Avicenna J Dent Res. 14(4):165-170.
doi: 10.34172/ajdr.2022.578
Original Article
Influence of Inlays/Onlays and Their Material on Stress Distribution in Mandibular Molars: Finite Element Analysis
Ayham Darwich 1, 2  , Abeer Aljareh 3
, Abeer Aljareh 3  , Omar Aladel 3, Szabolcs Szávai 4
, Omar Aladel 3, Szabolcs Szávai 4  , Hasan Nazha 4, *
, Hasan Nazha 4, * 
Author information:
1Faculty of Biomedical Engineering, Al-Andalus University for Medical Sciences, Tartous, Syria
2Faculty of Technical Engineering, University of Tartous, Tartous, Syria
3Faculty of Dentistry, Damascus University, Damascus, Syria
4Faculty of Mechanical Engineering and Informatics, University of Miskolc, Miskolc, Hungary
Abstract
Background: This study aimed to evaluate the influence of inlays/onlays and their material on stress distribution in mandibular molars with large cavities, using finite element analysis (FEA).
Methods: 3D models of the first mandibular molar were created. Then, a mesio-occluso-distal cavity was created, and cusps were reduced (1.5 mm for buccal cusps and 1 mm for lingual cusps). The restorations were: inlay, onlay that covered buccal cusps (B models), and onlay that covered all cusps (LB models). Inlays and onlays were represented by two materials: nanofill composite resin and polymer-infiltrated ceramic network (PICN). Vertical load of 600 N was applied and von Mises stresses were calculated.
Results: Inlay models showed higher stress concentration in tooth structures than onlay models. Composite resin inlays and onlays transmitted most of the stress to adjacent structures. On the other hand, PICN inlays/onlays absorbed most of stress and transmitted less stress to dental structures than composite resin restorations. Moreover, stress concentrations in PICN onlay models (B-buccal cusps and LB-all cusps) were similar, while composite resin LB onlay showed higher stress concentration in dental structures than composite resin B onlay.
Conclusions: Onlays showed better stress distribution than inlays. PICN might be a suitable choice as a restorative material of inlay/onlay for large cavities in molars, while the composite resin is unfavorable material for such restorations in terms of stress redistribution in dental structures.
Keywords: Ceramics, Composite resins, Inlays, Onlays, Finite element analysis
Copyright and License Information
© 2022 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Darwich A, Aljareh A, Aladel O, Szávai S, Nazha H. Influence of Inlays/Onlays and their material on stress distribution in mandibular molars: finite element analysis. Avicenna J Dent Res. 2022; 14(4):165-170. doi:10.34172/ajdr.2022.578
Introduction
Posterior teeth show hard tissue loss due to caries, trauma, abrasion, and other factors (1,2). Restorative materials must be biocompatible and able to withstand different conditions in the oral environment (1). The inlay is an intracoronal restoration that does not cover any cusp, whereas the onlay is a partial-coverage restoration that covers at least one cusp (3). Inlays and onlays provide conservative restorations for posterior teeth since preparation for inlay/onlay involves removing about 27%-39% of intact tissues, respectively, while preparation for a full crown requires removing 67.5%-75.6% of intact tissues (4). Furthermore, the mean survival rate of inlays is 90.89%, while it is 93.50% for onlays (5).
Inlays and onlays can be made of several materials such as composite resin and ceramic (6). Composite resin restorations could be fabricated directly in the mouth or indirectly. Direct restorations have some drawbacks such as poor contact points and polymerization shrinkage, while indirect way provides better mechanical and anatomical properties (2). Indirect composite resin systems contain a high amount of glass fillers. Indirect composite resins provide high mechanical and aesthetic properties, good marginal integrity, and low polymerization shrinkage (7). Composite resin can be classified into megafill, macrofill, midifill, minifill, microfill, hybrid, and nanofill composite resins according to the size and amount of filler particles. Nanofill composite resin contains silica or silica and zirconia as filler particles with a size of 20 nm (7). Having nanofillers in its composition, nanocomposite resin shows high mechanical resistance, high optic properties, low water absorption, and good surface quality. Therefore, it could be used for both anterior and posterior restorations (7). FiltekTM Supreme (3M ESPE, USA) is an example of nanofill composite resin which could be used for direct restorations as well as indirect restorations including inlays and onlays (8).
Ceramic restorations have improved aesthetic appearance and physical properties; however, they have much higher elastic moduli than dentin (9,10). Trying to produce materials whose elastic moduli are closer to the elastic modulus of dentin and materials that can be milled and fabricated easily, especially by computer aided design/computer aided manufacturing (CAD/CAM) technique, resin-matrix ceramic materials have been introduced (11). Various types and amounts of resin matrices and ceramic fillers are used in resin-matrix ceramics (12). Polymer-infiltrated ceramic network (PICN), which is described as hybrid ceramic, consists of a sintered feldspathic ceramic network (86% by weight) and a polymer network (14% by weight) (11). The ceramic network is pretreated with a coupling agent. Then, it is infiltrated with monomers which polymerize later and organize within the ceramic network. Consequently, the two networks combine together within the material (13).
The results of previous studies about inlays and onlays are still conflicting. Some authors concluded that cusp coverage was necessary to protect dental structures and improve the pattern of stress distribution (10,14), while others found that fracture resistance of inlays (2646.7N) was higher than fracture resistance of onlays (1673.6N) (15). Furthermore, composite resin restorations were found to be associated with good patterns of stress distribution in dental structures (2,6). However, other studies concluded that PICN restorations were better than feldspathic ceramic and composite resin in terms of stress distribution and fracture strength (16,17). The present study was conducted to evaluate the influence of inlays and onlays and their materials on stress distribution in mandibular molars when a vertical load was applied, using finite element analysis (FEA).
Materials and Methods
Modelling and Preparation
This study was performed using 3D FEA. A left first mandibular molar was scanned by cone-beam computed tomographic imaging (CBCT). Then, the scans were imported to Materialise Mimics software version 21.0 (Leuven, Belgium) to isolate tooth structures. Materialise 3-Matic software (Leuven, Belgium) was also used and 3D models were exported as STL files. Using a reverse engineering program (Geomagic Studio 2012, Geomagic Inc, USA), the models were refined and saved as IGES files. Afterwards, they were converted into solid bodies by PowerShape Ultimate 2017 (Autodesk Inc, USA) which was also used to perform Boolean operations. Then, SolidWorks 2018 (Dassault Systèmes SolidWorks Corporation, USA) was used to create 3D models of spongy bone, cortical bone, and tooth structures. A mesio-occluso-distal (MOD) cavity was created for an inlay preparation. The occlusal cavity was larger than two-thirds of the intercuspal distance in width and 2.0 mm in depth. The inlay preparation was modified by reducing the cusps to represent preparations for buccal-cusp-coverage onlay (B onlay model) and all-cusp-coverage onlay (LB onlay model). Buccal cusps were reduced by 1.5 mm and lingual cusps were reduced by 1.0 mm.
The studied restorations included inlay, B onlay (covered buccal cusps), and LB onlay (covered all cusps) (Figure 1).
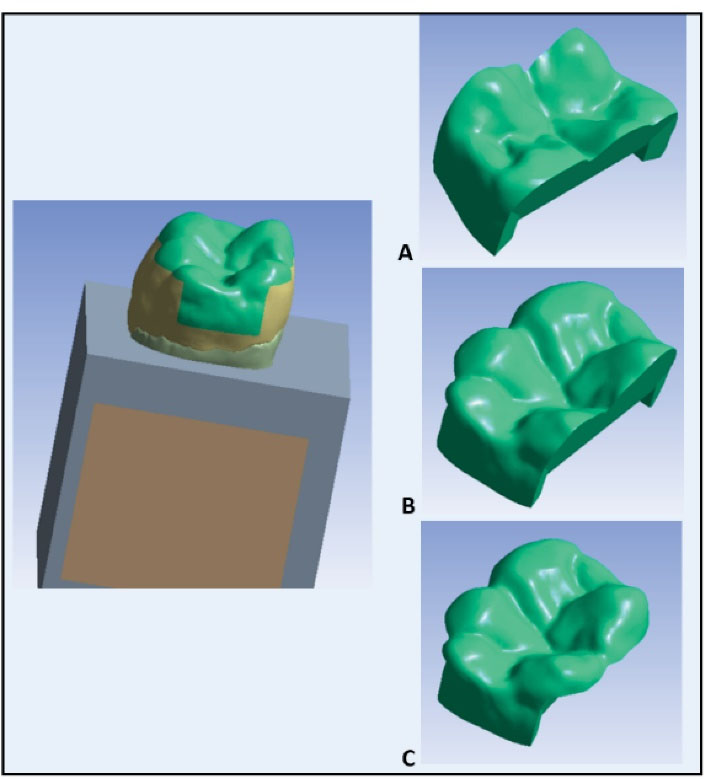
Figure 1.
The Studied Model. A: Inlay, B: Onlay covering buccal cusps, and C: Onlay covering all cusps.
.
The Studied Model. A: Inlay, B: Onlay covering buccal cusps, and C: Onlay covering all cusps.
Finally, all objects were imported into ANSYS Workbench version 20.0 R2 (Ansys Inc; Canonsburg, Pennsylvania, USA) as parasolid (x.t) files to perform FEA. Two restorative materials were represented for each restoration: (C) composite resin and (P) PICN. A mesh of linear tetrahedral quadratic elements connected in nodes was generated for each model. The total number of elements and nodes in the models is summarized in Table 1.
Table 1.
Number of Elements and Nodes of the Models
|
Model
|
Elements
|
Nodes
|
| Inlay |
37937 |
72030 |
| B onlay* |
61531 |
131946 |
| LB onlay** |
84525 |
153238 |
* B onlay: covered buccal cusps; **LB onlay: covered all cusps.
Material Properties and Meshing
All materials were assumed to be isotropic, homogeneous, and linear elastic. The mechanical properties of all materials used in this study are taken from the literature. A summary of the mechanical properties is shown in Table 2.
Table 2.
The Mechanical Properties of Studied Materials
|
Material
|
Young’s modulus (GPa)
|
Poisson’s Ratio
|
Reference
|
| Enamel |
84 |
0.33 |
(18) |
| Dentin |
18.6 |
0.30 |
(18) |
| Pulp |
0.002 |
0.45 |
(19) |
| Cortical bone |
13.7 |
0.30 |
(18) |
| Spongy bone |
1.37 |
0.30 |
(18) |
| PICN |
30 |
0.23 |
(20,21) |
| Composite resin |
12.7 |
0.35 |
(18) |
Boundary Conditions
The models were fixed at the inferior surface of the cortical bone. A vertical load of 600 N was applied to buccal cusp tips, central fossa, and distal marginal ridge. Then, stresses were analyzed according to von Mises stress in all models.
Results
The data obtained from the FEA were presented in maps with a color scale ranging from the highest values (purple and red colors) to the lowest values (blue color) in all models. Stress distribution patterns in the models are shown in Figures 2 to 5. The von Mises theory was used to determine the stress distribution in enamel, dentin, and restoration. The maximum stress values evaluated in megapascals (MPa) are summarized in Table 3.
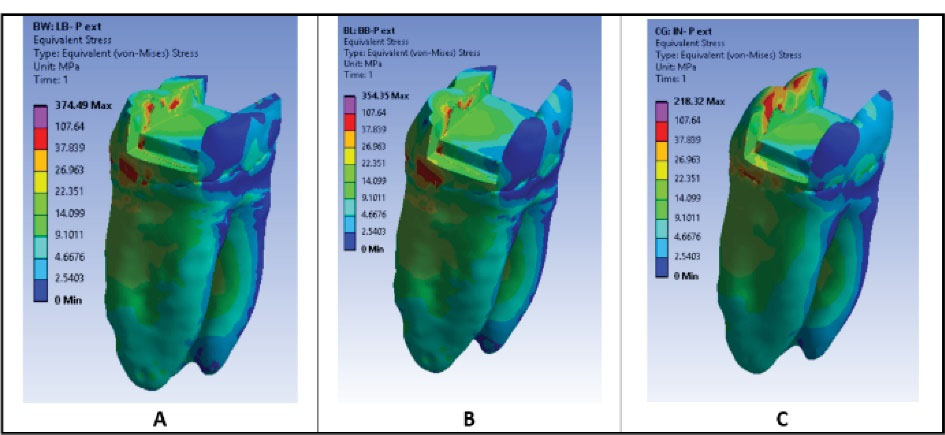
Figure 2.
Stress Distribution in Dental Structures in PICN Models: (A) LB onlay model (all cusp coverage), (B) B onlay model (buccal cusp coverage), (C) Inlay model.
.
Stress Distribution in Dental Structures in PICN Models: (A) LB onlay model (all cusp coverage), (B) B onlay model (buccal cusp coverage), (C) Inlay model.
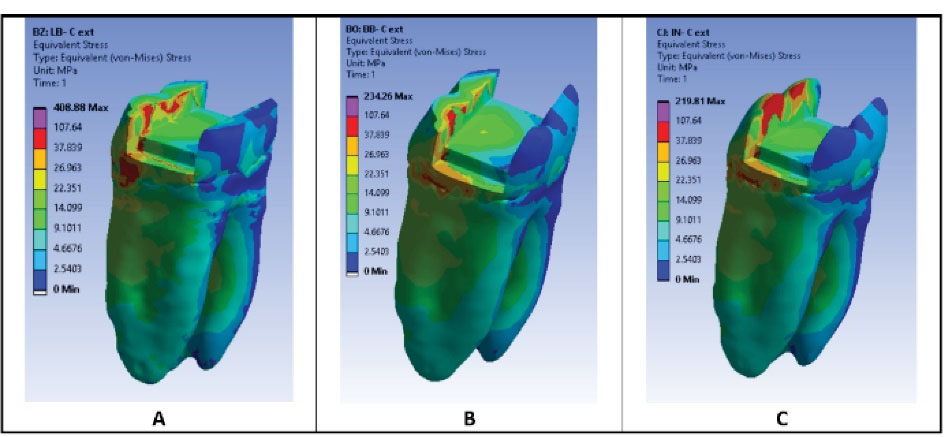
Figure 3.
Stress Distribution in Dental Structures in Composite Resin Models: (A) LB onlay model (all cusp coverage), (B) B onlay model (buccal cusp coverage), (C) Inlay model.
.
Stress Distribution in Dental Structures in Composite Resin Models: (A) LB onlay model (all cusp coverage), (B) B onlay model (buccal cusp coverage), (C) Inlay model.
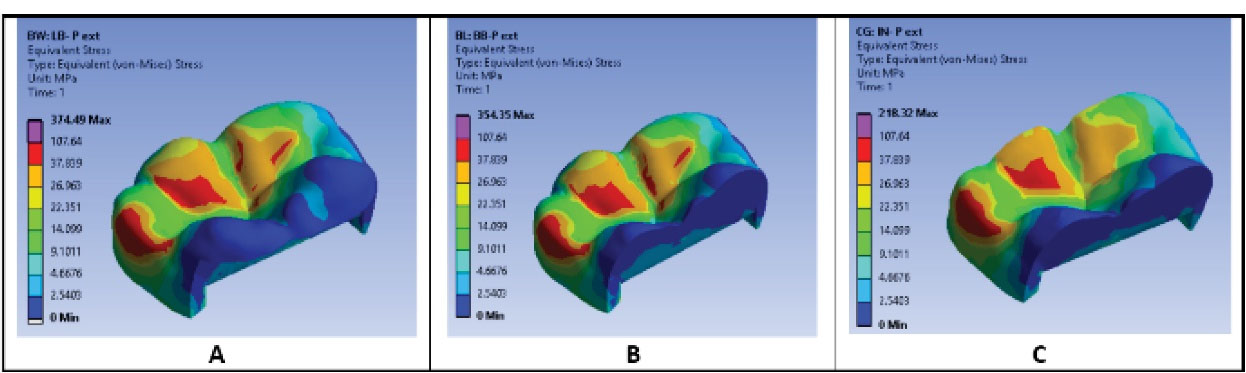
Figure 4.
Stress Distribution in PICN Restorations: (A) LB onlay model (all cusp coverage), (B) B onlay model (buccal cusp coverage), (C) Inlay model.
.
Stress Distribution in PICN Restorations: (A) LB onlay model (all cusp coverage), (B) B onlay model (buccal cusp coverage), (C) Inlay model.
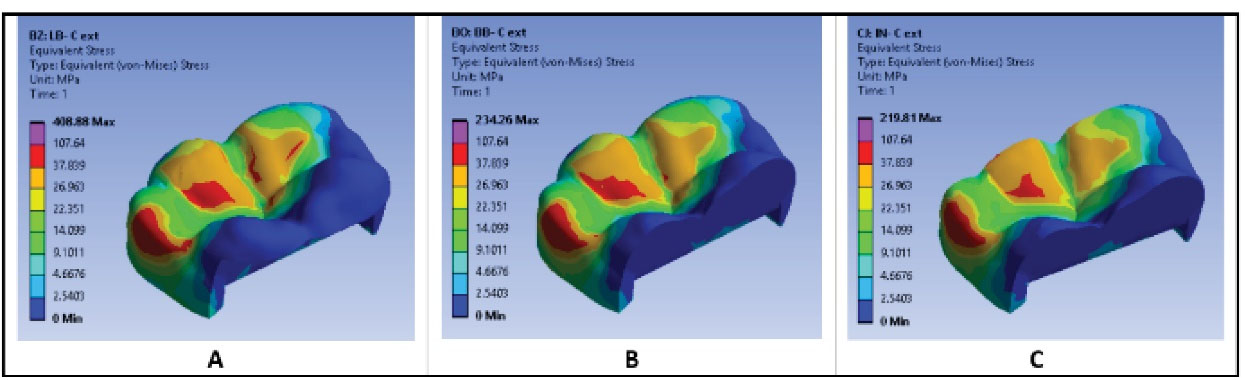
Figure 5.
Stress Distribution in Composite Resin Restorations: A. LB onlay model (all cusp coverage), B. B onlay model (buccal cusp coverage), C. Inlay model.
.
Stress Distribution in Composite Resin Restorations: A. LB onlay model (all cusp coverage), B. B onlay model (buccal cusp coverage), C. Inlay model.
Table 3.
The Values of von Mises Stresses (MPa) in Dental Structures and Restorations in All Models
|
Model
|
Enamel
|
Dentin
|
Restoration
|
| Inlay/PICN (P) |
212.74 |
45.387 |
60.501 |
| Inlay/Composite resin (C) |
209.54 |
42.896 |
59.412 |
| B*1-Onlay/P* |
354.35 |
137.72 |
71.376 |
| B*1-Onlay/C** |
234.26 |
42.343 |
88.801 |
| LB*2-Onlay/P* |
374.49 |
205.44 |
79.515 |
| LB*2-Onlay/C** |
408.88 |
257.33 |
90.148 |
*1 B: onlay that covered buccal cusps; *2LB: onlay that covered all cusps. *P: PICN (polymer infiltrated network ceramic); ** C: composite resin.
Stress Distribution in Tooth Structures
Color maps showed that stress was concentrated in the cervical area of the tooth in all models (Figures 2 and 3). It was also concentrated in the buccal cusps and the internal buccal wall of the occlusal cavity in inlay models (Figures 2C and 3C).
Stress concentration in the composite resin inlay model was higher compared to PICN inlay model (Figures 2C and 3C). Inlay models had more stress concentration in enamel and dentin than B and LB onlay models (Figures 2 and 3).
In onlay models (B and LB), stresses were concentrated in the internal buccal wall of the occlusal cavity as well as the cervical area of the tooth, particularly the distal cervical region. Stress in dental structures in B onlay model was similar to stress in LB onlay model when the material was PICN (Figures 2A and 2B), while stresses in dental structures in composite resin LB onlay model were higher compared to composite resin B onlay model (Figures 3A and 3B). However, composite resin models showed greater stress concentration in enamel than in PICN models irrespective of the design of the restoration (inlay, B onlay, or LB onlay) (Figures 2 and 3).
The values of von Mises stress in dental structures are shown in Table 3. Composite resin LB onlay model showed the highest values of stress in enamel and dentin among all models.
Stress Distribution in Restorations
Stress was concentrated in the internal slope of the middle buccal cusp and the distal marginal ridge in inlays and onlays. Stress lay on larger space in onlays than in inlays (Figures 4 and 5). It was also concentrated in the mesio-buccal cusp of PICN onlays (B and LB) and composite resin LB onlay (Figures 4A, 4B, and 5A). Stresses in restoration in both B and LB PICN onlay models were similar (Figures 4A and 4B), whereas the composite resin LB onlay model showed greater stress in the restoration than B onlay model (Figures 5A and 5B). All PICN models showed higher stress concentration in the restoration than composite resin models (Figures 4 and 5). The values of von Mises stresses in all restorations are shown in Table 3. Composite resin LB onlay showed the greatest value of stress in the restoration.
Discussion
FEA is considered an effective tool to analyze stresses in complex structures and evaluate their behavior under diverse conditions. Using FEA helps to predict the clinical performance of the restorative materials and the dental tissues in tooth-restoration complex (22). The current study aimed to evaluate stress distribution in mandibular molars with large cavities restored by inlays and onlays from different materials. Therefore, MOD cavities were created as mentioned in the literature (23). An average load of 600 N was applied to occlusal contact points (2,18). Then, stress was analyzed using equivalent von Mises stress, which is considered an indicator of the potential failure in the studied structures as it calculates all principal stresses (tensile, shear, and compressive stresses) in the study field (22).
Color maps showed that stress was concentrated in the loading points which are the occlusal contact points on enamel or onlay. It was also seen in the cervical area of the tooth. This result is consistent with the results of previous studies (2,10,24). Furthermore, stress was concentrated highly in the buccal cusps and the internal buccal wall of the occlusal cavity in inlay models. The finding is consistent with the findings of previous studies (10,18). This pattern of stress concentration might indicate clinical failure of dental structures or chipping of the buccal occlusal margins of inlay (10). Wear of composite resin inlay is higher and faster than the wear of the adjacent enamel. As a result, forces would act mainly on the dental structures which remain in more height than the inlay, and that may lead to tooth fracture (10,25). On the contrary, the wear rate of PICN is low, which is similar to that of lithium disilicate ceramic (20). Consequently, stresses in the buccal wall, which might be in the tooth-inlay interface, may lead to fracture or chipping of PICN inlay rather than fracture of the tooth (10,25).
Onlay models showed less stress concentration in dental tissues than in inlay models. It could be explained by cusp coverage. Forces were applied mainly on B and LB onlay models which absorbed most of the stress, while forces acted mainly on the buccal cusps of enamel with some forces applied on inlay. Therefore, more stresses were concentrated in dental structures in inlay models. These findings are in agreement with many studies which found that cusp coverage is an important factor in protecting the remaining tooth structures (10,14,18).
The pattern of stress distribution in dental structures in PICN B onlay model was similar to the pattern in PICN LB onlay model, whereas composite resin LB onlay model showed higher stress concentration in dental structures than B onlay model. This result could be attributed to the elastic modulus of the restorative material and its volume (10,26). Due to the low elastic modulus of composite resin, it transmits a lot of stress to tooth structures. Moreover, when more cusps are covered by composite resin onlay, the onlay volume increases and stress transmission to tooth structures increases as well. On the contrary, the elastic modulus of PICN is high and closer to the elastic modulus of dentin compared to composite resin. Furthermore, the more cusps are covered with PICN onlay, the more tooth structure protection could be provided by PICN restoration. This finding is in line with that of a study by Chang et al (27) who found that covering buccal and palatal cusps with ceramic onlays reduced stress concentration in dental structures although their study was carried out on upper premolars.
According to the restorative material and regardless of the restoration design, color maps showed that composite resin models had less stress concentration in the restoration and much more stress concentration in dental structures than PICN models. The results can be explained by the elastic moduli of the studied restorative materials. The higher the elastic modulus of the material, the higher the stress concentrates in the restorations (10). The elastic modulus of PICN is nearly three times as high as the elastic modulus of composite resin. Therefore, composite resin inlays and onlays cause great stress concentration in the surrounding dental tissues, while PICN restorations absorb stresses and minimize stress transmission to tooth structures (10).
Although FEA helps to predict clinical failure, it is hard to create all clinical situations precisely. For instance, all materials were assumed to be linear elastic and homogeneous even though their properties may be different in reality. Moreover, luting cement thickness was not represented since many previous studies accepted it as a part of dental tissues (6,22). It is also difficult to represent a non-uniform thickness of cement layer the same as its real thickness around restoration (2).
Conclusions
Within the limitations of this study, the following conclusions were drawn:
-
Onlays showed a better pattern of stress distribution in dental structures than inlays.
-
PICN inlays/onlays showed good behavior in terms of stress distribution. This behavior may make PICN a good choice as a restorative material for large cavities in molars, particularly when coverage of all cusps is required.
-
Composite resin inlays/onlays did not show a good pattern of stress redistribution in dental structures. Therefore, composite resin might be unsuitable material for the restoration of large cavities in molars.
Acknowledgments
The authors are grateful to the University of Miskolc (Institute of Machine and Product Design) for its unlimited support.
Author Contributions
Conceptualization: Ayham Darwich, Abeer Aljareh, Omar Aladel.
Data curation: Ayham Darwich, Abeer Aljareh.
Formal Analysis: Ayham Darwich, Abeer Aljareh.
Investigation: Ayham Darwich, Abeer Aljareh, Omar Aladel.
Methodology: Ayham Darwich, Abeer Aljareh, Omar Aladel.
Resources: Ayham Darwich, Abeer Aljareh, Szabolcs Szávai, Hasan Nazha.
Software: Ayham Darwich, Abeer Aljareh, Szabolcs Szávai, Hasan Nazha.
Supervision: Ayham Darwich, Omar Aladel.
Validation: Szabolcs Szávai, Hasan Nazha.
Visualization: Szabolcs Szávai, Hasan Nazha.
Writing – original draft: Ayham Darwich, Abeer Aljareh.
Writing – review & editing: Abeer Aljareh, Szabolcs Szávai, Hasan Nazha.
Conflict of Interest Disclosures
All authors were fully involved in the study and preparation of the manuscript and declared that they had no conflict of interest.
Ethical Statement
This study was approved by the Ethics Committee of Damascus University (No. 3101 dated 6/8/2018).
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- Oen KT, Veitz‐Keenan A, Spivakovsky S. CAD/CAM versus traditional indirect methods in the fabrication of inlays, onlays, and crowns The Cochrane Library 2014;4:1-8 Oen KT, Veitz-Keenan A, Spivakovsky S, Wong YJ, Bakarman E, Yip J CAD/CAM versus traditional indirect methods in the fabrication of inlays, onlays, and crowns. Cochrane Database Syst Rev 2014; 2014(4):CD011063. doi: 10.1002/14651858.cd011063 [Crossref] [ Google Scholar]
- Çelik Köycü B, Imirzalioğlu P, Özden UA. Three-dimensional finite element analysis of stress distribution in inlay-restored mandibular first molar under simultaneous thermomechanical loads. Dent Mater J 2016; 35(2):180-6. doi: 10.4012/dmj.2014-341 [Crossref] [ Google Scholar]
- The glossary of prosthodontic terms: ninth edition. J Prosthet Dent 2017;117(5S):e1-e105. 10.1016/j.prosdent.2016.12.001.
- Edelhoff D, Sorensen JA. Tooth structure removal associated with various preparation designs for posterior teeth. Int J Periodontics Restorative Dent 2002; 22(3):241-9. [ Google Scholar]
- Morimoto S, Rebello de Sampaio FB, Braga MM, Sesma N, Özcan M. Survival rate of resin and ceramic inlays, onlays, and overlays: a systematic review and meta-analysis. J Dent Res 2016; 95(9):985-94. doi: 10.1177/0022034516652848 [Crossref] [ Google Scholar]
- Jiang W, Bo H, Yongchun G, LongXing N. Stress distribution in molars restored with inlays or onlays with or without endodontic treatment: a three-dimensional finite element analysis. J Prosthet Dent 2010; 103(1):6-12. doi: 10.1016/s0022-3913(09)60206-7 [Crossref] [ Google Scholar]
- Cangul S, Adiguzel O. The latest developments related to composite resins. Int Dent Res 2017; 7(2):32-41. doi: 10.5577/intdentres.2017.vol7.no2.3 [Crossref] [ Google Scholar]
- 3M, ESPE, USA, Filtek Supreme Ultra Universal Restorative. USA. Available from: https://multimedia.3m.com/mws/media/1363018O/3m-filtek-supreme-ultra-universal-restorative-technical-product-profile.pdf. Updated 2020. Accessed November 8, 2020.
- Hopp CD, Land MF. Considerations for ceramic inlays in posterior teeth: a review. Clin Cosmet Investig Dent 2013; 5:21-32. doi: 10.2147/ccide.s42016 [Crossref] [ Google Scholar]
- Dejak B, Młotkowski A. A comparison of mvM stress of inlays, onlays and endocrowns made from various materials and their bonding with molars in a computer simulation of mastication - FEA. Dent Mater 2020; 36(7):854-64. doi: 10.1016/j.dental.2020.04.007 [Crossref] [ Google Scholar]
- Gracis S, Thompson VP, Ferencz JL, Silva NR, Bonfante EA. A new classification system for all-ceramic and ceramic-like restorative materials. Int J Prosthodont 2015; 28(3):227-35. doi: 10.11607/ijp.4244 [Crossref] [ Google Scholar]
- Mainjot AK, Dupont NM, Oudkerk JC, Dewael TY, Sadoun MJ. From artisanal to CAD-CAM blocks: state of the art of indirect composites. J Dent Res 2016; 95(5):487-95. doi: 10.1177/0022034516634286 [Crossref] [ Google Scholar]
- Della Bona A, Corazza PH, Zhang Y. Characterization of a polymer-infiltrated ceramic-network material. Dent Mater 2014; 30(5):564-9. doi: 10.1016/j.dental.2014.02.019 [Crossref] [ Google Scholar]
- Yang H, Park C, Shin JH, Yun KD, Lim HP, Park SW. Stress distribution in premolars restored with inlays or onlays: 3D finite element analysis. J Adv Prosthodont 2018; 10(3):184-90. doi: 10.4047/jap.2018.10.3.184 [Crossref] [ Google Scholar]
- Saridag S, Sevimay M, Pekkan G. Fracture resistance of teeth restored with all-ceramic inlays and onlays: an in vitro study. Oper Dent 2013; 38(6):626-34. doi: 10.2341/12-211-l [Crossref] [ Google Scholar]
- Ilgenstein I, Zitzmann NU, Bühler J, Wegehaupt FJ, Attin T, Weiger R. Influence of proximal box elevation on the marginal quality and fracture behavior of root-filled molars restored with CAD/CAM ceramic or composite onlays. Clin Oral Investig 2015; 19(5):1021-8. doi: 10.1007/s00784-014-1325-z [Crossref] [ Google Scholar]
- Amesti-Garaizabal A, Agustín-Panadero R, Verdejo-Solá B, Fons-Font A, Fernández-Estevan L, Montiel-Company J. Fracture resistance of partial indirect restorations made with CAD/CAM technology A systematic review and meta-analysis. J Clin Med 2019; 8(11):1932. doi: 10.3390/jcm8111932 [Crossref] [ Google Scholar]
- Yamanel K, Caglar A, Gülsahi K, Ozden UA. Effects of different ceramic and composite materials on stress distribution in inlay and onlay cavities: 3D finite element analysis. Dent Mater J 2009; 28(6):661-70. doi: 10.4012/dmj.28.661 [Crossref] [ Google Scholar]
- Lin CL, Chang CH, Wang CH, Ko CC, Lee HE. Numerical investigation of the factors affecting interfacial stresses in an MOD restored tooth by auto-meshed finite element method. J Oral Rehabil 2001; 28(6):517-25. doi: 10.1046/j.1365-2842.2001.00689.x [Crossref] [ Google Scholar]
- Vita Zahnfabrik, Vita Enamic, Technical and scientific documentation. Germany. Available from: https://www.vita-zahnfabrik.com/en/VITA-ENAMIC-24970.html. Updated 2020. Accessed November 8, 2020.
- Belli R, Wendler M, de Ligny D, Cicconi MR, Petschelt A, Peterlik H. Chairside CAD/CAM materials Part 1: measurement of elastic constants and microstructural characterization. Dent Mater 2017; 33(1):84-98. doi: 10.1016/j.dental.2016.10.009 [Crossref] [ Google Scholar]
- Gulec L, Ulusoy N. Effect of endocrown restorations with different CAD/CAM materials: 3D finite element and weibull analyses. Biomed Res Int 2017; 2017:5638683. doi: 10.1155/2017/5638683 [Crossref] [ Google Scholar]
- Rosenstiel SF, Land MF, Fujimoto J. Contemporary Fixed Prosthodontics-E-Book. 5th ed. China: Elsevier Health Sciences; 2015.
- Mei ML, Chen YM, Li H, Chu CH. Influence of the indirect restoration design on the fracture resistance: a finite element study. Biomed Eng Online 2016; 15(1):3. doi: 10.1186/s12938-015-0115-4 [Crossref] [ Google Scholar]
- Yu P, Xiong Y, Zhao P, Xu Z, Yu H, Arola D. On the wear behavior and damage mechanism of bonded interface: ceramic vs resin composite inlays. J Mech Behav Biomed Mater 2020; 101:103430. doi: 10.1016/j.jmbbm.2019.103430 [Crossref] [ Google Scholar]
- Costa A, Xavier T, Noritomi P, Saavedra G, Borges A. The influence of elastic modulus of inlay materials on stress distribution and fracture of premolars. Oper Dent 2014; 39(4):E160-70. doi: 10.2341/13-092-l [Crossref] [ Google Scholar]
- Chang YH, Lin WH, Kuo WC, Chang CY, Lin CL. Mechanical interactions of cuspal-coverage designs and cement thickness in a cusp-replacing ceramic premolar restoration: a finite element study. Med Biol Eng Comput 2009; 47(4):367-74. doi: 10.1007/s11517-008-0379-y [Crossref] [ Google Scholar]