Avicenna J Dent Res. 11(4):111-115.
doi: 10.34172/ajdr.2019.22
Original Article
Assessment of Parameters Influencing Physiologic Gingival Pigmentation Using a Novel Classification System
Saumya John 1, *  , K.V. Arun 2, Avaneendra Talwar 3, Prameetha George Ittycheria 4
, K.V. Arun 2, Avaneendra Talwar 3, Prameetha George Ittycheria 4  , Sunu Alice Cherian 5
, Sunu Alice Cherian 5  , Jasmine Clements 6
, Jasmine Clements 6
Author information:
1Department of Periodontics, Pushpagiri College of Dental Sciences, Thiruvalla, Kerala, India.
2Professor and Head of Department, Department of Periodontics, Ragas Dental College, Chennai, Tamil Nadu, India.
3Professor, Department of Periodontics, A.B Shetty Memorial Institute of Dental Sciences, Deralakatte, Mangalore, Karnataka, India.
4Senior Lecturer, Department of Periodontics, Pushpagiri College of Dental Sciences, Thiruvalla, Kerala, India.
5Lecturer, Department of Periodontics, Ragas Dental College, Chennai, Tamil Nadu, India.
6Ragas Dental College, Chennai, Tamil Nadu, India.
Abstract
Background: Depigmentation has become an important treatment modality among the general population due to the growing esthetic concern about the pigmentation. Previous studies have not considered parameters such as anatomical distribution of gingiva, intensity of pigmentation, and skin color in their classification systems. The purpose of this study was to assess physiologic gingival pigmentation in individuals based on certain gingival parameters and their correlation with skin color for better treatment strategies using a new classification system.
Methods: The study was carried out in Ragas Dental College using a cross-sectional design. A total of 112 female dental students were examined for skin color and gingival parameters. The facial gingiva of upper anterior teeth was assessed for gingival phenotype, intensity and distribution of pigmentation. Descriptive statistics were used to describe the data and the associations between variables were done using chi-square test (P < 0.05).
Results: It was found that skin color has a significant association with the intensity of pigmentation (P = 0.0001). In both dark and fair skinned individuals, Class II pigmentation (47%, 23.2%) with thick phenotype (62.5%, 35%) was most prevalent. Dark-skinned individuals were also found to have a generalized distribution of melanin pigmentation (19%) with high intensity of pigmentation (28.5%) predominantly. Fair-skinned individuals had a patchy distribution of melanin pigmentation with low intensity of pigmentation (37%).
Conclusions: The association of skin color with various parameters affecting gingival pigmentation can help in determining the depigmentation treatment strategies.
Keywords: Gingiva, Pigmentation, Phenotype, Esthetics, Laser
Copyright and License Information
© 2019 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: John S, Arun KV, Talwar A, Ittycheria PG, Cherian SA, Clements J. Assessment of Parameters Influencing Physiologic Gingival Pigmentation Using a Novel Classification System. Avicenna J Dent Res. 2019;11(4):111-115. doi: 10.34172/ajdr.2019.22.
Background
Highlights
-
Skin color significantly correlates with gingival pigmentation parameters.
-
An exclusive classification for physiologic gingival pigmentation was proposed.
-
It would aid in achieving a better outcome for depigmentation procedures.
Gingiva is a soft tissue that covers the alveolar process of the jaws and the cervical portion of the teeth. The color of the healthy gingiva is determined by numerous factors. The most important factors include degree of keratinization, epithelial thickness, oxygenation of blood, number and size of blood vessels, and the amount of pigments in the tissue (1). Carotene, melanin, reduced hemoglobin, and oxyhemoglobin are the main pigments contributing to the normal color of the gingiva, among which melanin is the most important factor (2-4).
Melanocytes in the epithelial basal cell layer convert tyrosine to melanin using enzyme tyrosinase, which is then stored in the basal cells in the form of melanosomes. It can also be found in the keratinocytes of gingival epithelium (2).Becker et al showed that melanocytes are present in oral mucous membranes under the microscope in both light and dark-complexioned individuals, even though no clinical evidence of pigmentation exists (5). Prinz reported an increased incidence of oral pigmentation in darker-complexioned individuals (6). The normal variations in physiologic pigmentation patterns are not associated with the quantity of melanocytes, instead they are associated with the activity of melanocytes in each individual (7,8). The development of pigmentation is genetically acquired, but the intensity of the pigmentation is often influenced by physical, hormonal, and chemical factors (9). The occurrence of gingival pigmentation does not have any gender or age-related predilection. It is found mostly in the incisor region and is observed less frequently in the posterior region (6).
Melanin pigmentation of the gingiva is not a medical problem. Complaints of “black gums” may cause esthetic problems and embarrassment when the pigmentation is noticed during speech and smiling (10,11). Seeking cosmetic therapy for melanin pigmentation is common and various methods including gingivectomy with free gingival autografting, chemical agents such as 90% phenol and 95% alcohol, electrosurgery, abrasion with diamond bur, cryosurgery, semiconductor diode laser, CO2 laser, Nd:YAG laser, and Er:Cr:YSGG laser have been used as treatment methods (12-22). The excision of the attached gingiva by “push back” procedure or gingival margin by gingivectomy can also be considered. However, proper case selection is essential for obtaining better results using depigmentation procedures and preventing recurrence.
According to Dummet et al, the color of healthy gingiva varies from pale-pink to bluish-purple (23). Between these limits of normalcy are a large number of colors, which primarily depend on the degree of epithelial cornification, intensity of the melanogenesis, arrangement of gingival vascularity, and the depth of epithelialization. Color variation may be uniform, unilateral, bilateral, mottled, macular, or blotched. Studying gingival color using the Munsell color system in dentistry, Ibusuki reported that gingival color varied with the position of the papillary, marginal, and attached gingivae (24).
In their review, Dummet and Barens divided oral mucosal pigmentation into the following categories: local and ethnicity pigmentation, oral pigmentary manifestations of systemic disease, pigmentary disturbances associated with pharmaceuticals and other chemicals, and benign and malignant neoplasm of pigmentary origin (7). According to Brocheriou et al, pigmented lesions of the oral cavity are of multiple origins.They can be classified as follows: non-tumoral pigmentation, non-melanin pigmented tumors, benign melanin pigmented tumors, and malignant melanomas (25). Peeran et al have also proposed an extensive classification and index for gingival pigmentation to assess the treatment needs of the patients (26). However, in an attempt to cover all aspects of gingival pigmentation, various aspects of physiologic gingival pigmentation crucial to treatment planning have not been covered.
Previous studies have not considered parameters such as anatomy of the gingiva, the intensity of pigmentation, and skin color in their classification systems. Therefore, the purpose of our study was to assess the patterns of physiologic gingival pigmentation in a population based on gingival phenotype, distribution, and intensity of pigmentation. Additionally, their correlation with skin color was investigated using a new classification system.
Materials and Methods
This cross-sectional study was conducted on 112 female dental students in the age group of 18-25 years at Ragas Dental College in Chennai, Tamil Nadu, India. The study protocol was approved by the Institutional Review Board of Ragas Dental College.
Systemically healthy adults with clinically healthy gingiva were included in the study. Those with periodontal diseases, hyperpigmentation that was associated with systemic diseases, drug use or malignancy, history of previous treatment of hyperpigmentation, and smoking history were excluded from the study.
Informed consent was obtained from all the participants after the purpose of the study was explained. The participants were examined using a mouth mirror and Williams probe under natural light for the various gingival parameters. Two examiners did the assessment to avoid any bias.
Assessment of Skin Color and Gingiva
The participants were divided into two groups based on their skin color as fair or dark. The fair-complexioned students included the lighter skin colored, wheatish and brown skin colored while the rest were classified as dark-complexioned individuals.
Gingival anatomy assessed for pigmentation was categorized as:
-
Class 1: Attached gingiva
-
Class 2: Attached gingiva and interdental papilla
-
Class 3: Attached gingiva, interdental papilla, and marginal gingiva
The distribution of melanin pigmentation was assessed as generalized or patchy. Generalized implied the presence of melanin in the gingiva uniformly throughout the entire segment. It was termed patchy when it was restricted to gingiva of few teeth.
The intensity of pigmentation based on skin color was categorized as either high or low. In high intensity, the pigmentation is more intense than the skin color and in low intensity, the pigmentation is less intense than the skin color.
The phenotype of the gingiva was assessed based on the transparency of the periodontal probe as thick or thin. It was graded as thick if the probe is not visible through the marginal gingiva and as thin when the probe is visible through the marginal gingiva.
The gingiva around the maxillary anterior teeth (canine to canine) was assessed which is most associated with gingival esthetics as described in Figure 1 (27).
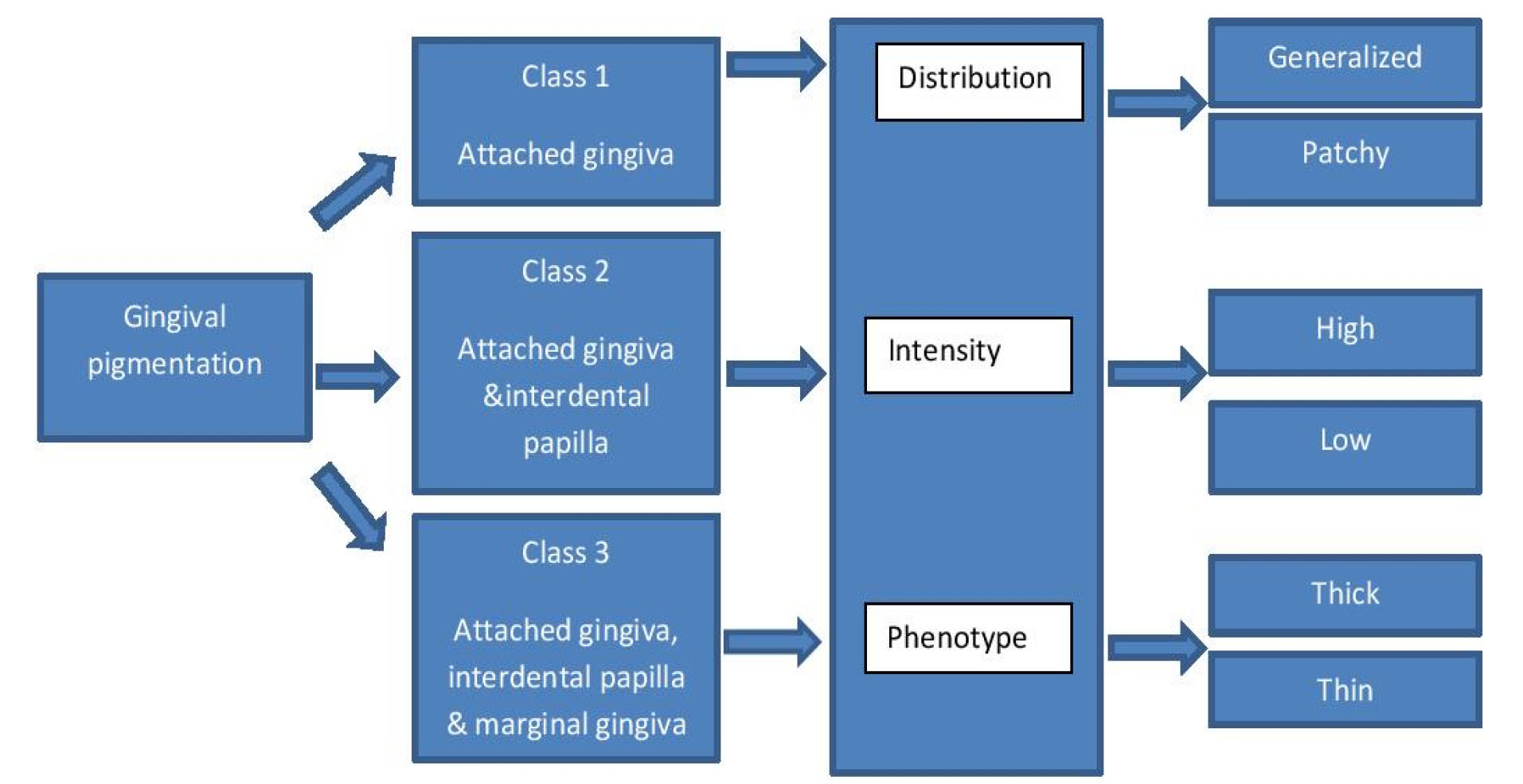
Figure 1.
Classification of Physiologic Gingival Pigmentation.
.
Classification of Physiologic Gingival Pigmentation.
Data Analysis
Data were entered and the statistical analysis was done using the SPSS software version 10.0.5. Chi-square test was used to find any association between skin color and gingival parameters. P> 0.05 was considered statistically significant.
Results
The mean age of the participants was 19.80 ± 2.0 years. Out of the 112 participants, 64.3% and 35.7% were fair and dark skinned, respectively. Class 2 pigmentation (79, 70.5%) with patchy distribution of melanin pigmentation (70, 62.5%), high intensity pigmentation (63, 56.2%), and thick phenotype (109, 97.3%) was more prevalent. Frequency distribution of skin color and patterns of gingival pigmentation are shown in Table 1. The association of skin color and intensity of pigmentation was found to be highly significant (P = 0.0001). The association of skin color and gingival pigmentation patterns are shown in Table 2.
Table 1.
Distribution of Skin Color and Patterns of Gingival Pigmentation (n=112)
|
Variables
|
No. (%)
|
| Skin color |
|
| Dark |
40 (35.7) |
| Fair |
72 (64.3) |
| Type of pigmentation |
|
| Class 1 |
20 (17.9) |
| Class 2 |
79 (70.5) |
| Class 3 |
13 (11.6) |
| Distribution of melanin pigmentation |
|
| Generalized |
42 (37.5) |
| Patchy |
70 (62.5) |
| Intensity of pigmentation |
|
| Low |
49 (43.8) |
| High |
63 (56.2) |
| Phenotype of the gingiva |
|
| Thick |
109 (97.3) |
| Thin |
3 (2.7) |
Table 2.
Association of Skin Color with Gingival Pigmentation Patterns
|
Patterns of gingival pigmentation
|
Fair (%)
|
Dark (%)
|
P
Value
|
| Type of Pigmentation |
|
|
0.11 |
| Class 1 |
14 (12.5) |
6 (5.4) |
| Class 2 |
53 (47.3) |
26 (23.2) |
| Class 3 |
5 (4.5) |
8 (7.1) |
| Distribution of melanin pigmentation |
|
|
0.24 |
| Generalized |
21 (18.8) |
21 (18.8) |
| Patchy |
51 (45.5) |
19 (16.9) |
| Intensity of pigmentation |
|
|
0.0001 |
| Low |
41 (36.6) |
8 (7.1) |
| High |
31 (27.7) |
32 (28.6) |
| Phenotype of the gingiva |
|
|
1.0 |
| Thick |
2 (1.8) |
1(0.9) |
| Thin |
70 (62.5) |
39 (34.8) |
Discussion
Previous studies have classified skin color as fair, wheatish, brown, and dark which might be difficult to assess by clinicians. Hence, the skin color was classified as fair and dark, as it might be easier to replicate while planning depigmentation procedures.
Dummet-Gupta Oral Pigmentation Index (DOPI) has been used by most authors until now to assess parameters affecting gingival pigmentation. However, this index can lead to subjective variation (23). Hence, to avoid that variation, there was a need to classify the intensity of pigmentation either as ‘high’ or ‘low’ by two examiners. Objective assessment using spectrometric analysis is not economical and it is difficult to carry out in a dental office.
Ponnaiyan et al defined 6 classes of gingival pigmentation based on the anatomic distribution and used DOPI to assess the intensity of pigmentation (28,29). This might be cumbersome for clinicians to follow and liable to errors in treatment planning. The classification proposed in this study covers all aspects of physiological gingival pigmentation and it is comparatively easier to follow.
There is a need for relating gingival pigmentation to skin color, intensity of gingival pigmentation, distribution of pigmentation and gingival phenotype as this could help us to decide on treatment options. Hence, the participants were screened for gingival parameters influencing the outcome of depigmentation procedures and their correlations with the skin color were assessed. In this study, we have found that there is a highly significant association between skin color and the intensity of pigmentation, distribution of pigmentation, and the gingival phenotype (P < 0.01), which is similar to previous studies.
Class 2 pigmentation (involving attached gingiva and interdental papilla) has been most commonly found in both fair and dark skinned subjects, which is similar to previous studies in the Indian population (28-30). Ponnaiyan et al has reported mild pigmentation to be predominant in fair individuals. In the current study, Class 2 pigmentation followed by Class 1 pigmentation (involving only attached gingiva) with both high and low intensity of pigmentation was found in fair-skinned individuals (28,29).
In this study, Class 3 pigmentation (involving all three parts of gingiva) correlated with a high intensity, generalized type of distribution and thick phenotype was more prevalent in dark individuals, which is similar to previous studies (30).
One of the major drawbacks of depigmentation procedures is the recurrence of pigmentation. The intensity and distribution of pigmentation are crucial for determining repigmentation as stated by Kumaraswamy (31). Recurrence of pigmentation occurs due to the migration of active melanocytes from areas adjacent to the treated site (32).Therefore, in patients with Class 1 and Class 2 pigmentation with a patchy distribution and low intensity, the procedure would probably give the best results. The recurrence rate comparatively reduced due to the decreased number of melanocytes in these sites.
In this study, very few individuals were found with a thin gingival phenotype which might be due to the small sample size of the population. Thin phenotype is one of the parameters to be considered because the depigmentation procedure itself can cause denudation of gingival tissue in these cases. Gingival augmentation using free gingival grafts from non-pigmented sites would be most beneficial in patients with thin gingival phenotype as the gingiva formed would mimic the properties of the donor site (12).
More studies are recommended over a wide geographic area with a larger sample size including both genders. This study was carried out in females only as they are comparatively more concerned about their esthetic appearance and more inclined to undergo depigmentation procedures.
Conclusions
Class 2 pigmentation (present in attached gingiva and interdental papilla) with high intensity, patchy distribution, and a thick phenotype was more prevalent. Moreover, the association of skin color has been found to be highly significant with the intensity of pigmentation. Anatomical delineation of gingival pigmentation and their contributory factors can help design therapeutic strategies.
Conflict of Interest Disclosures
The authors declare that they have no conflict of interest.
Acknowledgements
The authors are extremely grateful to Dr. T.S.S. Kumar at Ragas Dental College for his support in carrying out the study.
Ethical Statement
The present study was carried out in accordance with the Helsinki Declaration of 1975, revised in 2002. This study protocol was approved by the Institutional Review Board of Ragas Dental College. The objectives of this study were explained to the subjects prior to commencement of the study and their data were kept confidential. A detailed informed consent was obtained from all the subjects.
Authors’ Contribution
KVA and AT developed the concept and design of the study and contributed to the supervision of the project. The acquisition of data was carried out by SJ and JC. The analysis and interpretation of data were carried out by SAC and PGI. All authors have read and approved the final manuscript.
References
- McCarthy PL, Shklar G. Diseases of the Oral Mucosa. 2nd ed. Philadelphia, PA: Lea & Febiger; 1980. p. 27.
- Dummett CO. First symposium on oral pigmentation. J Periodontol 1960; 31(5):345. doi: 10.1902/jop.1960.31.5.345 [Crossref] [ Google Scholar]
- Goldzieher JW, Roberts IS, Rawls WB, Goldzieher MA. Chemical analysis of the intact skin by reflectance spectrophotometry. AMA Arch Derm Syphilol 1951; 64(5):533-48. doi: 10.1001/archderm.1951.01570110003001 [Crossref] [ Google Scholar]
- Dummett CO, Barens G. Pigmentation of the oral tissues: a review of the literature. J Periodontol 1967; 38(5):369-78. doi: 10.1902/jop.1967.38.5.369 [Crossref] [ Google Scholar]
- Becker SW. Melanin pigmentation: a systematic study of the pigment of the human skin and upper mucous membranes, with special consideration of pigmented dendritic cells. Arch Derm Syphilol 1927; 16(3):259-90. doi: 10.1001/archderm.1927.02380030002001 [Crossref] [ Google Scholar]
- Prinz H. Pigmentation of the oral mucous membrane. Dental Cosmos 1932; 72:554-61. [ Google Scholar]
- Dummett CO, Barens G. Oromucosal pigmentation: an updated literary review. J Periodontol 1971; 42(11):726-36. doi: 10.1902/jop.1971.42.11.726 [Crossref] [ Google Scholar]
- van Wyk CW. Mouth pigmentation patterns in a group of healthy South African Bantu. S Afr Med J 1970; 44(7):177-80. [ Google Scholar]
- Dummett CO. Clinical observations on pigment variations in healthy oral tissues of the Negro. J Dent Res 1945; 24(1):7-13. doi: 10.1177/00220345450240010701 [Crossref] [ Google Scholar]
- Dummett CO, Sakumura JS, Barens G. The relationship of facial skin complexion to oral mucosa pigmentation and tooth color. J Prosthet Dent 1980; 43(4):392-6. doi: 10.1016/0022-3913(80)90207-3 [Crossref] [ Google Scholar]
- Hoexter DL. Periodontal aesthetics to enhance a smile. Dent Today 1999; 18(5):78-81. [ Google Scholar]
- Tamizi M, Taheri M. Treatment of severe physiologic gingival pigmentation with free gingival autograft. Quintessence Int 1996; 27(8):555-8. [ Google Scholar]
- Dello Russo NM. Esthetic use of a free gingival autograft to cover an amalgam tattoo: report of case. J Am Dent Assoc 1981; 102(3):334-5. doi: 10.14219/jada.archive.1981.0036 [Crossref] [ Google Scholar]
- Gnanasekhar JD, al-Duwairi YS. Electrosurgery in dentistry. Quintessence Int 1998; 29(10):649-54. [ Google Scholar]
- Tal H, Landsberg J, Kozlovsky A. Cryosurgical depigmentation of the gingiva A case report. J Clin Periodontol 1987; 14(10):614-7. doi: 10.1111/j.1600-051x.1987.tb01525.x [Crossref] [ Google Scholar]
- Yeh CJ. Cryosurgical treatment of melanin-pigmented gingiva. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998; 86(6):660-3. doi: 10.1016/s1079-2104(98)90199-8 [Crossref] [ Google Scholar]
- Hasegawa A, Okagi H. Removing melagenous pigmentation using 90 percent phenol with 95 percent alcohol. Dent Outlook 1973; 42:673-6. [ Google Scholar]
- Bishop K. Treatment of unsightly oral pigmentation: a case report. Dent Update 1994; 21(6):236-7. [ Google Scholar]
- Atsawasuwan P, Greethong K, Nimmanon V. Treatment of gingival hyperpigmentation for esthetic purposes by Nd:YAG laser: report of 4 cases. J Periodontol 2000; 71(2):315-21. doi: 10.1902/jop.2000.71.2.315 [Crossref] [ Google Scholar]
- Yousuf A, Hossain M, Nakamura Y, Yamada Y, Kinoshita J, Matsumoto K. Removal of gingival melanin pigmentation with the semiconductor diode laser: a case report. J Clin Laser Med Surg 2000; 18(5):263-6. doi: 10.1089/clm.2000.18.263 [Crossref] [ Google Scholar]
- Nakamura Y, Hossain M, Hirayama K, Matsumoto K. A clinical study on the removal of gingival melanin pigmentation with the CO(2) laser. Lasers Surg Med 1999; 25(2):140-7. doi: 10.1002/(sici)1096-9101(1999)25:2<140::aidlsm7>3.0.co;2-7. [Crossref] [ Google Scholar]
- Gholami L, Ansari Moghaddam S, Rigi Ladiz MA, Molai Manesh Z, Hashemzehi H, Fallah A. Comparison of gingival depigmentation with Er,Cr:YSGG laser and surgical stripping, a 12-month follow-up. Lasers Med Sci 2018; 33(8):1647-56. doi: 10.1007/s10103-018-2501-1 [Crossref] [ Google Scholar]
- Dummett CO, Gupta OP. The DOPI assessment in gingival pigmentation. IADR program and Abstracts of papers. 1966. p 122,.
- Ibusuki M. The color of gingiva studied by visual color matching Part II Kind, location, and personal difference in color of gingiva. Bull Tokyo Med Dent Univ 1975; 22(4):281-92. [ Google Scholar]
- Brocheriou C, Kuffer R, Verola O. [Pigmented lesions of the oral cavity]. Ann Pathol 1985; 5(4-5):221-9. [ Google Scholar]
- Peeran SW, Ramalingam K, Peeran SA, Altaher OB, Alsaid FM, Mugrabi MH. Gingival pigmentation index proposal of a new index with a brief review of current indices. Eur J Dent 2014; 8(2):287-90. doi: 10.4103/1305-7456.130640 [Crossref] [ Google Scholar]
- Kokich VG. Esthetics: the orthodontic-periodontic restorative connection. Semin Orthod 1996; 2(1):21-30. doi: 10.1016/s1073-8746(96)80036-3 [Crossref] [ Google Scholar]
- Ponnaiyan D, Gomathy L, Anusha J. The correlation of skin color and gingival pigmentation patterns in a group of South Indians in Tamil Nadu, India. SRM J Res Dent Sci 2013; 4(2):54-8. doi: 10.4103/0976-433x.120178 [Crossref] [ Google Scholar]
- Ponnaiyan D, Jegadeesan V, Perumal G, Anusha A. Correlating skin color with gingival pigmentation patterns in South Indians - a cross sectional study. Oral Health Dent Manag 2014; 13(1):132-6. [ Google Scholar]
- Rakhewar PS, Patil HP, Thorat M. Identification of gingival pigmentation patterns and its correlation with skin color, gender and gingival phenotype in an Indian population. Indian J Multidiscip Dent 2016; 6(2):87-92. doi: 10.4103/2229-6360.197763 [Crossref] [ Google Scholar]
- Kumaraswamy A. Beauty is indeed skin deep. Ann Plast Surg 1980; 4(6):462-8. [ Google Scholar]
- Perlmutter S, Tal H. Repigmentation of the gingiva following surgical injury. J Periodontol 1986; 57(1):48-50. doi: 10.1902/jop.1986.57.1.48 [Crossref] [ Google Scholar]