Maxillofac Surg 2003; 61(12):1436-48. doi: 10.1016/j.joms.2003.08.003 [Crossref] [ Google Scholar]
- Comfort MB, Tse AS, Tsang AC, McGrath C. A study of the comparative efficacy of three common analgesics in the control of pain after third molar surgery under local anaesthesia. Aust Dent J 2002; 47(4):327-30. doi: 10.1111/j.1834-7819.2002.tb00546.x [Crossref] [ Google Scholar]
- Baxendale BR, Vater M, Lavery KM. Dexamethasone reduces pain and swelling following extraction of third molar teeth. Anaesthesia 1993; 48(11):961-4. doi: 10.1111/j.1365-2044.1993.tb07474.x [Crossref] [ Google Scholar]
- Haraji A, Rakhshan V, Khamverdi N, Khanzadeh Alishahi H. Effects of intra-alveolar placement of 02% chlorhexidine bioadhesive gel on dry socket incidence and postsurgical pain: a double-blind split-mouth randomized controlled clinical trial. J Orofac Pain 2013; 27(3):256-62. doi: 10.11607/jop.1142 [Crossref] [ Google Scholar]
- Haraji A, Rakhshan V. Chlorhexidine gel and less difficult surgeries might reduce post-operative pain, controlling for dry socket, infection and analgesic consumption: a split-mouth controlled randomised clinical trial. J Oral Rehabil 2015; 42(3):209-19. doi: 10.1111/joor.12230 [Crossref] [ Google Scholar]
- Torres-Lagares D, Infante-Cossio P, Gutierrez-Perez JL, Romero-Ruiz MM, Garcia-Calderon M, Serrera-Figallo MA. Intra-alveolar chlorhexidine gel for the prevention of dry socket in mandibular third molar surgery A pilot study. Med Oral Patol Oral Cir Bucal 2006; 11(2):E179-84. [ Google Scholar]
- Eshghpour M, Mortazavi H, Mohammadzadeh Rezaei N, Nejat A. Effectiveness of green tea mouthwash in postoperative pain control following surgical removal of impacted third molars: double blind randomized clinical trial. Daru 2013; 21(1):59. doi: 10.1186/2008-2231-21-59 [Crossref] [ Google Scholar]
- Torres-Lagares D, Gutierrez-Perez JL, Hita-Iglesias P, Magallanes-Abad N, Flores-Ruiz R, Basallote-Garcia M. Randomized, double-blind study of effectiveness of intra-alveolar application of chlorhexidine gel in reducing incidence of alveolar osteitis and bleeding complications in mandibular third molar surgery in patients with bleeding disorders. J Oral Maxillofac Surg 2010; 68(6):1322-6. doi: 10.1016/j.joms.2009.08.022 [Crossref] [ Google Scholar]
- Briner WW, Grossman E, Buckner RY, Rebitski GF, Sox TE, Setser and RE. Assessment of susceptibility of plaque bacteria to chlorhexidine after six months’ oral use. J Periodontal Res 1986; 21(s16):53-9. doi: 10.1111/j.1600-0765.1986.tb01515.x [Crossref] [ Google Scholar]
- Lang N, Brecx MC. Chlorhexidine digluconate–an agent for chemical plaque control and prevention of gingival inflammation. J Periodontal Res 1986; 21(s16):74-89. doi: 10.1111/j.1600-0765.1986.tb01517.x [Crossref] [ Google Scholar]
- Hennessey TS. Some antibacterial properties of chlorhexidine. J Periodontal Res Suppl 1973; 12:61-7. doi: 10.1111/j.1600-0765.1973.tb02166.x [Crossref] [ Google Scholar]
- Altonen M, Saxen L, Kosunen T, Ainamo J. Effect of two antimicrobial rinses and oral prophylaxis on preoperative degerming of saliva. Int J Oral Surg 1976; 5(6):276-84. doi: 10.1016/s0300-9785(76)80028-2 [Crossref] [ Google Scholar]
- Peñarrocha M, Sanchis JM, Sáez U, Gay C, Bagán JV. Oral hygiene and postoperative pain after mandibular third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001; 92(3):260-4. doi: 10.1067/moe.2001.115722 [Crossref] [ Google Scholar]
- Larrazábal C, García B, Peñarrocha M, Peñarrocha M. Influence of oral hygiene and smoking on pain and swelling after surgical extraction of impacted mandibular third molars. J Oral Maxillofac Surg 2010; 68(1):43-6. doi: 10.1016/j.joms.2009.07.061 [Crossref] [ Google Scholar]
- Verbic RL. Local implantation of aureomycin in extraction wounds: a preliminary study. J Am Dent Assoc 1953; 46(2):160-3. doi: 10.14219/jada.archive.1953.0029 [Crossref] [ Google Scholar]
- Hellem S, Nordenram A. Prevention of postoperative symptoms by general antibiotic treatment and local bandage in removal of mandibular third molars. Int J Oral Surg 1973; 2(6):273-8. doi: 10.1016/s0300-9785(73)80022-5 [Crossref] [ Google Scholar]
- Krekmanov L, Nordenram A. Postoperative complications after surgical removal of mandibular third molars Effects of penicillin V and chlorhexidine. Int J Oral Maxillofac Surg 1986; 15(1):25-9. doi: 10.1016/s0300-9785(86)80007-2 [Crossref] [ Google Scholar]
- Cuenca E, Serra L, Manau C, Echeverría J, Rionóo R, Salleras L. Manual de odontología preventiva y comunitaria. Barcelona: Masson; 1991.
- Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 1983; 17(1):45-56. doi: 10.1016/0304-3959(83)90126-4 [Crossref] [ Google Scholar]
- Seymour RA. The use of pain scales in assessing the efficacy of analgesics in post-operative dental pain. Eur J Clin Pharmacol 1982; 23(5):441-4. doi: 10.1007/bf00605995 [Crossref] [ Google Scholar]
- Field EA, Nind D, Varga E, Martin MV. The effect of chlorhexidine irrigation on the incidence of dry socket: a pilot study. Br J Oral Maxillofac Surg 1988; 26(5):395-401. doi: 10.1016/0266-4356(88)90092-7 [Crossref] [ Google Scholar]
- Hermesch CB, Hilton TJ, Biesbrock AR, Baker RA, Cain-Hamlin J, McClanahan SF. Perioperative use of 012% chlorhexidine gluconate for the prevention of alveolar osteitis: efficacy and risk factor analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998; 85(4):381-7. doi: 10.1016/s1079-2104(98)90061-0 [Crossref] [ Google Scholar]
- Ragno JR Jr, Szkutnik AJ. Evaluation of 012% chlorhexidine rinse on the prevention of alveolar osteitis. Oral Surg Oral Med Oral Pathol 1991; 72(5):524-6. doi: 10.1016/0030-4220(91)90487-w [Crossref] [ Google Scholar]
- Sáez-Cuesta Ú, Peñarrocha Diago M, Sanchis Bielsa JM, Gay Escoda C. Estudio del postoperatorio de 100 terceros molares mandibulares incluidos, en relación a la edad, el sexo, el tabaco y la higiene bucal. Revista del Ilustre Consejo General de Colegios de Odontólogos y Estomatólogos de España (RCOE) 1999; 4(5):471-5. [ Google Scholar]
- Fotos PG, Koorbusch GF, Sarasin DS, Kist RJ. Evaluation of intra-alveolar chlorhexidine dressings after removal of impacted mandibular third molars. Oral Surg Oral Med Oral Pathol 1992; 73(3):383-8. doi: 10.1016/0030-4220(92)90140-l [Crossref] [ Google Scholar]
- MacGregor AJ, Hart P. Effect of bacteria and other factors on pain and swelling after removal of ectopic mandibular third molars. J Oral Surg 1969; 27(3):174-9. [ Google Scholar]
- Grossi SG, Genco RJ, Machtei EE, Ho AW, Koch G, Dunford R. Assessment of risk for periodontal disease II Risk indicators for alveolar bone loss. J Periodontol 1995; 66(1):23-9. doi: 10.1902/jop.1995.66.1.23 [Crossref] [ Google Scholar]
- Sanchis JM. Penarrocha M. Dolor orofacial postquirurgico. In: Diago MP, ed. Dolor Orofacial: Etiología, Diagnóstico y Tratamiento. Barcelona: Mason; 1997. p. 267-70.
- Veksler AE, Kayrouz GA, Newman MG. Reduction of salivary bacteria by pre-procedural rinses with chlorhexidine 012%. J Periodontol 1991; 62(11):649-51. doi: 10.1902/jop.1991.62.11.649 [Crossref] [ Google Scholar]
- Lago-Méndez L, Diniz-Freitas M, Senra-Rivera C, Gude-Sampedro F, Gándara Rey JM, García-García A. Relationships between surgical difficulty and postoperative pain in lower third molar extractions. J Oral Maxillofac Surg 2007; 65(5):979-83. doi: 10.1016/j.joms.2006.06.281 [Crossref] [ Google Scholar]
- Osborn TP, Frederickson G Jr, Small IA, Torgerson TS. A prospective study of complications related to mandibular third molar surgery. J Oral Maxillofac Surg 1985; 43(10):767-9. doi: 10.1016/0278-2391(85)90331-3 [Crossref] [ Google Scholar]
- Phillips C, White RP Jr, Shugars DA, Zhou X. Risk factors associated with prolonged recovery and delayed healing after third molar surgery. J Oral Maxillofac Surg 2003; 61(12):1436-48. doi: 10.1016/j.joms.2003.08.003 [Crossref] [ Google Scholar]
- Maggirias J, Locker D. Psychological factors and perceptions of pain associated with dental treatment. Community Dent Oral Epidemiol 2002; 30(2):151-9. doi: 10.1034/j.1600-0528.2002.300209.x [Crossref] [ Google Scholar]
- Levine JD, Gordon NC, Smith R, Fields HL. Post-operative pain: effect of extent of injury and attention. Brain Res 1982; 234(2):500-4. doi: 10.1016/0006-8993(82)90894-0 [Crossref] [ Google Scholar]
- Rakhshan V. Common risk factors for postoperative pain following the extraction of wisdom teeth. J Korean Assoc Oral Maxillofac Surg 2015; 41(2):59-65. doi: 10.5125/jkaoms.2015.41.2.59 [Crossref] [ Google Scholar]
- Wiesenfeld-Hallin Z. Sex differences in pain perception. Gend Med 2005; 2(3):137-45. doi: 10.1016/s1550-8579(05)80042-7 [Crossref] [ Google Scholar]
- Brecx M, Theilade J. Effect of chlorhexidine rinses on the morphology of early dental plaque formed on plastic film. J Clin Periodontol 1984; 11(9):553-64. doi: 10.1111/j.1600-051x.1984.tb00908.x [Crossref] [ Google Scholar]
- Yankell SL, Moreno OM, Saffir AJ, Lowary RL, Gold W. Effects of chlorhexidine and four antimicrobial compounds on plaque, gingivitis, and staining in beagle dogs. J Dent Res 1982; 61(9):1089-93. doi: 10.1177/00220345820610091201 [Crossref] [ Google Scholar]