Avicenna J Dent Res. 15(1):10-17.
doi: 10.34172/ajdr.2023.579
Original Article
Evaluation of Radiographic Features and Clinical Signs of Maxillofacial Malignancies in Patients Referred to Mashhad Dental School During 2003-2017
Samareh Mortazavi 1, 2  , Atessa Pakfetrat 3, Masoome Baghbani 4, Atie Safaee 1, 2, *
, Atessa Pakfetrat 3, Masoome Baghbani 4, Atie Safaee 1, 2, * 
Author information:
1Assistant Professor, Department of Oral and Maxillofacial Radiology, School of Dentistry, Mashhad University of Medical Sciences, Mashhad, Iran
2Assistant Professor, Oral and Maxillofacial Diseases Research Center, Mashhad University of Medical Sciences, Mashhad, Iran
3Professor, Oral and Maxillofacial Diseases Research Center, Mashhad University of Medical Sciences, Mashhad, Iran
4Private Dental Practice, Mashhad, Iran
Abstract
Background: The aim of this study was to evaluate the radiographic and clinical features of malignant oral and maxillofacial lesions in patients referred to the Radiology Department of Mashhad Dental School from 2003 to 2017.
Methods: A total of 45 radiographs of patients who had been referred to the Radiology Department of Mashhad Dental School from 2003 to 2017 were selected from the radiology archive. The patients presenting with malignant lesions in jaws and a definite pathologic diagnosis were selected as the study population. The radiographic features of lesions were investigated using intraoral radiographies, panoramic, and cone-beam computed tomography (CBCT) or computed tomography (CT) views. Then, 18 patients whose information was available were evaluated. Fisher’s exact test was used to compare the characteristics of lesions.
Results: The age of the patients ranged from 5 to 84 years, with a mean of 49.18 years. Of the 45 lesions identified, squamous cell carcinoma (SCC) was the most prevalent malignancy, followed by lymphoma and mucoepidermoid carcinoma. Most malignant lesions were seen in the posterior region of the jaws, and lesions were generally more prevalent in the mandible. Additionally, 77.8% of the observed malignancies had an ill-defined border, and 86.6% of them were radiolucent. In the clinical view, swelling was the most common symptom, and the duration of the disease in the majority of the lesions was less than 3 months.
Conclusions: Paying attention to the course of the lesion, its internal structure and borders in the radiographic view can lead to a more accurate differentiation of malignant lesions from benign ones and timely referral of the patient.
Keywords: Diagnosis, Differential, Mandibular neoplasms, Diagnostic imaging, Maxillary neoplasms, Radiography
Copyright and License Information
© 2023 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Mortazavi S, Pakfetrat A, Baghbani M, Safaee A. Evaluation of radiographic features and clinical signs of maxillofacial malignancies in patients referred to Mashhad Dental School during 2003-2017. Avicenna J Dent Res. 2023; 15(1):10-17. doi:10.34172/ajdr.2023.579
Background
Cancer has been reported to be one of the five major causes of mortality in all societies. In the United States, cancer is the second most common cause of death after cardiovascular diseases. In Iran, cancer is the third leading cause of death, which claims more than 30 000 lives every year. According to published data, 55855 cases of cancer were reported in Iran in 2006. Five percent of all cancers occur in the head and neck region, with almost half of them developing in the oral cavity (1-3).
In addition to proximity to important vital structures, the head and neck area accounts for important physiological processes and plays a significant role in human beauty (4). Depending on a variety of risk factors and environmental conditions, oral cancer can have a broad spectrum of manifestations. For example, in one society with the habit of tobacco consumption (the most important risk factor associated with oral cancer), this disease can be expected to emerge in different forms compared to other communities. Moreover, it has been recorded that oral cancer often affects people over the age of 53. The incidence of oral cancer varies according to age, gender, race, and geographical location. In men, for instance, oral cancer is believed to represent 4% of all cancers their body may develop, while the corresponding figure is 2% for women. The incidence of oral cancer in males ranges from 1 to 10 cases per 100 000 people in different countries (5). In 2010, Taghavi et al conducted a retrospective ten-year study on malignant tumors in Iran. Osteosarcoma proved to be the most common tumor identified in their study, with mucoepidermoid carcinoma and ameloblastic carcinoma occupying the second rank. Men were found to be the most affected gender (6). In 2017, Pałasz et al studied the contemporary methods of diagnostic imaging used to detect oral SCC and stated that it is important to properly combine imaging methods to establish the most effective eclectic protocol (7).
Malignant lesions cause changes in bone tissues that can be detected on panoramic radiographic images and CT scans of the affected area. The authors decided to study the radiographic characteristics as well as clinical signs of malignant lesions in the oral and maxillofacial area in patients referred to the Radiology Department of Mashhad Dental School.
Materials and Methods
In the radiology department of Mashhad Dental School, for each patient who suffers from a lesion in the maxillofacial area, a file containing the patient’s personal information, a brief history, requested and additional radiographic images, and a definitive diagnosis of pathology (if any) is available. To conduct this study, by referring to this archive, all cases that had a malignant lesion with a definite diagnosis in the jaw area were selected. Patients whose information was fully available (presence of radiographic images and definitive pathology results) in the radiology department of Mashhad Dental School during 2003-2017 were included in the study. Patients whose definitive pathology result was not available were excluded from the study. In addition, patients whose radiographic images were not of good quality were excluded from the study. Finally, 45 malignant lesions (31 cases belonged to men [39.7%] and 33 cases belonged to women [20.0%]) were examined for radiographic features in all available radiographic views. After deleting the patients’ names along with the identified types of malignant lesions for the purpose of this study, all of the radiographs were numbered, and subsequently, the radiographic features of these lesions were investigated on all radiographic views (periapical, occlusal, panoramic, cone-beam computed tomography [CBCT], or computed tomography [CT]) by two maxillofacial radiologists according to the checklist for radiographic features of lesions (Figure 1).
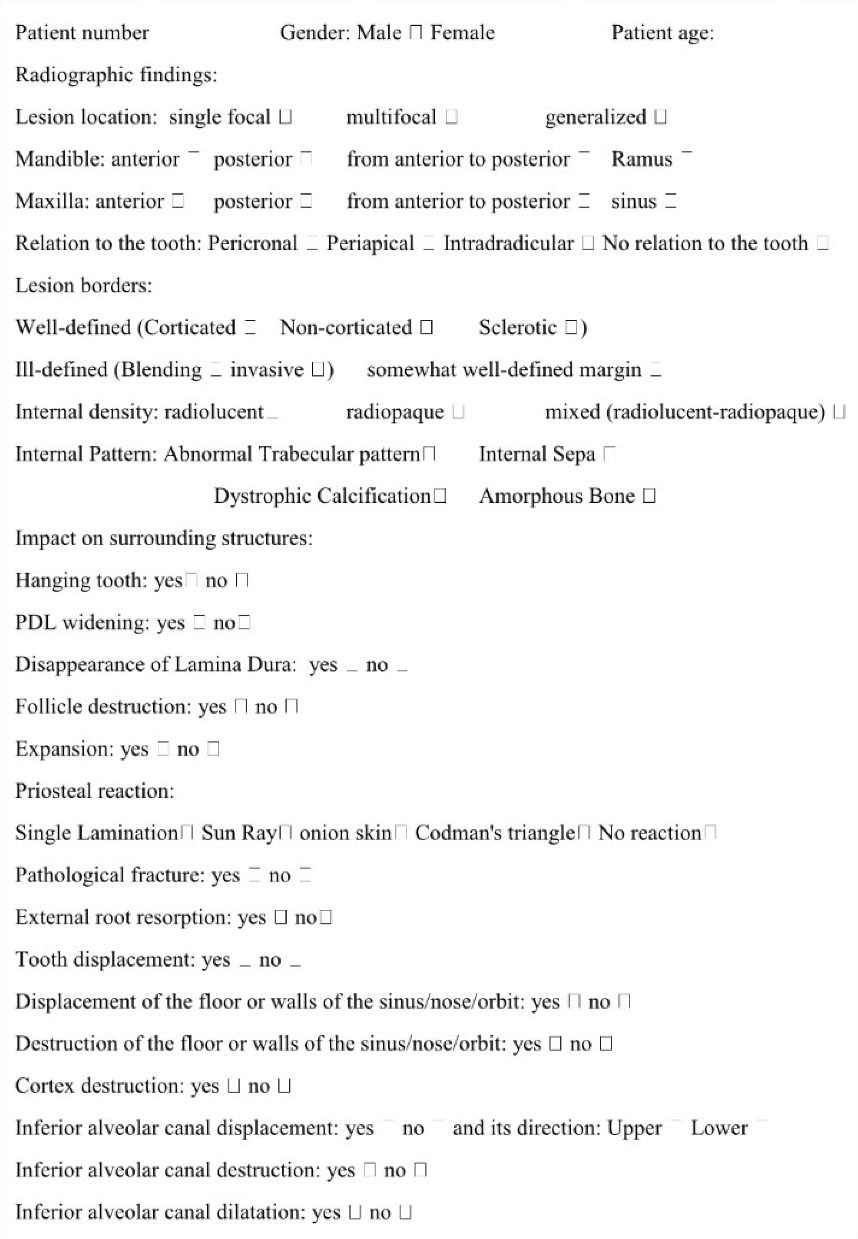
Figure 1.
Checklist for Radiologic Features of Maxillofacial Malignancies
.
Checklist for Radiologic Features of Maxillofacial Malignancies
In the event of any conflict of opinion between the two maxillofacial radiologists, the lesion was observed by a third specialist.
A total of 45 radiographs of patients with malignant maxillofacial lesions were selected from the archives of the radiology department. Then, 18 patients who met the inclusion criteria were selected to evaluate the clinical features of their diseases according to the checklist for clinical features of lesions (Figure 2).
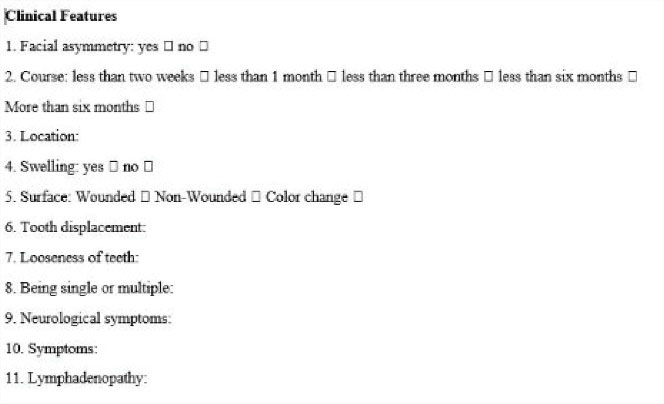
Figure 2.
Checklist for Clinical Features of Maxillofacial Malignancies
.
Checklist for Clinical Features of Maxillofacial Malignancies
Finally, the achieved data were analyzed using the SPSS version 21.0. Fisher’s exact test was used to compare the characteristics of lesions. The statistical significance level was set at P < 0.05.
Results
This study involved 45 radiographs of patients with malignant lesions in the maxillofacial area which were selected from the archives of the radiology department. Due to the fact that the clinical records of all cases were not available in the department of oral diseases, the clinical symptoms of only 18 patients were evaluated.
According to the records found in the radiology department, out of 45 cases, 21 cases were males (46.7%) and 24 cases were females (53.3%). Moreover, the patients aged between 5 and 84 years, with a mean age of 49.18 years. As presented in Table 1, squamous cell carcinoma (SCC) was the most frequently identified lesion detected by biopsy (40% of lesions). Lymphoma and Mucoepidermoid carcinoma, with 5 and 4 cases, respectively, ranked second and third. Among the 45 lesions studied, 21 cases were seen in males and 24 cases in females. The relationship between the type of lesion and gender proved to be statistically significant (P = 0.016).
Table 1.
Distribution of Lesions Detected by Biopsy according to the Gender and Age
|
Type of Lesion
|
Number (%)
|
Mean age
|
Male
|
Female
|
| SCC |
18 (40.0) |
61.4 |
9 (50.0) |
9 (50.0) |
| Lymphoma |
5 (11.1) |
25.8 |
3 (60.0) |
2 (40.0) |
| Mucoepidermoid carcinoma |
4 (8.9) |
45.7 |
0 |
4 (100.0) |
| Chondrosarcoma |
3 (6.7) |
50.6 |
1 (33.3) |
2 (66.7) |
| Osteosarcoma |
2 (4.4) |
35.5 |
1 (50.0) |
1 (50.0) |
| Multiple myeloma |
2 (4.4) |
54.5 |
2 (100.0) |
0 |
| Metastatic tumor |
2 (4.4) |
70 |
0 |
2 (100.0) |
| Adenocarcinoma |
2 (4.4) |
72 |
2 (100.0) |
0 |
| Leukemia |
1 (2.2) |
11 |
0 |
1 (100.0) |
| LCH |
1 (2.2) |
5 |
1 (100.0) |
0 |
| Ewing's sarcoma |
1 (2.2) |
10 |
1 (100.0) |
0 |
| Basal cell carcinoma |
1 (2.2) |
50 |
0 |
1 (100.0) |
| Rhabdomyosarcoma in sinus |
1 (2.2) |
13 |
0 |
1 (100.0) |
| Neurofibrosarcoma |
1 (2.2) |
38 |
1 (100.0) |
0 |
| Pleomorphic adenocarcinoma |
1 (2.2) |
64 |
0 |
1 (100.0) |
| Total |
45 |
49.18 |
21 |
24 |
|
P value (Fisher's exact test) |
|
|
0.016 |
As shown in Table 2, 29 lesions (64.44%) existed in the mandible, of which 24 cases (82.76%) were found to be in the mandible region only and 5 cases (17.24%) involved both jaws. The results revealed that the relationship between the type of lesion and the involved jaw was statistically significant (P = 0.015).
Table 2.
Frequency Distribution of Lesions according to the Location
|
Type of lesion
|
Lesion Location
|
|
|
Mandible
|
Maxilla
|
Both jaws
|
Total (%)
|
| SCC |
12 (66.6%) |
6 (33.3%) |
0 (0.00%) |
18 (40%) |
| Lymphoma |
3 (60%) |
0 (0.00%) |
2 (40%) |
5 (11.11%) |
| Mucoepidermoid carcinoma |
1 (25%) |
3 (75%) |
0 (0.00%) |
4 (8.88%) |
| Chondrosarcoma |
2 (66.6%) |
1 (33.3%) |
0 (0.00%) |
3 (6.66%) |
| Osteosarcoma |
0 (0.00%) |
2 (100%) |
0 (0.00%) |
2 (4.44%) |
| Multiple myeloma |
0 (0.00%) |
0 (0.00%) |
2 (100%) |
2 (4.44%) |
| Metastatic tumor |
2 (100%) |
0 (0.00%) |
0 (0.00%) |
2 (4.44%) |
| Adenocarcinoma |
1 (50%) |
1 (50%) |
0 (0.00%) |
2 (4.44%) |
| Leukemia |
0 (0.00%) |
0 (0.00%) |
1 (100%) |
1 (2.22%) |
| LCH |
1 (100%) |
0 (0.00%) |
0 (0.00%) |
1 (2.22%) |
| Ewing's sarcoma |
1 (100%) |
0 (0.00%) |
0 (0.00%) |
1 (2.22%) |
| Basal cell carcinoma |
0 (0.00%) |
1 (100%) |
0 (0.00%) |
1 (2.22%) |
| Rhabdomyosarcoma in sinus |
0 (0.00%) |
1 (100%) |
0 (0.00%) |
1 (2.22%) |
| Neurofibrosarcoma |
1 (100%) |
0 (0.00%) |
0 (0.00%) |
1 (2.22%) |
| Pleomorphic adenocarcinoma |
0 (0.00%) |
1 (100%) |
0 (0.00%) |
1 (2.22%) |
|
P value (Fisher's exact test) |
0.015 |
45 (100%) |
With regard to mandibular lesions, the highest frequency belonged to the posterior region with 14 cases (48.27%), followed by involvement of both anterior and posterior regions with 9 cases (31%). The lowest frequency was observed in the anterior region and ramus of the mandible, each with 3 cases (10.34%). There were 21 lesions in the maxilla, of which 16 cases were found in the maxilla only and 5 cases involved both jaws. Among these lesions, the highest frequency was observed in the posterior region with 11 cases (52.38%), followed by involvement of both anterior and posterior regions with 4 cases (19.04%). The anterior region and sinus involvements were seen in 3 samples (14.28%) (Figure 3).

Figure 3.
Coronal CBCT Image of a Mucoepidermoid Carcinoma in Maxilla Extending to the Maxillary Sinus
.
Coronal CBCT Image of a Mucoepidermoid Carcinoma in Maxilla Extending to the Maxillary Sinus
Table 3 displays that most of the malignant lesions (60.0%) had an ill-defined invasive border. There was no significant relationship between the type of lesion and the type of borders: ill-defined (invasive, saucer, invasive + saucer, and blending) (P = 0.979) or well-defined (corticated, non-corticated, and sclerotic) (P = 0.695).
Table 3.
Frequency Distribution of Lesions according to the Border
|
Lesion Border
|
Type
|
Number
|
Percent
|
| Ill-defined |
Invasive |
27 |
60.0 |
| Saucer |
4 |
8.9 |
| Invasive + saucer |
4 |
8.9 |
| Blending |
0 |
0.0 |
| Well-defined |
Corticated |
4 |
8.9 |
| Non-corticated |
4 |
8.9 |
| Sclerotic |
1 |
2.2 |
| Poorly-defined |
Poorly-defined |
1 |
2.2 |
As demonstrated in Table 4, there was a significant relationship between the type of lesion and its extension in the jaws (P = 0.005) (Figure 4).
Table 4.
Frequency Distribution of Lesions According to Extension
|
Type of Lesion
|
Lesion Extension
|
|
|
Single Focal
|
Multifocal
|
Generalized
|
Total (%)
|
| Squamous cell carcinoma |
18 (100%) |
0 |
0 |
18 (40) |
| Lymphoma |
3 (60.0) |
1 (20.0) |
1 (20.0) |
5 (11.1) |
| Mucoepidermoid carcinoma |
4 (100%) |
0 |
0 |
4 (8.8) |
| Chondrosarcoma |
3 (100%) |
0 |
0 |
3 (6.6) |
| Osteosarcoma |
2 (100%) |
0 |
0 |
2 (4.4) |
| Multiple myeloma |
0 |
2 (100%) |
0 |
2 (4.4) |
| Metastatic tumor |
2 (100%) |
0 |
0 |
2 (4.4) |
| Adenocarcinoma |
2 (100%) |
0 |
0 |
2 (4.4) |
| Leukemia |
0 |
0 |
1 (100%) |
1 (2.2) |
| Langerhans cell histiocytosis |
0 |
1 (100%) |
0 |
1 (2.2) |
| Ewing's Sarcoma |
1 (100%) |
0 |
0 |
1 (2.2) |
| Basal cell carcinoma |
1 (100%) |
0 |
0 |
1 (2.2) |
| Rhabdomyosarcoma in sinus |
1 (100%) |
0 |
0 |
1 (2.2) |
| Neurofibrosarcoma |
1 (100%) |
0 |
0 |
1 (2.2) |
| Pleomorphic adenocarcinoma |
1 (100%) |
0 |
0 |
1 (2.2) |
| Total |
39 |
4 |
2 |
45 |
|
P value (Fisher's exact test) |
0.005 |
|

Figure 4.
The Panoramic Radiographic View Showing the Multifocal Spread of Multiple Myeloma across the Mandible
.
The Panoramic Radiographic View Showing the Multifocal Spread of Multiple Myeloma across the Mandible
In terms of internal density, 39 lesions (86.6%) were radiolucent, and 6 cases (13.3%) had a mixed characteristic (radiolucent-radiopaque). There was no significant relationship between the type of lesion and its internal density (P = 0.295).
The internal patterns of lesions have been listed in Table 5. There was no significant relationship between the type of lesion and its internal pattern (P = 0.064).
Table 5.
Frequency Distribution of Internal Patterns of Lesions
|
Internal Pattern
|
Number
|
Percent
|
| No internal pattern |
25 |
55.5 |
| Abnormal trabecular appearance |
13 |
28.8 |
| Dystrophic calcification |
3 |
6.6 |
| Internal septa |
1 |
2.2 |
| Amorph bone |
1 |
2.2 |
| Dystrophic calcification + internal septa |
1 |
2.2 |
| Dystrophic calcification + abnormal trabecular appearance |
1 |
2.2 |
| Total |
45 |
100 |
Only 2 cases of SCC had caused inferior alveolar canal displacement (Figure 5). Eleven lesions had resulted in inferior alveolar canal destruction. There was a significant relationship between the type of lesion and inferior alveolar canal destruction (P = 0.029).

Figure 5.
The Cropped Panoramic Image Indicating a Lesion With a Radiolucent Internal Structure and Ill-defined Borders on the Left Side of the Posterior Mandible, Causing Displacement of the Inferior Alveolar Canal in an Inferior Direction
.
The Cropped Panoramic Image Indicating a Lesion With a Radiolucent Internal Structure and Ill-defined Borders on the Left Side of the Posterior Mandible, Causing Displacement of the Inferior Alveolar Canal in an Inferior Direction
Among the study samples, 38 lesions had caused no periosteal reaction. One case of SCC had triggered a single lamination reaction. Sunlight reaction was seen in 3 lesions: 1 case of osteosarcoma, 1 case of lymphoma, and 1 case of Ewing sarcoma. The onion-skin reaction was observed only in 1 case of lymphoma, and the Codman triangle was identified in 2 cases of chondrosarcoma (Figure 6). In general, no significant relationship was found between the various types of periosteal reaction and the type of lesion (P = 0.113).
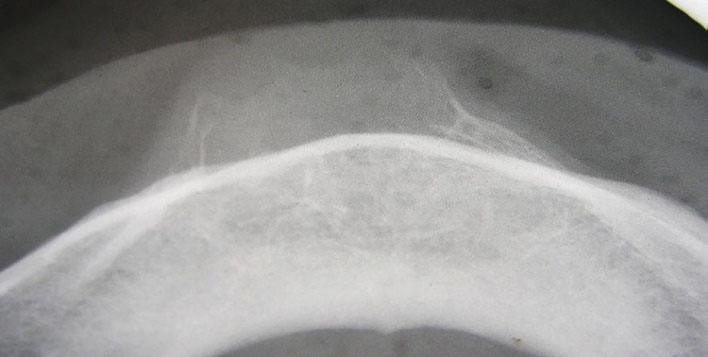
Figure 6.
The Occlusal View Indicating Codman Triangle in Chondrosarcoma
.
The Occlusal View Indicating Codman Triangle in Chondrosarcoma
Tables 6 and 7 provide information on the frequency and relationship of the variables associated with the effect of the lesion on the surrounding structures categorized by the type of lesion (Figures 7 and 8). Among the variables mentioned in the table, there was a significant relationship between the destruction of dental follicles and the type of lesion (P = 0.003).
Table 6.
Effects of Each Lesion on Surrounding Structures
|
Type of Lesion
|
Effects on Surrounding Structures
|
Tooth
Floating
in Air
|
PDL
Widening
|
Lamina
Dura
|
Follicular
Destruction
|
| Squamous cell carcinoma |
6 (33.3%) |
8 (44.4%) |
8 (44.4%) |
0 (0.00%) |
| Lymphoma |
1 (20%) |
3 (60%) |
3 (60%) |
2 (40%) |
| Mucoepidermoid carcinoma |
0 (0.00%) |
1 (25%) |
1(25%) |
0 (0.00%) |
| Chondrosarcoma |
0 (0.00%) |
2 (66.6%) |
2 (66.6%) |
0 (0.00%) |
| Osteosarcoma |
0 (0.00%) |
1 (50%) |
1 (50%) |
1 (50%) |
| Multiple myeloma |
0 (0.00%) |
0 (0.00%) |
0 (0.00%) |
0 (0.00%) |
| Metastatic tumor |
0 (0.00%) |
0 (0.00%) |
0 (0.00%) |
0 (0.00%) |
| Adenocarcinoma |
1 (50%) |
1 (50%) |
1 (50%) |
0 (0.00%) |
| Leukemia |
0 (0.00%) |
1 (100%) |
1 (100%) |
1 (100%) |
| Langerhans cell histiocytosis |
0 (0.00%) |
0 (0.00%) |
0 (0.00%) |
1 (100%) |
| Ewing's Sarcoma |
0 (0.00%) |
1 (100%) |
1 (100%) |
1 (100%) |
| Basal cell carcinoma |
0 (0.00%) |
0 (0.00%) |
0 (0.00%) |
0 (0.00%) |
| Rhabdomyosarcomain sinus |
0 (0.00%) |
0 (0.00%) |
1 (100%) |
1 (100%) |
| Neurofibrosarcoma |
1 (100%) |
1 (100%) |
1 (100%) |
0 (0.00%) |
| Pleomorphic adenocarcinoma |
0 (0.00%) |
0 (0.00%) |
0 (0.00%) |
0 (0.00%) |
| Total |
9 (20%) |
19 (42.22%) |
20 (44.4%) |
7 (15.5%) |
|
P value (Fisher's exact test) |
0.791 |
0.803 |
0.761 |
0.003 |
Table 7.
Effects of Each Lesion on Surrounding Structures
|
Type of Lesion
|
Expansion
|
Root Resorption
|
Tooth Displacement
|
Cortex Destruction
|
| Squamous cell carcinoma |
7 (38.8%) |
2 (11.11%) |
3 (16.6%) |
14 (77.7%) |
| Lymphoma |
3 (60%) |
1 (20%) |
2 (40%) |
3 (60%) |
| Mucoepidermoid carcinoma |
4(100%) |
0 (0.00%) |
0 (0.00%) |
3 (75%) |
| Chondrosarcoma |
1 (33.3%) |
1 (33.3%) |
0 (0.00%) |
3 (100%) |
| Osteosarcoma |
2 (100%) |
0 (0.00%) |
1 (50%) |
2 (100%) |
| Multiple myeloma |
0 (0.00%) |
0 (0.00%) |
0 (0.00%) |
0 (0.00%) |
| Metastatic tumor |
1 (50%) |
0 (0.00%) |
0 (0.00%) |
2 (100%) |
| Adenocarcinoma |
2 (100%) |
0 (0.00%) |
0 (0.00%) |
2 (100%) |
| Leukemia |
0 (0.00%) |
0 (0.00%) |
1 (100%) |
1 (100%) |
| LCH |
1 (100%) |
0 (0.00%) |
0 (0.00%) |
1 (100%) |
| Ewing's Sarcoma |
1 (100%) |
0 (0.00%) |
1 (100%) |
1 (100%) |
| Basal cell carcinoma |
0 (0.00%) |
0 (0.00%) |
0 (0.00%) |
1 (100%) |
| Rhabdomyosarcomain sinus |
1 (100%) |
0 (0.00%) |
1 (100%) |
1 (100%) |
| Neurofibrosarcoma |
1 (100%) |
0 (0.00%) |
0 (0.00%) |
1 (100%) |
| Pleomorphic adenocarcinoma |
1 (100%) |
0 (0.00%) |
0 (0.00%) |
1 (100%) |
| Total |
25 (55.5%) |
4 (8.9%) |
9 (20%) |
36 (80%) |
|
P value (Fisher's exact test) |
0.123 |
0.893 |
0.201 |
0.683 |
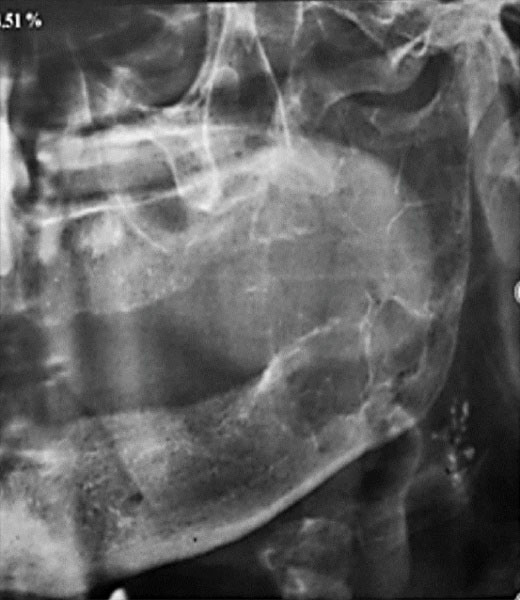
Figure 7.
The Cropped Panoramic Image Indicating Metastatic Tumor of the Thyroid Gland in a 70-year-old Woman With Affected Left Ramus of the Mandible. Several calcified lymph nodes are seen below the angle of the mandible
.
The Cropped Panoramic Image Indicating Metastatic Tumor of the Thyroid Gland in a 70-year-old Woman With Affected Left Ramus of the Mandible. Several calcified lymph nodes are seen below the angle of the mandible

Figure 8.
The Periapical Radiograph Showing Root Resorption of the Premolar Tooth in SCC
.
The Periapical Radiograph Showing Root Resorption of the Premolar Tooth in SCC
Data regarding the clinical symptoms of patients were available for 18 subjects: 8 males and 10 females. In addition, 12 malignant lesions (66.6%) had caused asymmetry in the patients. The duration of the disease was found to be less than 3 months in 8 lesions (44.4%), less than 6 months in 4 lesions (22.2%), less than 1 month in 3 lesions (16.6%), and less than 2 weeks in 3 lesions (16.6%). Fifteen malignant lesions (83.3%) had resulted in swelling. An ulcerated surface was observed in 9 lesions (50.0%), and a non-ulcerated surface in 8 lesions (44.4%). Discoloration was seen in 1 case (5.55%). None of the malignancies had caused tooth displacement. However, tooth loosening had occurred in 6 cases (33.3%). Neurological symptoms were found in cases of pleomorphic adenocarcinoma and non-Hodgkin lymphoma. Six malignant lesions (33.3%) had caused lymphadenopathy.
Discussion
Malignant lesions are associated with a wide range of oral and maxillofacial lesions, among which a number of lesions are more prevalent. Having knowledge of the radiographic features and clinical signs of these lesions will provide invaluable help for clinicians to make faster and more accurate diagnoses as well as to ensure timely initiation of treatment.
In the present study, the radiographic features of 45 oral and maxillofacial lesions along with the clinical signs of 18 cases were available to the researchers. SCC accounted for the highest number of malignant lesions (40%), followed by lymphoma (11.1%) and mucoepidermoid carcinoma (9.9%). The subjects aged between 5 and 82 years, with the mean age being 49.18 years. Women formed a larger proportion of the study population (53.3%). Compared with the study performed by Taghavi et al, the current study featured a broader age range of patients, indicating a higher mean age. Besides, male subjects constituted the greater proportion of the total sample size (6). They described osteosarcoma as the most common malignant lesion of the jaws but did not evaluate soft-tissue malignancies. These facts render the results obtained in their study incomparable with those of the present study (6).
The most common clinical symptoms in the present study were swelling (83.3%) and asymmetry (66.6%). These findings are consistent with the results of the study by Taghavi et al. The most common radiographic feature in their study was reported to be unilocular radiolucency with an ill-defined border, which is consistent with the observations of the current study (6).
In the present study, external root resorption was found in 4 of the 45 malignant lesions: 2 cases of SCC, 1 case of lymphoma, and 1 case of chondrosarcoma. However, in the study by Kawai et al, 72 malignant lesions were evaluated, of which 31 cases had caused external root resorption, including 19 cases of SCC (8). Furthermore, there were comparatively more malignant lesions in the mandible (25 cases). As for the remaining lesions, 16 cases existed in the maxilla, and 4 cases involved both jaws. This distribution of the lesions was similar to what was reported in the study by Taghavi et al (6).
Salivary Gland Malignancies
In the current study, mucoepidermoid carcinoma was observed only in women, which was consistent with the study by Taghavi et al (6). In the present study, there were 7 salivary gland malignancies, including 4 cases of mucoepidermoid carcinoma, 2 cases of adenocarcinoma, and 1 case of pleomorphic adenocarcinoma. From these malignancies, 5 lesions were found in females and 2 cases were found in males, with a mean age of 60.56 years. According to the study conducted by Li et al, the most common salivary gland malignancy was mucoepidermoid carcinoma, and the prevalence of salivary gland malignancies was higher in females than in males, but the mean age of subjects was lower compared to the current study (46.5 years). A greater number of salivary malignancies were observed in the maxilla in the course of the present study, whereas the prevalence of such lesions was higher in the mandible as reported by Yi Li. The majority of the lesions found in the present study were radiolucent and had ill-defined borders. These findings were consistent with those stated in the study conducted by Li et al (9).
Squamous Cell Carcinoma
In the study by Pałasz et al, the prevalence of SCC in males was twice as high as in females, but in the present study, the prevalence of these lesions was equal in males and females (7). Additionally, the onset age of this type of lesion was found to be above 50 years, which is consistent with the data achieved in the present study (5).
Only 1 case of basal cell carcinoma was seen in the current study. This case was identified as a single-focal lesion in the maxilla observed in a 50-year-old female. The border of the lesion was ill-defined and invasive. This lesion did not cause any effect on the teeth or any periosteal reaction. However, cortical destruction was observed.
Sarcomas
In the present study, a case of Ewing’s sarcoma was observed in the posterior lower jaw of a 10-year-old girl. A similarity in terms of the location exists between this case and those reported in the studies by Lopes et al and by Siegal et al (10,11). In terms of the age of the patient, this case was only similar to the one reported by Lopes et al (10). Since the study by Siegal et al investigated Ewing’s sarcoma only in the head and neck area, the most common sites for the occurrence of this lesion were the skull (primary) and the lower jaw (secondary) (11). The current study observed a periosteal reaction in the form of sunray spicules, a finding consistent with the study by Lopes et al (10).
The present study found 3 cases of chondrosarcoma in 2 females and 1 male, with a mean age of 50.6 years. Likewise, Saito et al reported more lesions in females (29 out of the 56 cases of chondrosarcoma examined). With regard to the mean age of patients with chondrosarcoma, however, the figure presented in the current study was 9 years higher than that of the study by Saito et al. In the present study, 2 out of 3 lesions had a mixed internal structure; a higher proportion as compared with the study by Saito et al (12). The current study detected the Codman triangle periosteal reaction in 2 lesions, but according to previous studies, the most prevalent periosteal reaction associated with chondrosarcoma was the sunlight reaction.
In the present study, 2 cases of osteosarcoma were observed in 1 male and 1 female, with a mean age of 35.5 years, and both lesions were observed in the maxilla. The mean age of the patients with such lesions in the study performed by Ajura and Lau was 34 years (13), which is very similar to the figure recorded in the present study. According to the data from the studies by Ajura & Lau (13) and Bianchi & Boccardi (14), most of the osteosarcoma cases were found in the mandible and in males. These findings were not consistent with the results obtained in the present study.
Hematopoietic System Malignancies
The current study found 1 case of Langerhans cell histiocytosis (LCH), with an ill-defined invasive border and a radiolucent internal structure, in a 5-year-old boy. Similar to the present study, the study by Schepman et al also detected a radiolucent internal structure in lesions, but only 3 patients were less than 5 years old. In their study, most of the lesions had well-defined borders, but few cases showed irregular borders (15).
In the present study, two metastatic tumors in the oral and maxillofacial area were examined, both of which were seen in the mandibular region of 2 females with a mean age of 70 years. They were completely radiolucent in terms of internal structure. In a study by Lee and Lee on patients with metastatic tumors, male subjects formed the larger proportion of the cases, and the mean age of the subjects was lower compared to the current study. However, their findings in terms of the common location of the lesion in the mandible as well as the internal structure were consistent with the results of the present study (16).
In the present study, 2 cases of multiple myeloma were observed in males, with a mean age of 54.5 years, both of which showed multifocal extensions in both jaws. These lesions were completely radiolucent and had no corticated border (punched-out). The study by Lambertenghi-Deliliers et al involved 193 patients with multiple myeloma, most of whom were males, with a mean age similar to that in the current study (55 years). Similarly, most lesions were non-corticated and radiolucent (17).
In the present study, 1 case of leukemia was seen in an 11-year-old girl. This case showed generalized involvement of both jaws, which had resulted in the destruction of tooth follicles. Radiographic examination also revealed destruction of lamina dura, periodontal ligament (PDL) widening, and tooth displacement. However, clinical examination only established tooth loosening, but not tooth displacement. These findings were consistent with the results of the study by Curtis (18).
Comparison of the results of the present study with similar studies in the literature revealed some differences in terms of the age range associated with the prevalence of malignant lesions, as well as the gender-based prevalence of lesions. These differences in the findings might be due to the dissimilarities in geographical conditions, lifestyle, or racial characteristics. However, more studies with larger sample sizes can effectively contribute to the verification and generalization of the results achieved in the current study.
Conclusions
Imaging, along with clinical examination, plays an important role in the diagnosis of maxillofacial tumors. The rapid course of the lesion, the radiolucent internal structure, and ill-defined borders in the radiographic view are warning signs that require immediate attention. Advanced imaging techniques such as CT scan or CBCT that allow 3D analysis can be very effective in determining the location of a lesion and revealing the effect of the lesion on the surrounding structures.
Acknowledgments
The authors would like to thank the vice-chancellor for Research at Mashhad University of Medical Sciences, Mashhad, Iran, for the support.
Authors’ Contribution
Conceptualization: Samareh Mortazavi.
Methodology: Samareh Mortazavi, Atessa Pakfetrat, Masoome Baghbani, Atie Safaee.
Validation: Samareh Mortazavi, Masoome Baghbani, Atie Safaee.
Formal Analysis: Samareh Mortazavi, Atessa Pakfetrat, Masoome Baghbani, Atie Safaee.
Investigation:Samareh Mortazavi, Atessa Pakfetrat, Masoome Baghbani, Atie Safaee.
Data Curation: Samareh Mortazavi, Atessa Pakfetrat.
Writing—Original Draft: Samareh Mortazavi, Masoome Baghbani.
Preparation: Samareh Mortazavi, Atie Safaee.
Writing—Review and Editing: Samareh Mortazavi, Atie Safaee
Visualization: Samareh Mortazavi, Atessa Pakfetrat.
Supervision: Atessa Pakfetrat.
Project Administration: Atie Safaee.
Competing Interests
None.
Ethical Approval
Our study was done according to the guidelines of the Declaration of Helsinki and was also approved by the Ethics Committee of Mashhad University of Medical Sciences, Mashhad, Iran (IR.mums.sd.REC.1394.193).
Funding
The vice-chancellor for Research at Mashhad University of Medical Sciences supported the study (No. 950340).
References
- Neville BW, Damm DD, Allen C, Bouquot JE. Oral and Maxillofacial Pathology. 3rd ed. New York: Elsevier; 2009. p. 400-16.
- Aminzadeh A, Motaghi A, Mohammadi E. Epidemiologic study of oral and paraoral malignancies in one cancer referral center in Isfahan during a 5-year period. J Isfahan Dent Sch 2013; 8(6): 560-6. [Persian].
- Mousavi SM, Gouya MM, Ramazani R, Davanlou M, Hajsadeghi N, Seddighi Z. Cancer incidence and mortality in Iran. Ann Oncol 2009; 20(3):556-63. doi: 10.1093/annonc/mdn642 [Crossref] [ Google Scholar]
- Ansari M. A 13 years statistical evaluation on maxillofacial malignant tumors in Hamedan. Journal of Dental Medicine 2003;15(4):103-8. [Persian].
- Petersen PE. The World Oral Health Report 2003: continuous improvement of oral health in the 21st century--the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol 2003; 31 Suppl 1:3-23. doi: 10.1046/j..2003.com122.x [Crossref] [ Google Scholar]
- Taghavi N, Mehrdad L, Rajabi M, Akbarzadeh A. A 10-year retrospective study on malignant jaw tumors in Iran. J Craniofac Surg 2010; 21(6):1816-9. doi: 10.1097/SCS.0b013e3181f43e1f [Crossref] [ Google Scholar]
- Pałasz P, Adamski Ł, Górska-Chrząstek M, Starzyńska A, Studniarek M. Contemporary diagnostic imaging of oral squamous cell carcinoma–a review of literature. Pol J Radiol 2017; 82:193-202. doi: 10.12659/pjr.900892 [Crossref] [ Google Scholar]
- Kawai N, Wakasa T, Asaumi J-i, Kishi K. A radiographic study on resorption of tooth root associated with malignant tumors. Oral Radiol 2000; 16(2):55-65. doi: 10.1007/bf02492700 [Crossref] [ Google Scholar]
- Li Y, Li LJ, Huang J, Han B, Pan J. Central malignant salivary gland tumors of the jaw: retrospective clinical analysis of 22 cases. J Oral Maxillofac Surg 2008; 66(11):2247-53. doi: 10.1016/j.joms.2008.01.041 [Crossref] [ Google Scholar]
- Lopes SL, Almeida SM, Costa AL, Zanardi VA, Cendes F. Imaging findings of Ewing’s sarcoma in the mandible. J Oral Sci 2007; 49(2):167-71. doi: 10.2334/josnusd.49.167 [Crossref] [ Google Scholar]
- Siegal GP, Oliver WR, Reinus WR, Gilula LA, Foulkes MA, Kissane JM. Primary Ewing’s sarcoma involving the bones of the head and neck. Cancer 1987; 60(11):2829-40. doi: 10.1002/1097-0142(19871201)60:11<2829::aidcncr2820601139>3.0.co;2-s [Crossref] [ Google Scholar]
- Saito K, Unni KK, Wollan PC, Lund BA. Chondrosarcoma of the jaw and facial bones. Cancer 1995; 76(9):1550-8. doi: 10.1002/1097-0142(19951101)76:9<1550::aidcncr2820760909>3.0.co;2-s [Crossref] [ Google Scholar]
- Ajura AJ, Lau SH. A retrospective clinicopathological study of 59 osteogenic sarcoma of jaw bone archived in a stomatology unit. Malays J Pathol 2010; 32(1):27-34. [ Google Scholar]
- Bianchi SD, Boccardi A. Radiological aspects of osteosarcoma of the jaws. Dentomaxillofac Radiol 1999; 28(1):42-7. doi: 10.1038/sj.dmfr.4600407 [Crossref] [ Google Scholar]
- Schepman KP, Radden BG, Van der Waal I. Langerhans’ cell histiocytosis of the jaw bones Report of 11 cases. Aust Dent J 1998; 43(4):238-41. doi: 10.1111/j.1834-7819.1998.tb00170.x [Crossref] [ Google Scholar]
- Lee YH, Lee JI. Metastatic carcinoma of the oral region: an analysis of 21 cases. Med Oral Patol Oral Cir Bucal 2017; 22(3):e359-e65. doi: 10.4317/medoral.21566 [Crossref] [ Google Scholar]
- Lambertenghi-Deliliers G, Bruno E, Cortelezzi A, Fumagalli L, Morosini A. Incidence of jaw lesions in 193 patients with multiple myeloma. Oral Surg Oral Med Oral Pathol 1988; 65(5):533-7. doi: 10.1016/0030-4220(88)90135-1 [Crossref] [ Google Scholar]
- Curtis AB. Childhood leukemias: osseous changes in jaws on panoramic dental radiographs. J Am Dent Assoc 1971; 83(4):844-7. doi: 10.14219/jada.archive.1971.0405 [Crossref] [ Google Scholar]