Avicenna J Dent Res. 15(2):53-58.
doi: 10.34172/ajdr.2023.1613
Original Article
The Effect of Laser Diode 940 nm on Decreasing Oropharyngeal Pain After Bimaxillary Orthognathic Surgery: A Double-Blind Randomized Trial Study
Mohammad Reza Jamalpour 1, 2  , Gholam Reza Rouhani 1, *
, Gholam Reza Rouhani 1, * 
Author information:
1Department of Oral and Maxillofacial Surgery, School of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran
2Dental Implants Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
Abstract
Background: Due to its invasiveness and length, bimaxillary orthognathic surgery causes highly excruciating pain in the oropharyngeal area for the patient. There are several ways to reduce this pain, including prescribing painkillers and anti-inflammatory drugs. The aim of this study was to evaluate the effect of photobiomodulation by a 940-nm laser on reducing pain in the oropharyngeal area after bimaxillary orthognathic surgery.
Methods: This randomized clinical trial study was performed on 40 patients aged 17-40 years who were candidates for bimaxillary orthognathic surgery referred to the Department of Oral and Maxillofacial Surgery of Besat hospital in 2021. All patients in the intervention group underwent the photobiomodulation of the oropharyngeal area with a 940-nm diode laser immediately after the end of bimaxillary orthognathic surgery. Sore throat, jaw pain, pain when swallowing, and stridor were recorded in the first to fifth days after surgery. Finally, changes in the mean score of indices were compared within and between the two groups using repeated measure analysis of variance.
Results: The mean age of patients in the intervention and control groups was 22.4±4.38 and 25.15±5.48 years, respectively (P=0.09). The pain score in the four areas studied in both intervention and control groups had a decreasing trend over time, which was statistically significant (P<0.001). In addition, the difference in the trend between the two groups was statistically significant so that in the intervention group, the decreasing trend was more severe (P<0.05). Eventually, a significant interaction was observed between the type of intervention and time in all four areas (P<0.05).
Conclusions: The results showed that the use of a 940-nm diode laser led to a significant reduction in all four areas of sore throat, pain when swallowing, and stridor after bimaxillary orthognathic surgery.
Keywords: Pain, Bimaxillary orthognathic surgery, Photobiomodulation, Clinical trial study
Copyright and License Information
© 2023 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Jamalpour MR, Rouhani GR. The effect of laser diode 940 nm on decreasing oropharyngeal pain after bimaxillary orthognathic surgery: a double-blind randomized trial study. Avicenna J Dent Res. 2023; 15(2):53-58. doi:10.34172/ajdr.2023.1613
Background
Bimax surgery is one of the most important surgeries in the field of maxillofacial surgery, which is performed under general anesthesia. In this process, the patient is intubated, and a pharyngeal pack is placed for the patient (1). There have been many reports on the side effects of using a pharyngeal pack, including sore throat, pharyngeal injury, swelling of the tongue, and painful aphthous ulcers (2,3). Throat ulcers are also common complications after endotracheal intubation (4). In addition, the invasive and lengthy surgical procedure causes severe pain in the oropharyngeal area, which is extremely annoying for the patient (5).
Harmful stimuli following tissue damage due to the osteotomy of the facial bones, periosteum, and muscle stiffness can cause moderate to severe postoperative pain and swelling (6,7). Therefore, the prophylactic administration of sufficient analgesia and management of postoperative pain with analgesia are essential for early recovery and return to normal function (8). Several ways exist for reducing oropharyngeal pain, including analgesics and anti-inflammatory drugs, physiotherapy, ketamine, and magnesium sulfate 15 minutes before induction of anesthesia (9-12). The most commonly prescribed painkillers are nonsteroidal anti-inflammatory drugs (NSAIDs) (13), which unfortunately have many side effects such as gastrointestinal disorders, thrombocytopenia, skin rashes, high blood pressure, and headaches (13).In this regard, a method should be found that prevents long-term complications such as difficulty swallowing, trismus, and stridor in addition to reducing pain. Photodynamic therapy by laser is the method that has been recently considered by researchers in this regard.
Biostimulation using low-power laser radiation is an easy-to-use method for having a direct effect on the tissue and facilitating repair. In recent years, low-level laser therapy (LLLT) has been used to control bone and mucosal lesions. The function of LLLT on bone is through the proliferation and differentiation of osteoblasts, increased calcium deposition, activation of minichromosome maintenance genes, activation of type I collagen formation, increased adenosine triphosphate synthesis, and release of growth factors and cytokines (14). LLLT is also a non-invasive method that has antibacterial and angiogenic effects on soft and hard tissues (15,16). It appears that the energy of the laser activates the lymphatic system and affects the proliferation of macrophages, lymphocytes, endothelial cells, epithelial cells, keratinocytes, and fibroblasts. It further increases the production of mitochondrial enzymes, porphyrins, flavins, and cytochromes (17,18).
Laser plays an important role in maxillofacial surgeries, the benefits of which include homeostasis, reduction of edema, removal of bacteremia, reduction of postoperative pain, infection control, and avoidance of tissue contraction and scarring (12). Laser diode photodynamic therapy reduces inflammatory mediators such as interleukin (IL)-1 beta and IL-17, which improves clinical symptoms (18,19). Photomodulation therapy also reduces the levels of cytokines tumor necrosis factor-alpha and IL-8 (11). LLLT is highly effective in reducing pain and inflammatory responses without any side effects (10). Previous research has shown that one-session LLLT reduces pain and trismus and swelling after impacted dental surgery (20). On the other hand, laser technology has been widely studied in connection with postoperative pain reduction in the field of dentistry, and conflicting results have been obtained in this regard. Therefore, the present study investigated the effect of a 940-nm diode laser on reducing sore throat, pain when swallowing, and stridor after bimaxillary orthognathic surgery.
Materials and Methods
The present randomized controlled trial study was performed on 40 patients aged 17-40 years who were candidates for bimaxillary orthognathic surgery referred to the Department of Oral and Maxillofacial Surgery of Besat hospital affiliated with Hamadan University of Medical Sciences in 2021. Patients were chosen by the convenience sampling method.
Patients with a history of preoperative oral and facial pain, as well as patients receiving preoperative analgesic, sedative, or corticosteroid medications, were excluded from the study. In addition, the patient would be excluded from the study if the surgery lasted more than four or less than three hours, or the intubation procedure was repeated due to failure, or if the surgery became complicated.
Prior to the study, permission was obtained from the Ethics Committee of Hamadan University of Medical Sciences. Further, the signed informed consent form was obtained from each patient before entering the study. To achieve balance in the allocation of patients in the study groups, patients were equally divided into two groups of intervention and control using balanced block randomization. Neither the patients nor the researcher who measured the outcomes after LLLT were aware of the treatment option, and therefore the study was double-blind.
Patients in both groups underwent bimaxillary orthognathic surgery with similar conditions in terms of nasopharyngeal intubation, anesthesia, and pharyngeal pack placement. An oral and maxillofacial surgeon performed operations in the both groups. The anesthesia protocol was hypotensive.Patients in the intervention group underwent the photobiomodulation of the oropharyngeal region with a 940-nm diode laser immediately after the end of bimaxillary orthognathic surgery and before the removal of the nasopharyngeal tube. No radiation was given to the patients in the control group. The laser treatment was performed with a 940-nm diode laser (Biolase, USA). The irradiation parameters used only once were 940 nm in continuous mode with a power density of 0.5 W/cm2, 20 seconds for each region, a spot size of 2.8 cm2, an energy density of 4 J/cm2, and total energy of 50 J (Figure 1).

Figure 1.
Calibrated 940-nm Laser Device.
.
Calibrated 940-nm Laser Device.
The waves were irradiated in continuous mode in all areas of the oropharynx (i.e., the posterior and lateral walls, as well as the posterior tongue) with a normal head without a tip and without contact with the mucosa (Figure 2).
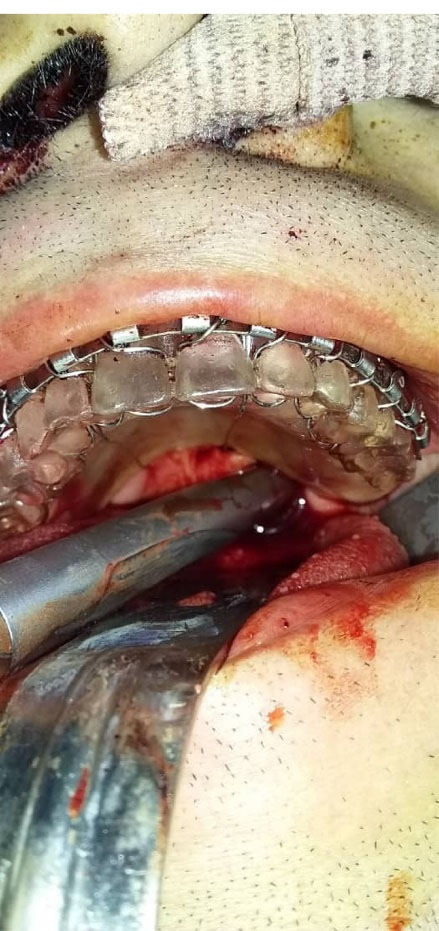
Figure 2.
The Radiation of a 940-nm Wavelength Laser on the Oropharynx.
.
The Radiation of a 940-nm Wavelength Laser on the Oropharynx.
All patients in both groups were asked to record the amount of pain they felt in the throat based on the visual analogue scale (VAS) in the first, second, third, fourth, and fifth days after surgery. In addition, during this time, the patient had to inform about the amount of pain he/she felt in the throat area while swallowing saliva by filling out the intended form. The presence or absence of stridor was also recorded at the same time interval.Prior to surgery, the patient was adequately explained how to determine pain based on the VAS index. The patients were also fully informed about the differentiation of pain in the throat and jaw area before and after the operation. The VAS scale measures a 10-cm line printed on a piece of paper to measure pain. It is “painless” at one end and “worst pain” or “indescribable pain” at the other. The patient puts a cross (×) on the line to indicate the severity of his/her pain. The physician then measures the line with a ruler to get a pain score.
Given that the measurements were performed in 5 consecutive days in each group, the repeated measure analysis of variance test was used to compare the mean scores of sore throat, jaw pain, pain when swallowing, and stridor over time and between the two groups. Finally, SPSS software (version 23) was used for data analysis, and a P value lower than 0.05 was considered statistically significant.
Results
The mean age of patients was 22.4 ± 4.38 and 25.15 ± 5.48 years in the intervention and control groups, respectively (P = 0.09). In terms of gender distribution, 15 (75%) and 13 (65%) patients in the intervention and control groups were males, respectively (P = 0.49).
As shown in Table 1 and Figure 3, the sore throat score in both intervention and control groups has a decreasing trend; more precisely, it decreased from 6.8 ± 2.02 on the first day to 2.75 ± 2.15 on the fifth day after surgery in the intervention group, as well as from 2.8 ± 1.44 on the first day to 1.05 ± 0.02 on the fifth day in the control group. Moreover, the jaw pain score decreased from 6.25 ± 2.45 on the first day to 2.8 ± 1.96 on the fifth day after surgery and from 3.9 ± 1.92 on the first day to 1.8 ± 1.01 on the fifth day in the intervention and control groups, respectively. Regarding the pain score when swallowing, a decline was observed in both intervention and control groups. In other words, it changed from 7.75 ± 2.24 on the first day to 4.4 ± 2.4 on the fifth day from surgery and from 3.75 ± 1.29 on the first day to 1.15 ± 0.37 on the fifth day in the intervention and control groups, respectively. The stridor score also was reduced in both intervention (from 5.75 ± 2.94 on the first day to 3.86 ± 1.86 on the fifth day after surgery) and control (from 1.15 ± 1.95 on the first day to 1 on the fifth day) groups.
Table 1.
Comparison of the Mean Scores of Sore Throat, Jaw Pain, Pain When Swallowing and Stridor in Patients Undergoing Bimaxillary Orthognathic Surgery in the First to Fifth Days After the Intervention in the Two Groups
|
Index
|
Time
|
Intervention Group Mean±SD
|
Control Group Mean±SD
|
Treatment Effect
|
Time Effect
|
Treatment × Time
|
| Sore throat |
Day 1 |
6.8 ± 2.02 |
2.8 ± 1.44 |
F = 46.06
df = 1
P < 0.001 |
F = 77.29
df = 4
P < 0.001 |
F = 11.75
df = 4
P < 0.001 |
| Day 2 |
6.05 ± 2.11 |
2.45 ± 1.46 |
| Day 3 |
5.2 ± 2.24 |
1.5 ± 0.83 |
| Day 4 |
4.05 ± 2.31 |
1.15 ± 0.37 |
| Day 5 |
2.75 ± 2.15 |
1.05 ± 0.22 |
| Jaw pain |
Day 1 |
6.25 ± 2.45 |
3.9 ± 1.92 |
F = 8.51
df = 1
P < 0.001 |
F = 100.55
df = 4
P < 0.001 |
F = 5
df = 4
P < 0.001 |
| Day 2 |
5.35 ± 2.74 |
3.45 ± 1.82 |
| Day 3 |
4.7 ± 2.6 |
2.8 ± 1.7 |
| Day 4 |
3.9 ± 2.17 |
2.1 ± 1.33 |
| Day 5 |
2.8 ± 1.96 |
1.8 ± 1.01 |
| Pain when swallowing |
Day 1 |
7.75 ± 2.24 |
3.75 ± 1.29 |
F = 54.9
df = 1
P < 0.001 |
F = 94.03
df = 4
P < 0.001 |
F = 4.03
df = 4
P = 0.003 |
| Day 2 |
7.25 ± 2.47 |
3.1 ± 1.02 |
| Day 3 |
6.45 ± 2.21 |
2.1 ± 1.02 |
| Day 4 |
5.15 ± 2.48 |
1.5 ± 0.61 |
| Day 5 |
4.1 ± 2.4 |
1.15 ± 0.37 |
| Stridor |
Day 1 |
5.75 ± 2.94 |
1.95 ± 1.15 |
F = 486.72
df = 1
P < 0.001 |
F = 43.63
df = 4
P < 0.001 |
F = 11.6
df = 4
P < 0.001 |
| Day 2 |
5.5 ± 3.14 |
1.65 ± 0.93 |
| Day 3 |
4.6 ± 2.74 |
1.2 ± 0.69 |
| Day 4 |
3.6 ± 2.28 |
1.05 ± 0.22 |
| Day 5 |
3.0 ± 1.86 |
1 |
Note. SD: Standard deviation.
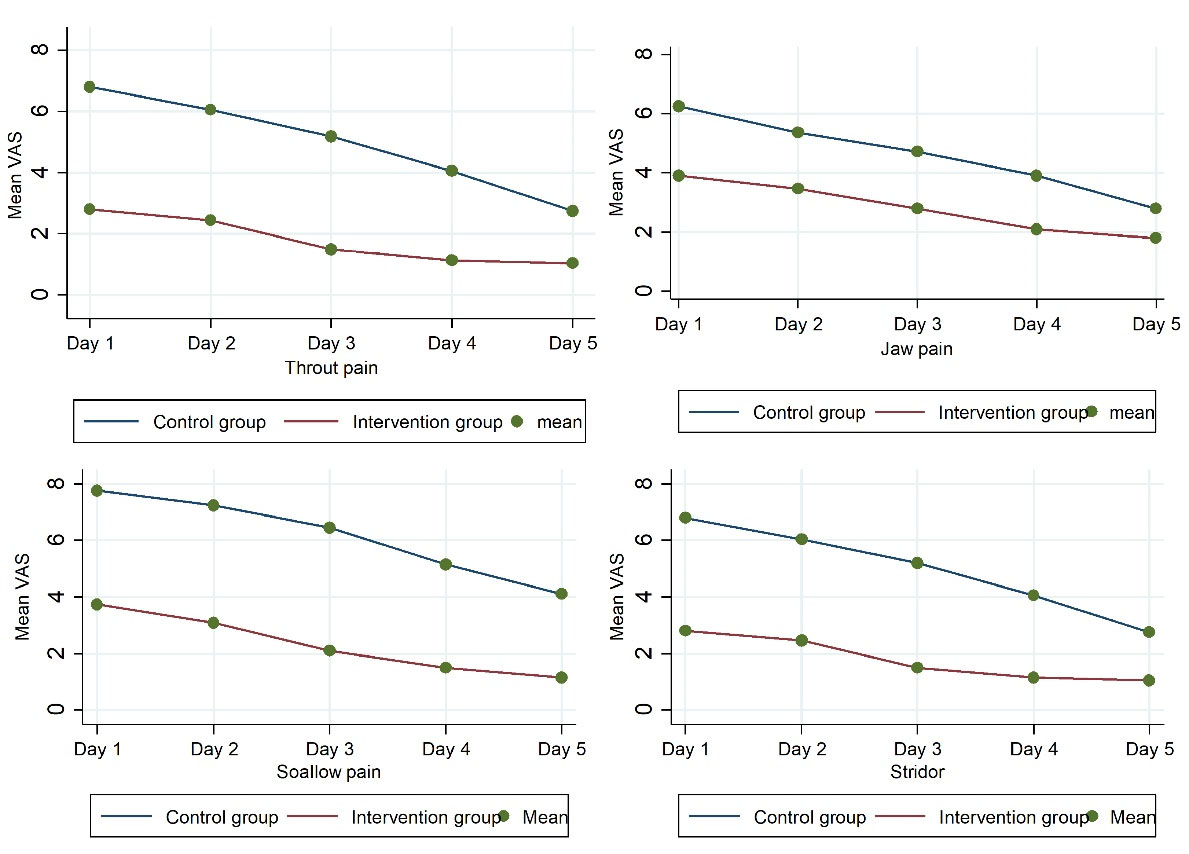
Figure 3.
Trend of Changes in Mean Sore Throat, Jaw Pain, Pain When Swallowing, and Stridor in Patients of the Two Groups.
.
Trend of Changes in Mean Sore Throat, Jaw Pain, Pain When Swallowing, and Stridor in Patients of the Two Groups.
The decreasing trend over time for all four indices was statistically significant (P < 0.001), and the difference in the trend between the two groups was statistically significant so that in the intervention group, the decreasing trend for investigated indices was more severe (P < 0.05). A significant interaction was also observed between the type of intervention and time for all studied indices (P < 0.05).
Discussion
The results of the present study showed that in the LLLT with a wavelength of 940 nm group, the postoperative pain score in the studied areas had a more severe decrease compared to the control group. On the other hand, there was a significant interaction between the treatment group and time and the difference in the pain score between groups, which was extremely high in the first four days but reduced on the fifth day.
As mentioned earlier, the laser used in this study had a wavelength of 940 nm, which has a higher penetration depth than wavelength lasers in the visible spectrum (21-24). Photobiomodulation lasers can affect inflammation in a dose-dependent manner, which ultimately reduces pain. The best results with acute pain occur when high-dose photobiomodulation lasers are used in the first 72 hours after surgery, which can significantly reduce inflammation (25).
Various studies have examined the analgesic effects of laser therapy in the field of dentistry. In line with the results of the present study, those of Matys et al demonstrated that the best effects on relieving orthodontic pain in the maxillary arch were obtained with a diode laser with a wavelength of 635 nm, and the use of ozone therapy represented no significant effects on reducing pain (26). Moreover, Heidari et al reported that a 940-nm laser diode can significantly reduce the pain of periodontal flap surgery (27). In addition, Qamruddin et al found positive results when using the 940-nm laser diode for pain relief during orthodontic treatment. According to their findings, a single dose of LLLT can be effective in reducing pain after the placement of elastomeric separators (24). Likewise, Bayani et al concluded that 810-nm laser wavelength was the most effective orthodontic pain treatment compared to NSAIDs and LLLT with 660-nm wavelength. This finding is important because LLLT can replace NSAIDs at different wavelengths (28). The results of Nóbrega et al revealed that single-dose radiation with LLLT at 830 nm could effectively control the pain caused by the position of interdental elastomeric separators (23). Evidence from the results of a study by Langella et al showed that a single use of postoperative photomodulation therapy reduces inflammation and significantly reduces acute inflammatory pain (29).
However, the effect of laser on reducing postoperative pain has not been significant in some studies in the field of dentistry. For instance, Eroglu and Keskin Tunc (30) indicated that the application of a one-session 940-nm diode laser, immediately after tooth exraction may help patients be less affected by trismus and swelling while not having a significant effect on reducing postoperative pain, which contradicts the results of our study because the use of diode laser reduced pain after surgery in our study.According to the findings of López-Ramírez et al (31), the use of LLLT did not show positive effects on reducing pain, swelling, and trismus after the extraction of the third mandibular incisor. Moreover, Almeida et al (32) used 660- and 780-nm diode lasers immediately after the free gingival transplant surgery and 48 hours later and did not find a clear difference in pain intensity and recovery level between case and control groups. Moslemi et al (33) employed a 660-nm diode laser at the site of the free gingival transplant donor site, but they reported no effect on reducing postoperative pain. Further, Lobo and Pol (34) found no significant difference between the laser (940-nm diode laser) and control groups in chronic periodontal flap surgery.
This contradiction between the findings of the present study and those of the above-mentioned studies can be attributed to the laser settings. These studies mainly aimed to control and promote postoperative recovery, and the pain was a minor parameter. Therefore, the lasers were tuned to accelerate healing as much as possible rather than reducing pain. As mentioned in previous studies, acute pain is better reduced at higher doses in the first 72 hours after surgery, which can reduce inflammation, and then lower doses can be used to accelerate the healing process (25). Additionally, fewer samples were examined in these studies, which could lead to inaccurate results. There are few studies on the use of photobiomodulation lasers in dentistry, and the effect of lasers depends on their settings (e.g., wavelength, power, energy density, radiation duration, distance from the target surface, and radiation mode). Further, the role of different types of surgery (e.g., periodontal plastic surgery, complex surgery, and surgical extraction) can be important in the effectiveness of lasers in reducing pain. The degree of anesthesia can also be an effective factor. In general, there was a difference between our study and previous studies in the use of a 940-nm diode laser in simultaneous orthognathic surgery of two jaws and its different methodology.
The impossibility of 100% simulation of surgical severity and tissue manipulation in all copper patients can be considered one of the limitations of the present study.
Conclusions
Under the limitations of this study, the results demonstrated that the use of a 940-nm diode laser resulted in a significant reduction in all four areas of sore throat, swallowing pain, and stridor.
Acknowledgements
The authors gratefully acknowledge the financial support from the Deputy of Research and Technology of Hamadan University of Medical Sciences.
Authors’ Contribution
Conceptualization: Mohammad Reza Jamalpour, Gholam Reza Rouhani.
Data curation: Mohammad Reza Jamalpour, Gholam Reza Rouhani
Formal analysis: Gholam Reza Rouhani.
Investigation: Mohammad Reza Jamalpour, Gholam Reza Rouhani.
Methodology: Mohammad Reza Jamalpour, Gholam Reza Rouhani.
Project administration: Mohammad Reza Jamalpour, Gholam Reza Rouhani.
Resources: Reza Jamalpour.
Supervision: Reza Jamalpour.
Validation: Reza Jamalpour.
Visualization: Gholam Reza Rouhani.
Writing–original draft: Gholam Reza Rouhani.
Writing–review & editing: Mohammad Reza Jamalpour.
Competing Interests
The authors declare that they have no conflict of interests.
Ethical Approval
This study was approved by the Ethics Committee of Hamadan University of Medical Sciences (IR.UMSHA.REC.1398.096), and registered in the Iranian Registry of Clinical Trials (http://www.irct.ir, identifier: IRCT20120531009926N9).
References
- Kim YK. Complications associated with orthognathic surgery. J Korean Assoc Oral Maxillofac Surg 2017; 43(1):3-15. doi: 10.5125/jkaoms.2017.43.1.3 [Crossref] [ Google Scholar]
- Al-Jandan BA, Syed FA, Zeidan A, Marei HF, Farooq I. Pharyngeal pack placement in minor oral surgery: a prospective, randomized, controlled study. Ear Nose Throat J 2018; 97(3):E18-E21. [ Google Scholar]
- Green R, Konuthula N, Sobrero M, Saini A, Parasher A, Pool C. Use of pharyngeal packs in functional endoscopic sinus surgery: a randomized controlled trial. Laryngoscope 2017; 127(11):2460-5. doi: 10.1002/lary.26651 [Crossref] [ Google Scholar]
- Tay JY, Tan WK, Chen FG, Koh KF, Ho V. Postoperative sore throat after routine oral surgery: influence of the presence of a pharyngeal pack. Br J Oral Maxillofac Surg 2002; 40(1):60-3. doi: 10.1054/bjom.2001.0753 [Crossref] [ Google Scholar]
- Shrestha S, Maharjan B, Karmacharya RM. Incidence and associated risk factors of postoperative sore throat in tertiary care hospital. Kathmandu Univ Med J (KUMJ) 2017; 15(57):10-3. [ Google Scholar]
- de Santana-Santos T, de Souza-Santos JA, Martins-Filho PR, da Silva LC, de Oliveira E Silva ED, Gomes AC. Prediction of postoperative facial swelling, pain and trismus following third molar surgery based on preoperative variables. Med Oral Patol Oral Cir Bucal 2013; 18(1):e65-70. doi: 10.4317/medoral.18039 [Crossref] [ Google Scholar]
- Nagatsuka C, Ichinohe T, Kaneko Y. Preemptive effects of a combination of preoperative diclofenac, butorphanol, and lidocaine on postoperative pain management following orthognathic surgery. Anesth Prog 2000; 47(4):119-24. [ Google Scholar]
- Chegini S, Johnston KD, Kalantzis A, Dhariwal DK. The effect of anesthetic technique on recovery after orthognathic surgery: a retrospective audit. Anesth Prog 2012; 59(2):69-74. doi: 10.2344/11-10.1 [Crossref] [ Google Scholar]
- Kuwamura A, Komasawa N, Takahashi R, Tanaka M, Minami T. Preoperative oral administration of Kikyo-to, a Kampo Medicine, alleviates postoperative sore throat: a prospective, double-blind, randomized study. J Altern Complement Med 2016; 22(4):294-7. doi: 10.1089/acm.2015.0241 [Crossref] [ Google Scholar]
- Rajan S, Malayil GJ, Varghese R, Kumar L. Comparison of usefulness of ketamine and magnesium sulfate nebulizations for attenuating postoperative sore throat, hoarseness of voice, and cough. Anesth Essays Res 2017; 11(2):287-93. doi: 10.4103/0259-1162.181427 [Crossref] [ Google Scholar]
- Teymourian H, Mohajerani SA, Farahbod A. Magnesium and ketamine gargle and postoperative sore throat. Anesth Pain Med 2015; 5(3):e22367. doi: 10.5812/aapm.5(3)2015.22367 [Crossref] [ Google Scholar]
- McHardy FE, Chung F. Postoperative sore throat: cause, prevention and treatment. Anaesthesia 1999; 54(5):444-53. doi: 10.1046/j.1365-2044.1999.00780.x [Crossref] [ Google Scholar]
- Ecklund CR, Ross MC. Over-the-counter medication use in preschool children. J Pediatr Health Care 2001; 15(4):168-72. doi: 10.1067/mph.2001.110913 [Crossref] [ Google Scholar]
- Latifyan S, Genot MT, Klastersky J. Bisphosphonate-related osteonecrosis of the jaw: a review of the potential efficacy of low-level laser therapy. Support Care Cancer 2016; 24(9):3687-93. doi: 10.1007/s00520-016-3139-9 [Crossref] [ Google Scholar]
- Altay MA, Tasar F, Tosun E, Kan B. Low-level laser therapy supported surgical treatment of bisphosphonate related osteonecrosis of jaws: a retrospective analysis of 11 cases. Photomed Laser Surg 2014; 32(8):468-75. doi: 10.1089/pho.2014.3742 [Crossref] [ Google Scholar]
- Garcia VG, da Conceição JM, Fernandes LA, de Almeida JM, Nagata MJ, Bosco AF. Effects of LLLT in combination with bisphosphonate on bone healing in critical size defects: a histological and histometric study in rat calvaria. Lasers Med Sci 2013; 28(2):407-14. doi: 10.1007/s10103-012-1068-5 [Crossref] [ Google Scholar]
- Diniz JS, Nicolau RA, de Melo Ocarino N, do Carmo Magalhães F, de Oliveira Pereira RD, Serakides R. Effect of low-power gallium-aluminum-arsenium laser therapy (830 nm) in combination with bisphosphonate treatment on osteopenic bone structure: an experimental animal study. Lasers Med Sci 2009; 24(3):347-52. doi: 10.1007/s10103-008-0568-9 [Crossref] [ Google Scholar]
- Luomanen M, Alaluusua S. Treatment of bisphosphonate-induced osteonecrosis of the jaws with Nd:YAG laser biostimulation. Lasers Med Sci 2012; 27(1):251-5. doi: 10.1007/s10103-011-0929-7 [Crossref] [ Google Scholar]
- Soheilifar S, Soheilifar S, Hatami S, Vahdatinia F, Molabashi V, Hajiloui M. Effects of low-level diode laser on the level of interleukin 1-beta in the gingival crevicular fluid and the incidence of gingivitis caused by the use of orthodontic separators: a randomized clinical trial. Avicenna J Dent Res 2020; 12(4):120-5. doi: 10.34172/ajdr.2020.24 [Crossref] [ Google Scholar]
- Meco BC, Ozcelik M, Yildirim Guclu C, Beton S, Islamoglu Y, Turgay A. Does type of pharyngeal packing during sinonasal surgery have an effect on PONV and throat pain?. Otolaryngol Head Neck Surg 2016; 154(4):742-7. doi: 10.1177/0194599815626126 [Crossref] [ Google Scholar]
- Aldelaimi AA, Aldelaimi TN, Al-Gburi SM. Using of diode laser (940 nm) in orofacial region. J Res Med Dent Sci 2017; 5(5):34-9. doi: 10.24896/jrmds.2017557 [Crossref] [ Google Scholar]
- Enwemeka CS. Attenuation and penetration of visible 6328 nm and invisible infra-red 904 nm light in soft tissues. Laser Ther 2000; 13(1):95-101. [ Google Scholar]
- Nóbrega C, da Silva EM, de Macedo CR. Low-level laser therapy for treatment of pain associated with orthodontic elastomeric separator placement: a placebo-controlled randomized double-blind clinical trial. Photomed Laser Surg 2013; 31(1):10-6. doi: 10.1089/pho.2012.3338 [Crossref] [ Google Scholar]
- Qamruddin I, Alam MK, Fida M, Khan AG. Effect of a single dose of low-level laser therapy on spontaneous and chewing pain caused by elastomeric separators. Am J Orthod Dentofacial Orthop 2016; 149(1):62-6. doi: 10.1016/j.ajodo.2015.06.024 [Crossref] [ Google Scholar]
- de Paula Eduardo C, de Freitas PM, Esteves-Oliveira M, Aranha AC, Ramalho KM, Simões A. Laser phototherapy in the treatment of periodontal disease A review. Lasers Med Sci 2010; 25(6):781-92. doi: 10.1007/s10103-010-0812-y [Crossref] [ Google Scholar]
- Matys J, Jaszczak E, Flieger R, Kostrzewska-Kaminiarz K, Grzech-Leśniak K, Dominiak M. Effect of ozone and diode laser (635 nm) in reducing orthodontic pain in the maxillary arch-a randomized clinical controlled trial. Lasers Med Sci 2020; 35(2):487-96. doi: 10.1007/s10103-019-02896-0 [Crossref] [ Google Scholar]
- Heidari M, Fekrazad R, Sobouti F, Moharrami M, Azizi S, Nokhbatolfoghahaei H. Evaluating the effect of photobiomodulation with a 940-nm diode laser on post-operative pain in periodontal flap surgery. Lasers Med Sci 2018; 33(8):1639-45. doi: 10.1007/s10103-018-2492-y [Crossref] [ Google Scholar]
- Bayani S, Rostami S, Ahrari F, Saeedipouya I. A randomized clinical trial comparing the efficacy of bite wafer and low level laser therapy in reducing pain following initial arch wire placement. Laser Ther 2016; 25(2):121-9. doi: 10.5978/islsm.16-OR-10 [Crossref] [ Google Scholar]
- Langella LG, Casalechi HL, Tomazoni SS, Johnson DS, Albertini R, Pallotta RC. Photobiomodulation therapy (PBMT) on acute pain and inflammation in patients who underwent total hip arthroplasty-a randomized, triple-blind, placebo-controlled clinical trial. Lasers Med Sci 2018; 33(9):1933-40. doi: 10.1007/s10103-018-2558-x [Crossref] [ Google Scholar]
- Eroglu CN, Keskin Tunc S. Effectiveness of single session of low-level laser therapy with a 940 nm wavelength diode laser on pain, swelling, and trismus after impacted third molar surgery. Photomed Laser Surg 2016; 34(9):406-10. doi: 10.1089/pho.2016.4101 [Crossref] [ Google Scholar]
- López-Ramírez M, Vílchez-Pérez MA, Gargallo-Albiol J, Arnabat-Domínguez J, Gay-Escoda C. Efficacy of low-level laser therapy in the management of pain, facial swelling, and postoperative trismus after a lower third molar extraction A preliminary study. Lasers Med Sci 2012; 27(3):559-66. doi: 10.1007/s10103-011-0936-8 [Crossref] [ Google Scholar]
- Almeida AL, Esper LA, Sbrana MC, Ribeiro IW, Kaizer RO. Utilization of low-intensity laser during healing of free gingival grafts. Photomed Laser Surg 2009; 27(4):561-4. doi: 10.1089/pho.2008.2292 [Crossref] [ Google Scholar]
- Moslemi N, Heidari M, Fekrazad R, Nokhbatolfoghahaie H, Yaghobee S, Shamshiri A. Evaluation of the effect of 660 nm low power laser on pain and healing in palatal donor site: a randomized controlled clinical trial. J Dent Med 2014; 27(1):71-7. [ Google Scholar]
- Lobo TM, Pol DG. Evaluation of the use of a 940 nm diode laser as an adjunct in flap surgery for treatment of chronic periodontitis. J Indian Soc Periodontol 2015; 19(1):43-8. doi: 10.4103/0972-124x.145808 [Crossref] [ Google Scholar]