Avicenna J Dent Res. 12(1):13-18.
doi: 10.34172/ajdr.2020.04
Original Article
The Effect of Silver Diamine Fluoride Versus Sodium Fluoride Varnish on the Microhardness of Demineralized Enamel: An In Vitro Study
Nasrin Farhadian 1  , Maryam Farhadian 2, Mozhde Borjali 3, *
, Maryam Farhadian 2, Mozhde Borjali 3, *  , Esmaeil Ghaderi 4
, Esmaeil Ghaderi 4
Author information:
1Professor of Orthodontics, Department of Orthodontics, School of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran.
2Assistant Professor, Department of Biostatistics, School of Public Health and Research Center for Health Sciences, Hamadan University of Medical Sciences, Hamadan, Iran.
3Postgraduate Orthodontic Student, Department of Orthodontics, School of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran.
4Bachelor Degree in Chemistry, Iran laboratory, Ashoora square, Hamadan, Iran.
Abstract
Background: Fixed orthodontic treatment has been associated with certain side effects such as white spot lesions (WSLs). Many studies showed the positive effect of sodium fluoride (NaF) varnish in remineralizing WSLs. Studies revealed that silver diamine fluoride (SDF) is effective in arresting dentin caries, but its potential for enamel remineralization has not been investigated clearly. The present study aimed to compare the effect of SDF and NaF on the microhardness of demineralized enamel.
Methods: A total of 60 intact premolar teeth were collected and divided into 4 equal groups. Group 1 remained intact (control). Groups 2 to 4 were exposed to artificial cariogenic solution to create enamel lesion. Then, groups 3 and 4 were treated with NaF 5% and SDF 38%, respectively. After one month of storage in artificial saliva, NaF and SDF were reapplied. One month later, the surface microhardness values (SMHs) of teeth were assessed.
Results: The results of ANOVA showed a significant difference among the 4 groups (P<0.001). There was significantly higher enamel microhardness in the control group compared with groups 2 and 3 (P<0.001); however, it was not significant for the SDF group (P=0.160). There was significantly higher enamel surface microhardness in groups 3 and 4 compared with group 2 (P≤0.001) and significantly higher mean SMH values in the SDF group compared with the NaF group (P=0.004).
Conclusions: NaF varnish and SDF can both remineralize early enamel lesion but SDF has greater remineralizing potential.
Keywords: White spot, Silver diamine fluoride, Tooth remineralization, Sodium fluoride
Copyright and License Information
© 2020 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Farhadian N, Farhadian M, Borjali M, Ghaderi E. The Effect of Silver Diamine Fluoride Versus Sodium Fluoride Varnish on the Microhardness of Demineralized Enamel: An In Vitro Study. Avicenna J Dent Res. 2020;12(1):13-18. doi: 10.34172/ajdr.2020.04.
Background
Highlights
-
Sodium fluoride (NaF) and silver diamine fluoride can both remineralize early enamel lesion.
-
Silver diamine fluoride has a higher remineralizing potential than NaF.
-
Silver diamine fluoride can cause enamel discoloration.
Fixed orthodontic treatment has become an integral part of modern orthodontics, but it has been associated with certain side effects such as white spot lesions (WSLs) (1). The difficulties in performing oral hygiene procedures give rise to these lesions (2-4).
WSLs are defined as “subsurface enamel porosity” appearing as small lines around the brackets, with a negative impact on the esthetic outcome of orthodontic treatment which might progress into carious lesions (2,5). On average, WSLs are found in 15.5%‒40% of patients before orthodontic treatment and increases to 30‒70% during the treatment (5). After removal of fixed appliances, a considerable improvement in WSLs is seen during the first 6-24 months; however, in many cases, these lesions remain visible as a permanent enamel scar (1,4,5).
Fluoride is the most important element that increases the strength of the enamel structure, and based on a meta-analysis, fluoride varnish can heal post-orthodontic WSLs (1,6). Advantages of fluoride varnishes over other topical fluoride regimens include the protection of enamel in the absence of patient compliance and continuous fluoride release over a long period (5). Silver diamine fluoride (SDF) was introduced in Japan in the 1970s and cleared by the Food and Drug Administration (FDA) in 2014 for the market. Silver acts as an antimicrobial agent and fluoride promotes remineralization. SDF reacts with calcium and phosphate ions and produces fluorohydroxyapatite (7-9).
Many studies demonstrated that SDF is effective in arresting dentin caries, but sometimes, treated teeth develop stains. The staining can be minimized by the application of potassium iodide solution after treatment without reducing the effect (10-15). Studies conducted on extracted teeth receiving semiannual applications of SDF have demonstrated its effectiveness in arresting lesions as well as higher fluoride uptake compared to fluoride varnish (7,8,13,16,17). A recent in vitro study conducted by Akyildiz and Sönmez revealed that SDF and sodium fluoride (NaF) varnish could both remineralize artificial enamel lesions, however, NaF varnish had a higher remineralizing potential (18).
The present in vitro study aimed to compare the effects of SDF and NaF varnish on the microhardness of artificial enamel lesions. Given its beneficial effects on the lesions, it can be used for further clinical trials in orthodontic patients.
Materials and Methods
A total of 60 human premolar teeth, with no caries, cracks, or hypoplastic lesions extracted for orthodontic reasons, were collected. They were disinfected by immersion in thymol solution 0.1% and then washed with saline. The roots of the teeth were cut 2 mm below the cementoenamel junction. The crowns were mounted on self-cure acrylic plates, with their buccal surface facing up (Figure 1).

Figure 1.
our Experimental Groups of Teeth Mounted on Acrylic Plates with Different Colors (a: Control Group, b: Demineralized Enamel Group, c: Sodium Fluoride Varnish 5% Group, and d: Silver Diamine Fluoride 38% Group).
.
our Experimental Groups of Teeth Mounted on Acrylic Plates with Different Colors (a: Control Group, b: Demineralized Enamel Group, c: Sodium Fluoride Varnish 5% Group, and d: Silver Diamine Fluoride 38% Group).
These teeth were randomly divided into four equal groups (15 teeth in each) as follows:
-
Group 1: the control group which remained intact with no intervention (mounted on yellow plates),
-
Group 2: only demineralizing solution was applied (mounted on blue plates),
-
Group 3: received NaF varnish 5% after demineralization process (mounted on red plates),
-
Group 4: received SDF solution 38% after the demineralization process (mounted on purple plates).
The teeth were brushed to remove the tissue remnants. All surfaces of teeth were covered with acid-resistant varnish except for a square area at the center of the buccal surface (2 mm*2 mm). The teeth in the group (1) were kept in artificial saliva (NaCl [400 mg/L], KCl [400 mg/L], CaCl2.H2O [795 mg/L], Na2H2PO4.H2O [690 mg/L], KSCN [300 mg/L], Na2S.9H2O [5 mg/L], Urea [1000 mg/L]) (19) with no intervention. All other teeth were immersed in demineralizing solution (calcium chloride [2.0 mmol/L], tri-sodium phosphate [2.0 mmol/L] in acetate buffer [75 mmol/L]) at 4.6 pH for 6 days, with daily refreshment of the solution to maintain the pH (20).
Then, the teeth in groups 2, 3, and 4 were washed with distilled water and air-dried. The teeth in group 2 were kept in artificial saliva in a separate container as group 1. The SDF solution 38% (w/v) (25% silver, 5.5% fluoride, and 8% ammonia) was made in a laboratory using hydrofluoric acid 48% (Merck, Darmstadt, Germany), silver nitrate (Merck, Darmstadt, Germany), and ammonia solution 25% (Merck, Darmstadt, Germany).
Groups 3 and 4 were treated with NaF varnish 5% (Duraphat®, Colgate, Sao Paulo) and SDF solution 38%, respectively. Then, they were wiped out with a cotton roll after 3 minutes and were kept in artificial saliva in separate containers.
All samples were incubated at 37°C for one month and brushed daily with a soft toothbrush. Artificial saliva was also replaced weekly. After one month, the teeth in groups 3 and 4 were washed with distilled water. Then, NaF varnish and SDF solution were reapplied respectively and the teeth were kept under the former conditions. One month later, the teeth were washed with saline and air dried.
In microhardness testing, an indentation is made on the specimen by a diamond indenter through the application of a load (21). The surface microhardness of each tooth was assessed at three points of the enamel surface, approximately 500 microns apart from each other (Figure 2), using Vickers microhardness tester (KOOPA MH4, Mazandaran, Iran) under a 0.2 kg load and dwell time of 10 seconds (Figure 3). The mean was recorded as the surface microhardness value (SMH) for each tooth. Then, the SMH values of the four experimental groups were compared.

Figure 2.
The Effect of the Indenter on the Enamel.
.
The Effect of the Indenter on the Enamel.

Figure 3.
Vickers Microhardness Tester (KOOPA MH4, Mazandaran, Iran).
.
Vickers Microhardness Tester (KOOPA MH4, Mazandaran, Iran).
Data were saved on an Excel spreadsheet, and statistics were calculated using the Statistical Package for the Social Sciences (SPSS) software version 21.0 (SPSS Inc., Chicago, IL, USA). Kolmogorov-Smirnov test showed that surface microhardness of teeth in the four groups had a normal distribution.
The mean SMH values were compared between groups using one-way ANOVA and Tukey post hoc test. The level of significance was set at 0.05.
Results
The descriptive results are demonstrated in Table 1. The results of ANOVA showed a significant difference among the four groups (P < 0.001) (Table 2).
Table 1.
Microhardness of Enamel in the Study Groups
|
|
N
|
Mean
|
Std. Deviation
|
Std. Error
|
95% CI for Mean
|
Minimum
|
Maximum
|
|
Lower Bound
|
Upper Bound
|
| Control (group 1) |
15 |
361.7 |
35.9 |
9.2 |
341.8 |
381.6 |
280.6 |
413.5 |
| Demineralized enamel (group 2) |
15 |
231.1 |
26.2 |
6.7 |
216.5 |
245.6 |
174.0 |
261.9 |
| NaFa (group 3) |
15 |
286.6 |
33.3 |
8.6 |
268.1 |
305.0 |
208.4 |
331.5 |
| SDFb (group 4) |
15 |
333.6 |
46.8 |
12.0 |
307.7 |
359.5 |
273.0 |
407.9 |
| Total |
60 |
303.2 |
61.2 |
7.9 |
287.4 |
319.1 |
174.0 |
413.5 |
Table 2.
Results of One-Way ANOVA to Compare the SMH Values Between Groups
|
|
Sum of Squares
|
df
|
Mean Square
|
F
|
P
Value*
|
| Between groups |
147439.36 |
3 |
49146.45 |
37.20 |
0.000 |
| Within groups |
73969.11 |
56 |
1320.87 |
|
|
| Total |
221408.47 |
59 |
|
|
|
* The mean difference is significant at the 0.05 level.
There was a significant higher enamel microhardness in the control group compared with the demineralized enamel and NaF groups (P < 0.001) according to Tukey post hoc test, but it was not significant for the SDF group (P = 0.160). There was significantly higher enamel surface microhardness in NaF and SDF groups compared with the demineralized enamel group (P = 0.001, P < 0.001). Interestingly, there were significantly higher mean SMH values in the SDF group compared with the NaF group (P = 0.004) (Table 3).
Table 3.
Multiple Comparisons With Tukey Post Hoc Test
|
(I) Group
|
(J) Group
|
Mean Difference (I-J)
|
Std. Error
|
P
Value*
|
| Control (group 1) |
Demineralized enamel (group 2) |
130.6 |
13.2 |
0.000 |
| Control (group 1) |
NaFa (group 3) |
75.1 |
13.2 |
0.000 |
| Control (group 1) |
SDFb (group 4) |
28.0 |
13.2 |
0.160 |
| Demineralized enamel (group 2) |
NaFa (group 3) |
-55.5 |
13.2 |
0.001 |
| Demineralized enamel (group 2) |
SDFb (group 4) |
-102.5 |
13.2 |
0.000 |
| NaF† (group 3) |
SDFb (group 4) |
-47.0 |
13.2 |
0.004 |
*. The mean difference is significant at the 0.05 level.
a NaF: Sodium fluoride varnish 5%.
b SDF: Silver diamine fluoride solution 38%.
A box plot has been created to compare the values between different experimental groups (Figure 4). The normal distribution was established in the control and NaF groups. The SDF group showed the highest dispersion of the data. Teeth treated with SDF showed enamel discoloration (grayish brown) a few days after the application of SDF. The discoloration was caused by the silver component of the SDF.
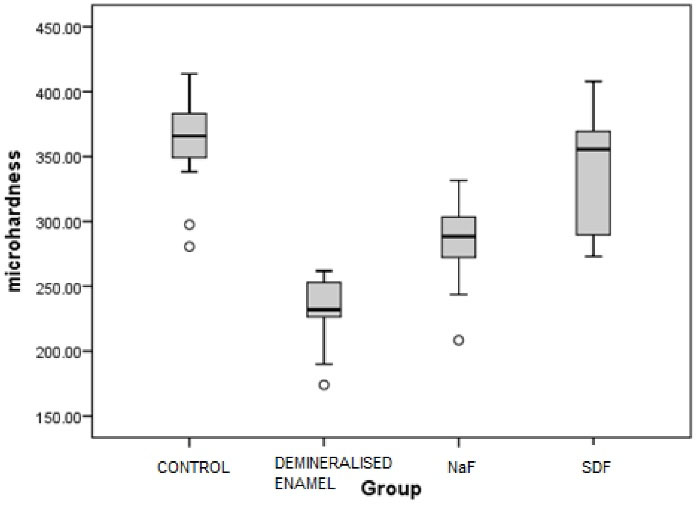
Figure 4.
A Box Plot for the Comparison of the Values Between Different Experimental Groups.
.
A Box Plot for the Comparison of the Values Between Different Experimental Groups.
Discussion
The present study assessed the effects of NaF varnish 5% and SDF solution 38% on the microhardness of demineralized enamel.Vickers microhardness test was used to evaluate remineralization as an indirect test that can measure the changes in surface structural strength. The average hardness value for enamel is in the range of 250 to 360 VHN (22).
There are various in vitro and in vivo studies about the treatment of enamel demineralization with NaF varnish, but the enamel remineralization potential of SDF has not been investigated much yet (8,18,23-25).
SDF can arrest caries and treat dentin hypersensitivity. In the treatment of exposed sensitive dentin, it forms a layer of silver-protein conjugates on the decayed surface of the exposed dentin and plugs the dentinal tubules. The first SDF material approved by the FDA was Advantage Arrest (Elevate Oral Care), for desensitizing cold-sensitive teeth (26). On the other hand, silver ions act directly against bacteria in lesions by breaking membranes, denaturing proteins, and inhibiting DNA replication (7,14,16). A recent study also showed the antifungal potency of SDF (27).
Gao et al and Hochli et al conducted two systematic reviews and based on the existing trials and deduced that 5% NaF varnish can remineralize early enamel caries (1,28).
Contreras et al (29) and Jabin et al (30) conducted two systematic review studies and assessed the effectiveness of SDF on carious dentin in primary teeth and permanent first molars. They concluded that the application of SDF is efficient and safe for the control of dental caries in primary teeth and permanent first molars.
Hendre et al conducted a systematic review of the effectiveness of SDF in the management of root caries in older adults. They assessed 3 randomized clinical trials from 2010 to 2016, all of which supported the effectiveness of SDF in root caries prevention and arrest (31).
Trieu et al conducted a systematic review of the dentine caries arrest capabilities of SDF and NaF. They assessed 6 randomized controlled trials from 2001 to 2018, and concluded that SDF was a more effective caries management reagent than NaF (32).
Zhao et al concluded in their literature review that SDF is a bactericidal agent and reduces the growth of cariogenic bacteria. It inhibits demineralization and promotes the remineralization of demineralized enamel and dentine (33).
Roberts et al conducted a systematic review to assess whether using potassium iodide after the application of SDF significantly reduces the staining of tooth structure. They concluded that although some studies reported positive effects, insufficient evidence exists supporting the benefits of potassium iodide on the tooth staining (34).
Yu et al assessed the remineralizing effect of the adjunctive application of SDF 38% and NaF varnish 5% on artificial enamel lesions. They allocated forty-eight demineralized enamel specimens to four groups. Group 1 received SDF 38% and NaF 5% (SDF + NaF), group 2 received SDF 38%, group 3 received NaF 5%, and group 4 received deionized water. The surface morphology, fluoride content of the specimens, lesion depth, and crystal characteristics were assessed. They concluded that SDF showed stronger remineralizing effects than NaF did but no significant difference was found between the SDF + NaF group and SDF group. This study revealed that the adjunctive application of SDF and NaF varnish had a similar remineralizing effect to SDF on enamel caries (35).
Akyildiz and Sönmez compared the remineralizing potential of NaF and SDF on artificial enamel lesions of human third molar teeth. They measured the Vickers microhardness values of specimens and concluded that NaF and SDF can both remineralize enamel caries but NaF is significantly more effective than SDF (18).
In the present study, NaF and SDF were both capable of remineralizing early enamel carious lesions of the premolar teeth, but SDF showed higher remineralizing potential and the teeth treated with SDF revealed higher surface microhardness which was comparable with sound enamel.
SDF is inexpensive and therefore affordable in most communities. The treatment procedure is simple and requires no expensive equipment or support infrastructure (10,11). SDF has a shelf life of 3 years unopened and its only contraindication is allergy to silver. The advantage of SDF in remineralization (annually or biannually) could be compromised by its potential for enamel discoloration, especially in esthetic zones.
Maintaining hygiene in non-esthetic posterior areas of the mouth is more difficult and especially after the removal of orthodontic appliances, demineralized lesions in these areas are prone to the progression of decay. Due to the better performance of SDF than NaF, which increased the hardness of white spots to the level of intact enamel, and its requirement for less frequent professional application (biannually) in high-risk cases than NaF (every 3 months), the use of SDF in these areas seems more advantageous.
Conclusions
NaF varnish 5% and SDF 38% can both remineralize early enamel lesion, but it seems that SDF has greater efficacy. SDF can cause enamel discoloration; therefore, using SDF is not appropriate in the esthetic zone.
Conflict of Interests Disclosures
The authors declare that they have no competing financial interests or personal relationships that could have appeared to influence the work reported in this study.
Acknowledgements
The authors gratefully acknowledge the support of this work by the Vice-chancellor for Research and Technology, Hamadan University of Medical Sciences, for financial support.
Ethical Statement
The project was found to be in accordance to the ethical principles and the national norms and standards for conducting medical research in Iran by the ethics committee of Hamadan University of Medical Sciences (approval ID: IR.UMSHA.REC.1397.781).
Authors’ Contribution
NF: conceived the ideas and methodology, collected the data, interpreted the data, led the writing and editing and final approval of manuscript. MF: analyzed the data, interpreted the data and final approval of manuscript. MB: conceived the ideas and methodology, collected the data, led the writing and editing and final approval of manuscript. EG: collected the data, led the writing and editing and final approval of manuscript.
Funding
This research was financially supported by Hamadan University of Medical Sciences (No. 9806124441).
References
- Höchli D, Hersberger-Zurfluh M, Papageorgiou SN, Eliades T. Interventions for orthodontically induced white spot lesions: a systematic review and meta-analysis. Eur J Orthod 2017; 39(2):122-33. doi: 10.1093/ejo/cjw065 [Crossref] [ Google Scholar]
- Sundararaj D, Venkatachalapathy S, Tandon A, Pereira A. Critical evaluation of incidence and prevalence of white spot lesions during fixed orthodontic appliance treatment: a meta-analysis. J Int Soc Prev Community Dent 2015; 5(6):433-9. doi: 10.4103/2231-0762.167719 [Crossref] [ Google Scholar]
- Oz AZ, Oz AA, Yazıcıoglu S. In vivo effect of antibacterial and fluoride-releasing adhesives on enamel demineralization around brackets: a micro-CT study. Angle Orthod 2017; 87(6):841-6. doi: 10.2319/060217-371.1 [Crossref] [ Google Scholar]
- Karabekiroğlu S, Ünlü N, Küçükyilmaz E, Şener S, Botsali MS, Malkoç S. Treatment of post-orthodontic white spot lesions with CPP-ACP paste: a three year follow up study. Dent Mater J 2017; 36(6):791-7. doi: 10.4012/dmj.2016-228 [Crossref] [ Google Scholar]
- Khoroushi M, Kachuie M. Prevention and treatment of white spot lesions in orthodontic patients. Contemp Clin Dent 2017; 8(1):11-9. doi: 10.4103/ccd.ccd_216_17 [Crossref] [ Google Scholar]
- Rafatjou R, Ronasi N, Rastegar Y, Safe M, Khezri Sarijeh N. Comparison of Fluoride content in drinking water and prevalence of dental fluorosis in 6 - 12-year-old students in Mariwan (a cold region) and Behbahan (a warm region) during the 2013-2014 educational year. Avicenna J Dent Res 2016; 8(4):e28153. doi: 10.17795/ajdr-28153 [Crossref] [ Google Scholar]
- Horst JA, Ellenikiotis H, Milgrom PL. UCSF protocol for caries arrest using silver diamine fluoride: rationale, indications and consent. J Calif Dent Assoc 2016; 44(1):16-28. [ Google Scholar]
- Shah SG, Bhaskar V, Chawla S. Efficacy of silver diamine fluoride as a topical fluoride agent compared to fluoride varnish and acidulated phosphate fluoride gel: An in vivo study. Journal of Pediatric Dentistry 2014; 2(1):5. [ Google Scholar]
- Mei ML, Nudelman F, Marzec B, Walker JM, Lo ECM, Walls AW. Formation of fluorohydroxyapatite with silver diamine fluoride. J Dent Res 2017; 96(10):1122-8. doi: 10.1177/0022034517709738 [Crossref] [ Google Scholar]
- Chu CH, Lo EC, Lin HC. Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese pre-school children. J Dent Res 2002; 81(11):767-70. doi: 10.1177/0810767 [Crossref] [ Google Scholar]
- Chu CH, Lo EC. Promoting caries arrest in children with silver diamine fluoride: a review. Oral Health Prev Dent 2008; 6(4):315-21. [ Google Scholar]
- Chu CH, Mei L, Seneviratne CJ, Lo EC. Effects of silver diamine fluoride on dentine carious lesions induced by Streptococcus mutans and Actinomyces naeslundii biofilms. Int J Paediatr Dent 2012; 22(1):2-10. doi: 10.1111/j.1365-263X.2011.01149.x [Crossref] [ Google Scholar]
- Rosenblatt A, Stamford TC, Niederman R. Silver diamine fluoride: a caries “silver-fluoride bullet”. J Dent Res 2009; 88(2):116-25. doi: 10.1177/0022034508329406 [Crossref] [ Google Scholar]
- Castillo JL, Rivera S, Aparicio T, Lazo R, Aw TC, Mancl LL. The short-term effects of diammine silver fluoride on tooth sensitivity: a randomized controlled trial. J Dent Res 2011; 90(2):203-8. doi: 10.1177/0022034510388516 [Crossref] [ Google Scholar]
- Nguyen V, Neill C, Felsenfeld J, Primus C. Potassium Iodide. The solution to silver diamine fluoride discoloration? Adv Dent Oral Health 2017; 5(1):1-6. doi: 10.19080/adoh.2017.05.5555655 [Crossref] [ Google Scholar]
- Mei ML, Ito L, Cao Y, Lo EC, Li QL, Chu CH. An ex vivo study of arrested primary teeth caries with silver diamine fluoride therapy. J Dent 2014; 42(4):395-402. doi: 10.1016/j.jdent.2013.12.007 [Crossref] [ Google Scholar]
- Fung MHT, Duangthip D, Wong MCM, Lo ECM, Chu CH. Arresting dentine caries with different concentration and periodicity of silver diamine fluoride. JDR Clin Trans Res 2016; 1(2):143-52. doi: 10.1177/2380084416649150 [Crossref] [ Google Scholar]
- Akyildiz M, Sönmez IS. Comparison of remineralising potential of nano silver fluoride, silver diamine fluoride and sodium fluoride varnish on artificial caries: an in vitro study. Oral Health Prev Dent 2019; 17(5):469-77. doi: 10.3290/j.ohpd.a42739 [Crossref] [ Google Scholar]
- Pytko-Polonczyk JJ, Jakubik A, Przeklasa-Bierowiec A, Muszynska B. Artificial saliva and its use in biological experiments. J Physiol Pharmacol 2017; 68(6):807-13. [ Google Scholar]
- Chokshi K, Chokshi A, Konde S, Shetty SR, Chandra KN, Jana S. An in vitro comparative evaluation of three remineralizing agents using confocal microscopy. J Clin Diagn Res 2016; 10(6):ZC39-42. doi: 10.7860/jcdr/2016/18191.7984 [Crossref] [ Google Scholar]
- Smallman RE, Bishop RJ. Chapter 5 - The characterization of materials. In: Smallman RE, Bishop RJ, editors. Modern Physical Metallurgy and Materials Engineering. 6th ed. Oxford: Butterworth-Heinemann; 1999. p. 125-67. 10.1016/b978-075064564-5/50005-7.
- del Pilar Gutiérrez-Salazara M, Reyes-Gasga J. Microhardness and chemical composition of human tooth. Mater Res 2003; 6(3):367-73. doi: 10.1590/s1516-14392003000300011 [Crossref] [ Google Scholar]
- Nozari A, Ajami S, Rafiei A, Niazi E. Impact of nano hydroxyapatite, nano silver fluoride and sodium fluoride varnish on primary teeth enamel remineralization: an in vitro study. J Clin Diagn Res 2017; 11(9):ZC97-ZC100. doi: 10.7860/jcdr/2017/30108.10694 [Crossref] [ Google Scholar]
- Salehzadeh Esfahani K, Mazaheri R, Pishevar L. Effects of treatment with various remineralizing agents on the microhardness of demineralized enamel surface. J Dent Res Dent Clin Dent Prospects 2015; 9(4):239-45. doi: 10.15171/joddd.2015.043 [Crossref] [ Google Scholar]
- Restrepo M, Bussaneli DG, Jeremias F, Cordeiro RC, Magalhães AC, Palomari Spolidorio DM. Control of white spot lesion adjacent to orthodontic bracket with use of fluoride varnish or chlorhexidine gel. ScientificWorldJournal 2015; 2015:218452. doi: 10.1155/2015/218452 [Crossref] [ Google Scholar]
- Burgess JO, Vaghela PM. Silver diamine fluoride: a successful anticarious solution with limits. Adv Dent Res 2018; 29(1):131-4. doi: 10.1177/0022034517740123 [Crossref] [ Google Scholar]
- Fakhruddin KS, Egusa H, Ngo HC, Panduwawala C, Pesee S, Venkatachalam T. Silver diamine fluoride (SDF) used in childhood caries management has potent antifungal activity against oral Candida species. BMC Microbiol 2020; 20(1):95. doi: 10.1186/s12866-020-01776-w [Crossref] [ Google Scholar]
- Gao SS, Zhang S, Mei ML, Lo EC, Chu CH. Caries remineralisation and arresting effect in children by professionally applied fluoride treatment - a systematic review. BMC Oral Health 2016; 16:12. doi: 10.1186/s12903-016-0171-6 [Crossref] [ Google Scholar]
- Contreras V, Toro MJ, Elías-Boneta AR, Encarnación-Burgos A. Effectiveness of silver diamine fluoride in caries prevention and arrest: a systematic literature review. Gen Dent 2017; 65(3):22-9. [ Google Scholar]
- Jabin Z, Vishnupriya V, Agarwal N, Nasim I, Jain M, Sharma A. Effect of 38% silver diamine fluoride on control of dental caries in primary dentition: a Systematic review. J Family Med Prim Care 2020; 9(3):1302-7. doi: 10.4103/jfmpc.jfmpc_1017_19 [Crossref] [ Google Scholar]
- Hendre AD, Taylor GW, Chávez EM, Hyde S. A systematic review of silver diamine fluoride: effectiveness and application in older adults. Gerodontology 2017; 34(4):411-9. doi: 10.1111/ger.12294 [Crossref] [ Google Scholar]
- Trieu A, Mohamed A, Lynch E. Silver diamine fluoride versus sodium fluoride for arresting dentine caries in children: a systematic review and meta-analysis. Sci Rep 2019; 9(1):2115. doi: 10.1038/s41598-019-38569-9 [Crossref] [ Google Scholar]
- Zhao IS, Gao SS, Hiraishi N, Burrow MF, Duangthip D, Mei ML. Mechanisms of silver diamine fluoride on arresting caries: a literature review. Int Dent J 2018; 68(2):67-76. doi: 10.1111/idj.12320 [Crossref] [ Google Scholar]
- Roberts A, Bradley J, Merkley S, Pachal T, Gopal JV, Sharma D. Does potassium iodide application following silver diamine fluoride reduce staining of tooth? a systematic review. Aust Dent J 2020; 65(2):109-17. doi: 10.1111/adj.12743 [Crossref] [ Google Scholar]
- Yu OY, Mei ML, Zhao IS, Li QL, Lo EC, Chu CH. Remineralisation of enamel with silver diamine fluoride and sodium fluoride. Dent Mater 2018; 34(12):e344-e52. doi: 10.1016/j.dental.2018.10.007 [Crossref] [ Google Scholar]