Avicenna J Dent Res. 11(2):41-47.
doi: 10.34172/ajdr.2019.08
Original Article
Effect of 5 Oral Hygiene Teaching Methods on Orthodontic Patients: A Single-Blind Randomized Controlled Clinical Trial
Mohammad Karim Soltani 1  , Farhad Jafari 1, Mojgan Taheri 2, *
, Farhad Jafari 1, Mojgan Taheri 2, *  , Ali Reza Soltanian 3, Masoumeh Khoshhal 4, Sima Torkaman 5
, Ali Reza Soltanian 3, Masoumeh Khoshhal 4, Sima Torkaman 5
Author information:
1Department of Orthodontics, Faculty of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran
2Department of Operative Dentistry, Dental School, Hamadan University of Medical Sciences, Hamadan, Iran
3Department of Biostatistics and Epidemiology, School of Public Health, Hamadan University of Medical Sciences, Hamadan, Iran
4Department of Periodontics, School of Dental Medicine, Hamadan University of Medical Sciences, Hamadan, Iran
5Resident of Pediatric Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran
Abstract
Background: The aim of the present study was to determine the most effective oral hygiene method in fixed orthodontic patients.
Methods: A total of 125 patients who had recently started their orthodontic treatment and had not received oral hygiene instructions were randomly assigned to 5 groups (n=25): verbal instructions (V), verbal instructions plus pamphlet (V+P), verbal instructions plus video film (V+F), verbal instructions plus the use of disclosing agents (V+D), and pamphlet plus the use of disclosing agents (P+D). One week after the installation of orthodontic appliance, plaque index (PI) and gingival index (GI) were recorded and oral hygiene instructions were provided. One week and 4 weeks after oral hygiene instructions, PI and GI were recorded again.
Results: PI and GI showed significant decreases in 5 groups after 1 week and 4 weeks (P ˂ 0.05). No statistically significant differences were detected between the 5 study groups in terms of plaque reduction after one week. However, after 4 weeks PI values were significantly lower in V+D group compared to P+D group. Regarding GI, V+D method resulted in a significantly lower GI than P+D after 1 week and 4 weeks.
Conclusions: To sum up, all the oral hygiene motivation methods applied in this study can be effective in decreasing PI and GI. However, it appears that the best way is the verbal oral hygiene instruction plus the use of disclosing agents.
Keywords: Oral hygiene motivation, Plaque control, Orthodontic patient
Copyright and License Information
© 2019 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Soltani MK, Jafari F, Taheri M, Soltanian AR, Khoshhal M, Torkaman S. Effect of 5 Oral Hygiene Teaching Methods on Orthodontic Patients: A Single-Blind Randomized Controlled Clinical Trial. Avicenna J Dent Res. 2019;11(2):41-47. doi: 10.15171/ajdr.2019.08.
Background
Highlights
-
All the teaching methods presented in our study were effective in improving oral hygiene in orthodontic patients.
-
Plaque index values were significantly lower in “verbal instructions plus the use of disclosing agents” group compared to “pamphlet plus the use of disclosing agents” group.
-
Regarding gingival index, “verbal instructions plus the use of disclosing agents” resulted in a significantly lower gingival index than “pamphlet plus the use of disclosing agents”.
Poor oral hygiene is one of the common problems in orthodontic patients. Fixed orthodontic appliances with attachments like bands, brackets, arch wires, springs, and other hardware increase the retention of plaque, along with making tooth cleaning more difficult (1,2). In addition, fixed orthodontic appliances are considered an external interference that could affect the microflora of the oral cavity and increase the levels of cariogenic bacteria like Streptococcus mutans and Lactobacillus spp. (3-5).
Accumulation of bacterial plaque predisposes the orthodontic patient to enamel decalcification, dental caries, and gingivitis (6-10).
Numerous studies have examined various methods to prevent these problems. Use of fluoride has been effective in the prevention of dental caries (11).
The effect of using different forms of fluoride has also been investigated in several studies (12). Plaque control is the most important way to prevent problems above mentioned. Therefore, various methods of health education should be considered for plaque control (2).
The use of chlorhexidine and different mouthwashes like herbal and synthetic mouthwashes as a chemical plaque control method have been studied in orthodontic patients (13,14).
Furthermore, a plethora of literature has compared different plaque removal devices. The effectiveness of using various devices such as dental floss (15,16), different bristle designs of toothbrushes (17), interdental toothbrushes (18,19), different types of interdental devices (20), electric toothbrushes (21), and water-jet (22) has been evaluated in orthodontic patients in many studies. Nonetheless, it seems that the main problem is the patient’s motivation. Rigau-Gay et el assessed the efficacy of a single inspirational interview in increasing the oral sanitation in orthodontic patients in comparison with conventional training alone. Obtained data exhibited an instant improvement in the oral sanitation which persisted through the 6-month follow-up (23).
Several studies have designed different teaching methods for oral hygiene in orthodontic patients and compared them (1,2). Daily text messages appear to be an effective reminder for oral hygiene than weekly text messages. Teenagers are the main generally-treated patients in orthodontics; therefore, agreement is mainly important for teenagers. Text messages are a convenient mode of communication that is widely used for teenagers and provides a means of growing compliance (24). Another study showed that oral hygiene status improved with text message reminder (25). Moreover, computer-based oral hygiene program is suggested to be more effective in giving ideal oral health status compared to the conventional technique in the patients with fixed orthodontic appliances (26). Therefore, the aim of this study was to design different teaching methods for oral hygiene in orthodontic patients and compare them to achieve an optimal oral health status.
Methods
This clinical trial was conducted in 2 private orthodontic clinics in Hamadan, Iran (between March 2013 and November 2013). The study was registered in Iranian Registry of Clinical Trials (identifier: IRCT20190122042457N1; https://www.irct.ir/trial/37162). A total of 125 orthodontic patients (87 females and 38 males in the age range of 12-26 years) were included in the present study according to the following criteria: 1) the patients had never received any special oral health instructions, 2) the patients did not have any learning problems, 3) patients had at least 24 teeth, 4) patients had no systemic disease like diabetes that may have affected their periodontal conditions, and 5) examined teeth should have been existed in the mouth, not been extracted or missed. Then, any tooth examined in this study had not facial or cervical restoration.
Lack of patient cooperation in principles of education and failure in follow-up or referral appointments led to the exclusion of some patients from the study. Moreover, if poor oral hygiene caused severe acute gingivitis, the patient should have been excluded from the study and referred to a periodontist.
Similar brackets (American Orthodontics Company) were bonded by the same orthodontic adhesive (3M-Unitek light-cured) for all the patients. The same type of orthodontic toothbrushes (Procter & Gamble, Weybridge, UK), interdental brushes (Procter & Gamble, Weybridge, UK), super floss, and fluoride mouthwashes (Procter & Gamble, Weybridge, UK) were also provided.
Estimation of Sample Size
The initial results of a pilot study revealed that the average correlation coefficient between plaque index (PI) before and after the intervention (1 week and 4 weeks after training) in the section was about 30% (R = 0.3). Moreover, in an early study, each case was measured three times (at baseline, 1 week, and 4 weeks after training). Therefore, according to the following formula (No 1), 25 patients were required in each group to evaluate the proposed goals.
Note that the standard deviation of the PI was determined by an average of 22 and the maximum permissible error was assumed to be 5%.
Average correlation coefficient: R = 0.3
The maximum permissible error: D = 5%
Total number of measurements: M = 3
The power of study: equal to 90%
The critical number is proportional to the error of the first kind (
)
Five oral hygiene instruction methods were designed in this study: verbal instructions on a model (V), verbal instructions on a model plus a pamphlet (V + P), verbal instructions on a model plus video film (V + F), verbal instructions on a model plus the use of disclosing agents (V + D), and a pamphlet plus the use of disclosing agents (P + D). The subjects in all the groups received the program on oral hygiene procedures from a trained dental student (Figure 1).
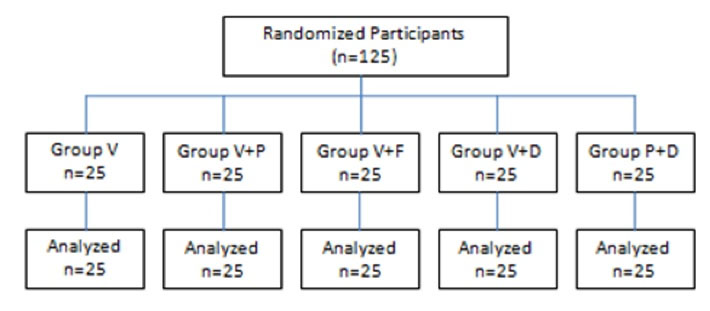
Figure 1.
Flow Diagram of the Study.
.
Flow Diagram of the Study.
One week after installation of the braces, PI and GI were measured as baseline values and then the patients randomly received one of the methods of oral hygiene instructions. To divide participants into 5 groups, simple randomization methods were used in this study. To this end, the simple randomization sequences were generated and participants were allocated to the groups based on the sequence. PI and GI were scored on the basis of 6 teeth, upper right central incisor, lower left central incisor, and first premolars. Second premolars were scored in cases with extracted first premolars. PI was based upon that of Greene & Vermillion (27) and Lees and Rock’ (2) grid used to record plaque score. After applying the disclosing agents, the teeth were rinsed and the plaque was examined in presumed boxes around the bracket, as shown in gray in Figure 1. These boxes were imaged by dividing the tooth by horizontal and vertical third lines while bracket was assumed in the center (2). A score of 0 to 3 was assigned for 5 boxes of each tooth; score 0 when there was no plaque on the box, 1 when some plaque covered the box, 2 when plaque covered most of the box, and 3 when the whole box was covered with plaque. Therefore the maximum score of PI for each patient was 90 (Figure 2).
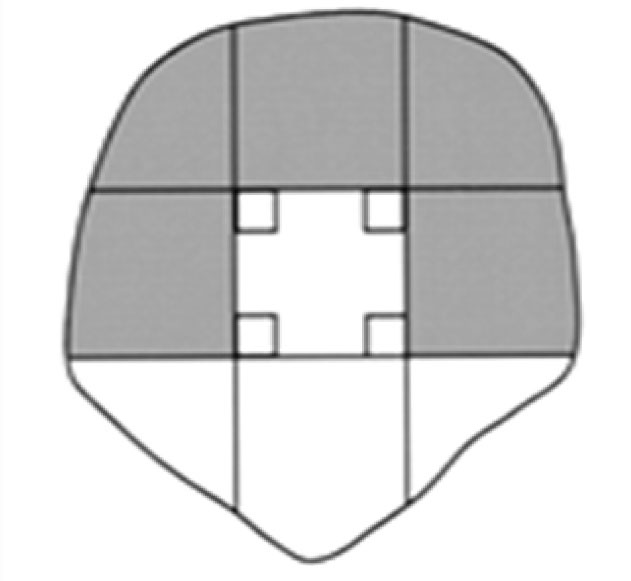
Figure 2.
Areas of Pl aque Measurement Around Bracket
.
Areas of Pl aque Measurement Around Bracket
The GI based on Löe and Silness (28) was recorded after gently probing the gingiva with a WHO probe (NOVA, CPITN-C PROBE, N0063-R, LONDON, England). Distobuccal, mid-buccal, and mesio-buccal areas of teeth were evaluated. Score 0 was considered for the normal gingiva, 1 for mild gingival inflammation without bleeding on probing, 2 for moderate gingival inflammation with bleeding on probing, and 3 for severe gingival inflammation with spontaneous bleeding. The study design was single-blind; therefore, PI and GI were measured by another examiner who was previously explained about the study. Patients below 18 years of age were given training in the presence of their parents. Patients randomly received one of the 5 oral health education techniques abovementioned.
Pamphlets and films were specifically designed for this study. The film included 11 minutes of special oral hygiene instructions for orthodontic patients. The script was based on the information included in the pamphlet: the effect of orthodontic treatment on oral health, explanation about the microbial nature of plaque and its effect on teeth and gums, effective plaque removal by orthodontic toothbrushes, interdental brushes, super floss, and instructions for the use of fluoride mouthwash.
Statistical Analysis
Paired t test was used to compare the means of PI and GI at different times. One-way ANOVA was used to compare the groups and post hoc Tukey test was used for two-by-two comparisons of the groups. To evaluate the normal distribution of quantitative variables, one-sample Kolmogorov-Smirnov test was used. In addition, Levene test was used to evaluate the homogeneity. Repeated measures test with greenhouse-Geisser correction was used to analyze the GI, and repeated measures test with sphericity assumption was used to analyze the PI.
Statistical analysis was performed by SPSS version 16.0 (SPSS Inc., Chicago, IL), and based on intention-to-treat strategy. Statistical significance was considered less than 0.05.
Results
In this study, 125 subjects (38 males and 87 females) participated with a mean age of 17.01 ± 4.27. The mean PI and GI at the baseline, and after 1 and 4 weeks are shown in Figures 3 and 4. Furthermore, the mean PI and GI for both genders at baseline, and 1 week and 4 weeks after the health education are shown, respectively, in Table 1 (sex was not a significant variable in the repeated measures test).
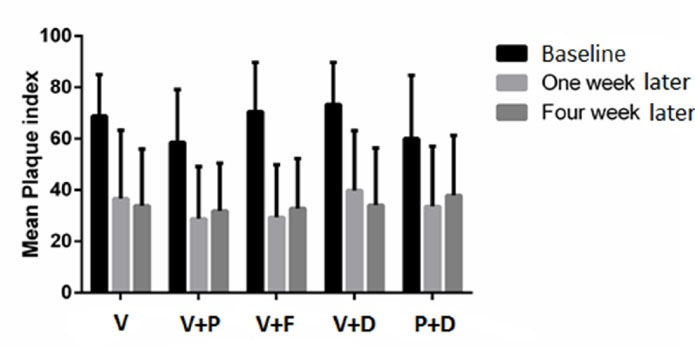
Figure 3.
The Mean Plaque Index in Each Group at the Baseline, and After 2 and 4 Weeks.
Note. Verbal instructions (V), verbal instructions plus pamphlet (V + P), verbal instructions plus video film (V + F), verbal instructions plus the use of disclosing agents (V + D), and pamphlet plus the use of disclosing agents (P + D).
.
The Mean Plaque Index in Each Group at the Baseline, and After 2 and 4 Weeks.
Note. Verbal instructions (V), verbal instructions plus pamphlet (V + P), verbal instructions plus video film (V + F), verbal instructions plus the use of disclosing agents (V + D), and pamphlet plus the use of disclosing agents (P + D).
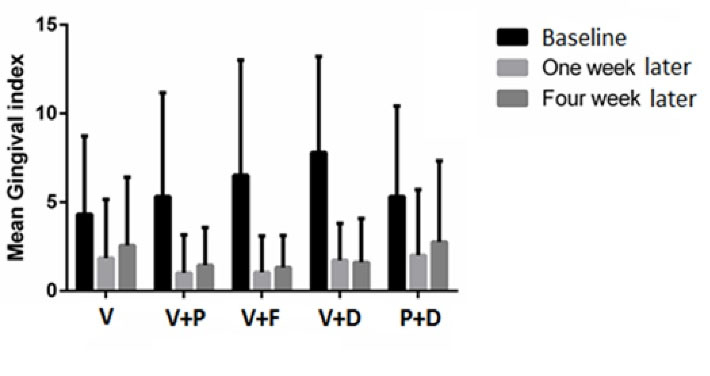
Figure 4.
The Mean Gingival Index in Each Group at the Baseline, and After 1 and 4 Weeks.
Note. Verbal instructions (V), verbal instructions plus pamphlet (V + P), verbal instructions plus video film (V + F), verbal instructions plus the use of disclosing agents (V + D), and pamphlet plus the use of disclosing agents (P + D).
.
The Mean Gingival Index in Each Group at the Baseline, and After 1 and 4 Weeks.
Note. Verbal instructions (V), verbal instructions plus pamphlet (V + P), verbal instructions plus video film (V + F), verbal instructions plus the use of disclosing agents (V + D), and pamphlet plus the use of disclosing agents (P + D).
Table 1.
The Mean Plaque Index and Gingival Index
|
Sex
|
Baseline
|
One Week Later
|
Four Weeks Later
|
|
Plaque index
|
|
|
|
| Female |
62.12 ± 19.08 |
31.08 ± 21.99 |
30.72 ± 19.27 |
| Male |
75.78 ± 19.63 |
39.55 ± 24.29 |
41.78 ± 23.03 |
|
Gingival index
|
|
|
|
| Female |
4.70 ± 4.96 |
1.08 ± 2.08 |
1.62 ± 2.58 |
| Male |
8.5 ± 5.93 |
2.52 ± 3.69 |
2.65 ± 4.12 |
One-sample Kolmogorov-Smirnov test and Levene test showed that the variables had a normal distribution and were also homogeneous. Before education, no significant differences were observed between the study groups in terms of PI and GI values (P ˂ 0.05).
Plaque Index
After 1 week, significant decreases were observed in all groups in terms of PI compared to the baseline (P ˂ 0.05). Whilst differences were not significant between the 5 groups regarding the plaque reduction after this period. The mean changes of PI among the groups were as follows: P + D ˂ V + P ˂ V ˂ V + D ˂ V + F.
Furthermore, after 4 weeks, significant decreases were seen in all groups in terms of PI compared to the baseline (P ˂ 0.05). The mean changes in PI values among five groups after 4 weeks compared to the baseline were as follows: P + D ˂ V + P ˂ V ˂ V + F ˂ V + D. After 4 weeks, one-way ANOVA revealed significant effects of interactions at P = 0.036 level on PI compared to the baseline, and Tukey test showed a difference between the V + D and P + D groups. Comparison of PI one and four weeks after the instruction showed no significant difference between the 5 study groups (P>0.05) (Figure 3).
Note. Verbal instructions (V), verbal instructions plus pamphlet (V + P), verbal instructions plus video film (V + F), verbal instructions plus the use of disclosing agents (V + D), and pamphlet plus the use of disclosing agents (P + D).
Table 2 shows the comparisons of PI over time and between groups based on the repeated-measures test assuming sphericity. According to the results, changes showed a decreasing trend over time (P < 0.001). But this downward trend was not significantly different between groups (P = 0.079).
Table 2.
Comparisons of Plaque Index Over Time and Between Groups
|
Time
|
Group
|
Mean (SD)
|
F (Time*Group)
|
P
Value
|
| Baseline |
V |
68.88 ± 16.04 |
1.79 |
0.079 |
| V + P |
58.56 ± 20.58 |
|
|
| V + F |
70.56 ± 19.13 |
|
|
| V + D |
73.40 ± 16.34 |
|
|
| P + D |
60.00 ± 24.69 |
|
|
| One week later |
V |
36.68 ± 26.57 |
|
|
| V + P |
28.80 ± 20.28 |
|
|
| V + F |
29.40 ± 20.48 |
|
|
| V + D |
39.80 ± 23.35 |
|
|
| P + D |
33.60 ± 23.42 |
|
|
| Four weeks later |
V |
33.84 ± 22.10 |
|
|
| V + P |
31.84 ± 18.65 |
|
|
| V + F |
32.80 ± 19.50 |
|
|
| V + D |
34.16 ± 22.23 |
|
|
| P + D |
37.84 ± 23.48 |
|
|
|
|
|
|
F (time) |
180.35 |
|
|
|
|
P-value |
<0.001 |
Gingival Index
One and 4 weeks after the trainings, GI significantly decreased compared to the baseline values in all groups (P˂ 0.05). When comparing the 5 groups, ANOVA showed significant differences after 1 week (P = 0.047) and 4 weeks (P = 0.02).
Moreover, Tukey test revealed that groups V and V + D had significant differences in terms of gingival scores after both time points, namely 1 week and 4 weeks. The mean changes of GI between the groups, 1 week and 4 weeks after oral instruction compared to the baseline, were as follows: V ˂ P + D ˂ V + P ˂ V + F ˂ V + D (Figure 4).
Table 3 shows the comparisons of GI over time and between groups based on the repeated-measures test with Greenhouse-Geisser correction. According to the results, changes had a decreasing trend over time (P < 0.001). And this downward trend was significantly different between the groups (P = 0.018).
Table 3.
Comparisons of Gingival Iindex Over Time and Between Groups
|
Time
|
Group
|
Mean (SD)
|
F (Time*Group)
|
P
Value
|
| Baseline |
V |
4.32 ± 4.41 |
2.73 |
0.018 |
| V + P |
5.32 ± 5.85 |
|
|
| V + F |
6.52 ± 6.49 |
|
|
| V + D |
7.80 ± 5.40 |
|
|
| P + D |
5.32 ± 5.10 |
|
|
| One week later |
V |
1.84 ± 3.31 |
|
|
| V + P |
1.00 ± 2.16 |
|
|
| V + F |
1.04 ± 2.05 |
|
|
| V + D |
1.72 ± 2.09 |
|
|
| P + D |
2.00 ± 3.71 |
|
|
| Four weeks later |
V |
2.56 ± 3.84 |
|
|
|
|
V + P |
1.44 ± 2.12 |
|
|
| V + F |
1.32 ± 1.80 |
|
|
| V + D |
1.60 ± 2.48 |
|
|
| P + D |
2.76 ± 4.57 |
|
|
|
|
|
|
F (time) |
82.50 |
|
|
|
|
P-value |
<0.001 |
Discussion
Improving oral hygiene in orthodontic patients has been investigated in a plethora of previous studies. These studies have examined the effects of various mechanical devices and chemical materials, however motivation and the effect of training methods in the patients have become more important recently. Motivational methods applied in the studies could be commonly categorized including message reminders, behavioral modification, and chairside education. Chairside oral hygiene instruction was the most frequently used method for increasing the motivation of oral hygiene. Verbal and written data, pictures or catalogs, videos, and visual appliances were applied by researchers to describe the mechanism of plaque formation, alert the danger of poor oral hygiene, and recommend brushing techniques (23,29,30).
The best ways people learn may be different and no single instructional method suits all the learners (1,31). It seems that the most common method of oral hygiene education in a modern orthodontic clinic is face-to-face training. In this technique, patients will have better learning opportunities. However, it appears that face-to-face training is not sufficient alone to persuade orthodontic patients to achieve good oral hygiene. Maybe that is why oral hygiene problems like multiple dental caries, gingivitis, and white spots are still common in patients with fixed orthodontics (7,10,32). Dentists are required to provide oral hygiene instructions and motivate patients to achieve optimal health and prevent the problems abovementioned (33,34). Therefore, different conventional methods in health education were compared in this study.
In the present study, different groups were designed aimed at reinforcing face-to-face training. Thus, the main methods including written instructions, video films (31,35), and disclosing agents (36,37) were added to the verbal instructions. These materials are practical and popular for educational purposes.
All the oral hygiene techniques used in this study were effective in decreasing plaque and gingivitis after 1 week and 4 weeks. However, the results showed that V + D was more effective in eliminating plaque and decreasing GI scores than the other techniques.
Boyd showed that use of disclosing agents can be effective in self-monitoring the plaque control in the orthodontic patients (36). This result supports ours in that disclosing agents change the color of plaque and provide the direct observation of plaque by patients for their own assessment. Therefore, disclosing agents can be effective in motivating patients. However, contrary to the results of the present study, Tan and Wade found no significant difference in the improvement of plaque control between the group who received only individual oral hygiene instructions and another group who received the same oral hygiene instructions supplemented with the home use of a disclosing agent. They concluded that repeated oral hygiene education seems to be the most important feature in patient motivation (37).
The mean PI in 125 patients before receiving oral hygiene instructions was 74%, meaning poor oral hygiene based on Greene and Vermillion (27). After education, PI reached to 37% which implies moderate oral hygiene. However, one study indicated that the mean PI in patients without orthodontic appliance was 34% before oral hygiene education (38). This indicates that orthodontic patients not receiving oral hygiene instructions may have worse oral health than patients without orthodontic appliances.
In a study on the effect of orthodontic treatment on gingivitis, Davies et al reported that girls have better oral hygiene and lower PI and GI than boys (39). Moreover, the present study demonstrated that the mean PI and GI were lower in girls before and after oral health instructions, though not statistically significant. Our findings were also in accordance with a previous study by Kudirkaite et al on oral hygiene among adolescents with fixed orthodontic appliances (40).
Many studies have demonstrated that plaque accumulates again after removal and reinforcement by appropriate methods is necessary. Since verbal instruction at each visit is costly and time-consuming (41), reinforcement of verbal instruction is beneficial for the patients and practitioners.
Conclusions
To sum up, all the training methods presented in our study were effective in improving oral hygiene in orthodontic patients. Further, it was shown that verbal instructions on a model plus the use of disclosing agents (V + D) and pamphlet plus the use of disclosing agents (P + D) were the most and the least effective methods in decreasing PI, respectively. Moreover, considering the improvement of gingival condition, verbal instructions on a model plus the use of disclosing agents (V + D) was the most appropriate method and verbal instructions on a model method (V) was the least.
Authors’ Contribution
MKS, FJ and MK have contributed to the conception and design of the study. MT and ST contributed to the data collection and drafted the manuscript. The statistical analyses and interpretation of data were carried out by ARS. All the authors have read and approved the final manuscript.
Ethical Statement
The study protocol was approved by the Ethics Committee of Hamadan University of Medical Sciences.
Conflict of Interest Disclosures
None of the authors have any conflicts of interest.
Acknowledgments
This investigation is part of a thesis by Mojgan Taheri, which was approved and financially supported by the Vice Chancler of Research and Technology Center of Hamadan University of Medical Sciensec, Hamadan, Iran.
References
- Ay ZY, Sayin MO, Özat Y, Goster T, Atilla AO, Bozkurt FY. Appropriate oral hygiene motivation method for patients with fixed appliances. Angle Orthod 2007; 77(6):1085-9. doi: 10.2319/101806-428.1 [Crossref] [ Google Scholar]
- Lees A, Rock WP. A comparison between written, verbal, and videotape oral hygiene instruction for patients with fixed appliances. J Orthod 2000; 27(4):323-8. doi: 10.1093/ortho/27.4.323 [Crossref] [ Google Scholar]
- Alves PV, Alviano WS, Bolognese AM, Nojima LI. Treatment protocol to control Streptococcus mutans level in an orthodontic patient with high caries risk. Am J Orthod Dentofacial Orthop 2008; 133(1):91-4. doi: 10.1016/j.ajodo.2006.03.031 [Crossref] [ Google Scholar]
- Klaus K, Eichenauer J, Sprenger R, Ruf S. Oral microbiota carriage in patients with multibracket appliance in relation to the quality of oral hygiene. Head Face Med 2016; 12(1):28. doi: 10.1186/s13005-016-0125-x [Crossref] [ Google Scholar]
- Smiech-Slomkowska G, Jablonska-Zrobek J. The effect of oral health education on dental plaque development and the level of caries-related Streptococcus mutans and Lactobacillus spp. Eur J Orthod 2007; 29(2):157-60. doi: 10.1093/ejo/cjm001 [Crossref] [ Google Scholar]
- Bollen AM, Cunha-Cruz J, Bakko DW, Huang GJ, Hujoel PP. The effects of orthodontic therapy on periodontal health: a systematic review of controlled evidence. J Am Dent Assoc 2008; 139(4):413-22. doi: 10.14219/jada.archive.2008.0184 [Crossref] [ Google Scholar]
- Gontijo L, Cruz Rde A, Brandão PR. Dental enamel around fixed orthodontic appliances after fluoride varnish application. Braz Dent J 2007; 18(1):49-53. [ Google Scholar]
- Krishnan V, Ambili R, Davidovitch Ze, Murphy NC. Gingiva and orthodontic treatment. Semin Orthod 2007; 13(4):257-71. doi: 10.1053/j.sodo.2007.08.007 [Crossref] [ Google Scholar]
- Pinto AS, Alves LS, Zenkner J, Zanatta FB, Maltz M. Gingival enlargement in orthodontic patients: effect of treatment duration. Am J Orthod Dentofacial Orthop 2017; 152(4):477-82. doi: 10.1016/j.ajodo.2016.10.042 [Crossref] [ Google Scholar]
- Tufekci E, Dixon JS, Gunsolley JC, Lindauer SJ. Prevalence of white spot lesions during orthodontic treatment with fixed appliances. Angle Orthod 2011; 81(2):206-10. doi: 10.2319/051710-262.1 [Crossref] [ Google Scholar]
- Alavi S, Yaraghi N. The effect of fluoride varnish and chlorhexidine gel on white spots and gingival and plaque indices in fixed orthodontic patients: a placebo-controlled study. Dent Res J (Isfahan) 2018; 15(4):276-82. [ Google Scholar]
- Landry DF, Shannon IL. A home-care program of chemical preventive dentistry for orthodontic patients. Am J Orthod 1973; 63(1):12-7. doi: 10.1016/0002-9416(73)90106-1 [Crossref] [ Google Scholar]
- Niazi FH, Kamran MA, Naseem M, AlShahrani I, Fraz TR, Hosein M. Anti-plaque efficacy of herbal mouthwashes compared to synthetic mouthwashes in patients undergoing orthodontic treatment: a randomised controlled trial. Oral Health Prev Dent 2018; 16(5):409-16. doi: 10.3290/j.ohpd.a40983 [Crossref] [ Google Scholar]
- Oltramari-Navarro PV, Titarelli JM, Marsicano JA, Henriques JF, Janson G, Lauris JR. Effectiveness of 050% and 075% chlorhexidine dentifrices in orthodontic patients: a double-blind and randomized controlled trial. Am J Orthod Dentofacial Orthop 2009; 136(5):651-6. doi: 10.1016/j.ajodo.2008.01.017 [Crossref] [ Google Scholar]
- Berchier CE, Slot DE, Haps S, Van der Weijden GA. The efficacy of dental floss in addition to a toothbrush on plaque and parameters of gingival inflammation: a systematic review. Int J Dent Hyg 2008; 6(4):265-79. doi: 10.1111/j.1601-5037.2008.00336.x [Crossref] [ Google Scholar]
- Zanatta FB, Moreira CH, Rösing CK. Association between dental floss use and gingival conditions in orthodontic patients. Am J Orthod Dentofacial Orthop 2011; 140(6):812-21. doi: 10.1016/j.ajodo.2011.06.028 [Crossref] [ Google Scholar]
- Naik SP, Punathil S, Shetty P, Jayanti I, Jalaluddin M, Avijeeta A. Effectiveness of different bristle designs of toothbrushes and periodontal status among fixed orthodontic patients: a double-blind crossover design. J Contemp Dent Pract 2018; 19(2):150-5. [ Google Scholar]
- Bock NC, von Bremen J, Kraft M, Ruf S. Plaque control effectiveness and handling of interdental brushes during multibracket treatment--a randomized clinical trial. Eur J Orthod 2010; 32(4):408-13. doi: 10.1093/ejo/cjp088 [Crossref] [ Google Scholar]
- Jordan RA, Hong HM, Lucaciu A, Zimmer S. Efficacy of straight versus angled interdental brushes on interproximal tooth cleaning: a randomized controlled trial. Int J Dent Hyg 2014; 12(2):152-7. doi: 10.1111/idh.12042 [Crossref] [ Google Scholar]
- Quaranta A, Marchisio O, D’Isidoro O, Genovesi AM, Covani U. Single-blind randomized clinical trial on the efficacy of an interdental cleaning device in orthodontic patients. Minerva Stomatol 2018; 67(4):141-7. doi: 10.23736/s0026-4970.18.04104-3 [Crossref] [ Google Scholar]
- Erbe C, Klukowska M, Timm HC, Barker ML, van der Wielen J, Wehrbein H. A randomized controlled trial of a power brush/irrigator/mouthrinse routine on plaque and gingivitis reduction in orthodontic patients. Angle Orthod 2019; 89(3):378-84. doi: 10.2319/022618-159.1 [Crossref] [ Google Scholar]
- Sharma NC, Lyle DM, Qaqish JG, Galustians J, Schuller R. Effect of a dental water jet with orthodontic tip on plaque and bleeding in adolescent patients with fixed orthodontic appliances. Am J Orthod Dentofacial Orthop 2008;133(4):565- 71; quiz 628.e1-2. 10.1016/j.ajodo.2007.12.008.
- Rigau-Gay MM, Claver-Garrido E, Benet M, Lusilla-Palacios P, Ustrell-Torrent JM. Effectiveness of motivational interviewing to improve oral hygiene in orthodontic patients: a randomized controlled trial. J Health Psychol. 2018:1359105318793719. 10.1177/1359105318793719.
- Ross MC, Campbell PM, Tadlock LP, Taylor RW, Buschang PH. Effect of automated messaging on oral hygiene in adolescent orthodontic patients: a randomized controlled trial. Angle Orthod 2019; 89(2):262-7. doi: 10.2319/040618-260.1 [Crossref] [ Google Scholar]
- Kumar GS, Kashyap A, Raghav S, Bhardwaj R, Singh A, Guram G. Role of text message reminder on oral hygiene maintenance of orthodontic patients. J Contemp Dent Pract 2018; 19(1):98-101. [ Google Scholar]
- Moshkelgosha V, Mehrvarz S, Saki M, Golkari A. Computer-based oral hygiene instruction versus verbal method in fixed orthodontic patients. J Dent Biomater 2017; 4(1):353-60. [ Google Scholar]
- Greene JC, Vermillion JR. The oral hygiene index: a method for classifying oral hygiene status. J Am Dent Assoc 1960; 61(2):172-9. doi: 10.14219/jada.archive.1960.0177 [Crossref] [ Google Scholar]
- Löe H, Silness J. Periodontal disease in pregnancy I Prevalence and severity. Acta Odontol Scand 1963; 21:533-51. doi: 10.3109/00016356309011240 [Crossref] [ Google Scholar]
- Cozzani M, Ragazzini G, Delucchi A, Mutinelli S, Barreca C, Rinchuse DJ. Oral hygiene compliance in orthodontic patients: a randomized controlled study on the effects of a post-treatment communication. Prog Orthod 2016; 17(1):41. doi: 10.1186/s40510-016-0154-9 [Crossref] [ Google Scholar]
- Iqbal J, Awan R, Parvez MA, Ul Haq A, Gardezi AA, Irfan S. Effectiveness of text message instructions on oral hygiene for orthodontic patients. Pak Oral Den J 2017; 37(2):278-82. [ Google Scholar]
- Nielsen E, Sheppard MA. Television as a patient education tool: a review of its effectiveness. Patient Educ Couns 1988; 11(1):3-16. doi: 10.1016/0738-3991(88)90072-9 [Crossref] [ Google Scholar]
- Chang HS, Walsh LJ, Freer TJ. Enamel demineralization during orthodontic treatment Aetiology and prevention. Aust Dent J 1997; 42(5):322-7. doi: 10.1111/j.1834-7819.1997.tb00138.x [Crossref] [ Google Scholar]
- Machen DE. Legal aspects of orthodontic practice: risk management concepts Disposing of your orthodontic practice: be careful. Am J Orthod Dentofacial Orthop 1991; 99(5):486-7. doi: 10.1016/s0889-5406(05)81584-7 [Crossref] [ Google Scholar]
- Zachrisson BU. Oral hygiene for orthodontic patients: current concepts and practical advice. Am J Orthod 1974; 66(5):487-97. doi: 10.1016/0002-9416(74)90110-9 [Crossref] [ Google Scholar]
- Glavind L, Zeuner E. Evaluation of a television-tape demonstration for the reinforcement of oral hygiene instruction. J Clin Periodontol 1986; 13(3):201-4. doi: 10.1111/j.1600-051x.1986.tb01460.x [Crossref] [ Google Scholar]
- Boyd RL. Longitudinal evaluation of a system for self-monitoring plaque control effectiveness in orthodontic patients. J Clin Periodontol 1983; 10(4):380-8. doi: 10.1111/j.1600-051x.1983.tb01287.x [Crossref] [ Google Scholar]
- Tan AE, Wade AB. The role of visual feedback by a disclosing agent in plaque control. J Clin Periodontol 1980; 7(2):140-8. doi: 10.1111/j.1600-051x.1980.tb01957.x [Crossref] [ Google Scholar]
- Furusawa M, Takahashi J, Isoyama M, Kitamura Y, Kashima T, Ueshima F. Effectiveness of dental checkups incorporating tooth brushing instruction. Bull Tokyo Dent Coll 2011; 52(3):129-33. [ Google Scholar]
- Davies TM, Shaw WC, Worthington HV, Addy M, Dummer P, Kingdon A. The effect of orthodontic treatment on plaque and gingivitis. Am J Orthod Dentofacial Orthop 1991; 99(2):155-61. doi: 10.1016/0889-5406(91)70118-g [Crossref] [ Google Scholar]
- Kudirkaite I, Lopatiene K, Zubiene J, Saldunaite K. Age and gender influence on oral hygiene among adolescents with fixed orthodontic appliances. Stomatologija 2016; 18(2):61-5. [ Google Scholar]
- Kakudate N, Morita M, Sugai M, Kawanami M. Systematic cognitive behavioral approach for oral hygiene instruction: a short-term study. Patient Educ Couns 2009; 74(2):191-6. doi: 10.1016/j.pec.2008.08.014 [Crossref] [ Google Scholar]