Avicenna J Dent Res. 14(3):125-129.
doi: 10.34172/ajdr.2022.23
Original Article
Evaluation of the Effects of Using Buccal Fat Pad on Dorsum Changes: A Randomized Clinical Trial
Mohammad Reza Jamalpour 1, *  , Arsalan Ebrahimifard 2
, Arsalan Ebrahimifard 2  , Maryam Farhadian 3
, Maryam Farhadian 3
Author information:
1Associate Professor of Oral and Maxillofacial Surgery, School of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran
2Department of Oral and Maxillofacial Surgery, School of Dentistry Lorestan University of Medical Sciences,, Khorramabad, Iran
3Associate Professor of Biostatistics, School of Health, Hamadan University of Medical Sciences, Hamadan, Iran
Abstract
Background: Irregularity of the dorsum is one of the common complications in rhinoplasty. Today, various
methods are used to correct the irregularity of the dorsum. This study was conducted to determine the effects of using a buccal fat pad (BFP) on dorsum changes.
Methods: In this randomized clinical trial, 20 patients undergoing primary rhinoplasty with the open
technique were randomly assigned to the intervention and control groups. In the intervention group, a layer of buccal fat was placed on the dorsum and fixed after the end of the osteotomy and before the suture of the skin. In the control group, the dorsum region was sutured without the use of the buccal fat. Both groups were followed for six months and assessed regarding changes in the dorsum and satisfaction with dorsum aesthetics.
Results: In the intervention and control groups, the mean age of patients was 26.60 ± 3.92 and 25.90 ± 4.38 years, respectively (P = 0.711). In terms of gender, 70% and 80% in the intervention and control groups were women, respectively. The frequencies of nasal asymmetry, nasal depression, dorsum narrowing, step, and nasal width in the intervention and control groups were 20% and 50% (P = 0.350). The mean score of patient satisfaction and surgeon satisfaction with the beauty of the bridge of the nose in the intervention group was significantly higher than that of the control group (P < 0.05).
Conclusions: Using BFP on the dorsum during primary rhinoplasty, in addition to reducing changes in the
dorsum, increased the satisfaction of dorsum beauty.
Keywords: Buccal fat, Dorsum, Nasal irregularities
Copyright and License Information
© 2022 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Jamalpour MR, Ebrahimifard A, Farhadian M. Evaluation of the effects of using buccal fat pad on dorsum changes: a randomized clinical trial. Avicenna J Dent Res. 2022; 14(3):125-129. doi:10.34172/ajdr.2022. 23
Introduction
Strengthening the dorsum is performed for various reasons such as cosmetic problems or correction of defects such as deformity or dropping the tip of the nose (1). In addition, in cases where the dorsal hump reduction is greater than 3 mm, there is a weak upper lateral crus and asymmetry of the dorsum. Surgeons usually use grafts during the surgery to help support the dorsum area (2,3).
Nowadays, various methods such as nasal septum cartilage (4), cartilage obtained from the ear (5) or ribs (6), silicone or Gore-Tex prostheses (7), and injection of gels and fillers are employed to fill the back of the nose and correct its problems. However, none of these products have the quality of the adipose tissue, which can be applied as a filler reference through volumetric quality and nutritional effect on the skin (8).
Regardless of the origin of the removed graft, autogenous grafts are used more. These grafts have fewer postoperative complications, accessibility, and better integration (9). The results of some studies have shown that in correcting irregularities in the dorsal region of the nose, autogenous cartilaginous grafts, in addition to ease of harvest and shorter time of surgery, have not caused any serious complications at the site of resection. Further, examining the angle of the inner valve of the nasal cartilage revealed an expected effect on the acellular dermis and the solvent-dehydrated pericardium (10).
Another method of autogenous grafts is the buccal fat pad (BFP). Egyedi first used BFPs in 1977 to repair oral lesions larger than 4 cm in diameter in four patients with tumors (11). This graft can be applied as an alternative for correcting limited changes in the facial area. Considering that the fat structure is well maintained, this tissue can maintain volume and stability. Furthermore, the complications of the removal site and the damage to the removed tissue are minimized by removing the BFP via a small incision inside the oral cavity. By splitting the buccinator muscle, the BFP capsule is carefully extracted to prevent damage (12). Anatomically, BFP is an encapsulated, round, convex, and predominantly fatty form with an excellent maxillary nutritional supply (13-15).
Buccal fat is employed in various lesions of the face and inside the mouth (12,16-21). However, a limited body of research has so far focused on the use of BFP to correct changes in the dorsum area. Therefore, the current study evaluated the effect of using BFP on the beauty and appearance of the dorsal region of the nose and the satisfaction of patients and surgeons with the beauty of the dorsum of the nose after the surgery.
Materials and Methods
In this one-blind clinical trial, 20 consecutive primary rhinoplasty patients, who referred to a private surgical center and met the inclusion criteria, were selected by available and continuous sampling. After obtaining written and informed consent from patients, they were assigned to two intervention and control groups using a quadruple randomization block. In both groups, surgery was performed based on the open method. In the intervention group, after the end of osteotomy and before skin suture, the BFP accessed the main buccal site of the cheek fat in the cheek by creating a step incision in the area behind the zygomatic batter at the periphery of the Stenson duct, and then was released and exited by blunt dissection fat (Figure 1). The incision site did not require a suture.

Figure 1.
How to Remove Buccal Fat and Place it on the Dorsal Nasal.
.
How to Remove Buccal Fat and Place it on the Dorsal Nasal.
A layer of BFP was placed on the dorsum and fixed to the skin with a 5-0 nylon suture while the splint was on the nose, after which the adhesive on the nose helped fix it. The control group underwent routine rhinoplasty surgery without the use of the buccal fat. Splints were removed in all patients on the eighth day after the surgery immediately after split removal and 2, 4, and 6 months after the surgery, and both groups were examined by a fellow maxillofacial surgeon (except for the person who operated on the patients and without knowing the type of the intervention). First, patients’ satisfaction with the beauty of the nasal dorsum was measured with the visual analog scale (VAS) scale. The surgeon then recorded his satisfaction with the beauty of the dorsum with the same scale. Moreover, the surgeon evaluated the presence of complications in the dorsum of the nose, including the presence of step, and narrowing and widening of the dorsum, as well as the asymmetry and depression of the dorsum of the nose, and the results were recorded in a checklist.
The exclusion criteria included the age range of 18-40, ASA class I, dorsal reduction of 3 mm and more than the inclusion criteria and a history of nasal fracture, cleft rhinoplasty, postoperative nasal trauma, history of respiratory problems in the nasal area, history of rhinoplasty, and lack of access to the patient to follow up the rhinoplasty result for any reason.
Data were analyzed by SPSS statistical software, version 21. Means and standard deviations were used to describe quantitative data and tables, graphs, and frequency percentages were applied to explain qualitative data. In addition, Fisher’s exact test was employed to compare the frequency of complications in the two groups, and Student’s t test or Mann-Whitney U test was utilized to compare the patients’ satisfaction with the appearance of the nose. Additionally, the variance analysis test of repeated observations was used to compare the VAS score of patients in different time periods. All data were analyzed at a confidence level of 95%, and the significance level was less than 0.05.
Results
In this study, 20 patients who were candidates for primary rhinoplasty surgery in two equal groups of 10 intervention and control patients underwent rhinoplasty with the open technique. The outcomes of rhinoplasty, including nasal asymmetry, dorsum depression, dorsum widening and narrowing, the presence of a dorsum or step in the dorsum, and the patient’s and surgeon’s satisfaction with the nasal dorsum were evaluated in four time periods during 6 months. The mean age of patients in the intervention and control groups was 25.20 ± 4.04 and 25.47 ± 2.82 years (P = 0.711), respectively. In terms of gender, the majority of cases (70% and 80%) were women in the intervention and control groups (P = 1.00), respectively. During a 6-month follow-up of patients, 1 case of dorsum depression (the fourth month) and 1 case of step (sixth month) were observed in the intervention group; but no cases of asymmetry, widening, and narrowing of the dorsum were detected in this group. Asymmetry (n=1, fourth month), nasal depression (n=1, fourth month), step just (n=1, fourth month), and step with depression (n=1, sixth months) were found in the control group. Totally, 2 and 5 patients in the intervention and control groups had changes in the dorsum, respectively (Table 1). No cases of widening or narrowing of the dorsum were observed in the intervention and control groups.
Table 1.
Frequency of Dorsum Changes During the Six-month follow-up of patients of Intervention and Control Groups
|
Dorsum Changes
|
Treatment Group
|
P Value
|
|
Intervention No. (%)
|
Control No. (%)
|
| Asymmetry |
0 (0) |
1 (10) |
1.00 |
| Dorsum depression |
1 (10) |
1 (10) |
0.582 |
| Step of dorsum |
1 (10) |
2 (20) |
0.582 |
| Step depression |
0 (0) |
1 (10) |
1.00 |
| Total |
2 (20) |
5 (50) |
0.350 |
Out of 10 patients in the intervention group, 2 (20%) had complications at the removal site of fat pad graft, including 1 case of abscess and 1 case of hematoma.
There was no significant difference between the intervention and control groups in terms of satisfaction with the dorsum in times immediately after splint removal in the second and sixth month of evaluation. However, in the fourth month of evaluation, the mean score of satisfaction with the dorsum in the intervention group was significantly (P = 0.015) higher compared to the control group. The mean score of surgeon satisfaction with the appearance of the dorsum in all four stages of the evaluation of the intervention group was significantly (P < 0.05) higher than that of the control group (Table 2).
Table 2.
Mean Frequency of (SD) Patients’ Satisfaction From Dorsum in the Intervention and Control Groups
|
Evaluation Time
|
Treatment Group
|
P Value
|
Intervention
Mean ± SD
|
Control
Mean ± SD
|
| Patient satisfaction |
| Just after splint removal |
6.90±0.58 |
6.40±0.97 |
0.247* |
| Second month |
7.60±0.52 |
6.90±4.29 |
0.128* |
| Fourth month |
48.00±0.82 |
6.60±1.43 |
0.015* |
| Sixth month |
8.80±1.55 |
7.20±2.04 |
0.064* |
| Surgeon satisfaction just after splint removal |
7.90±0.32 |
7.10±0.88 |
0.043* |
| Second month |
8.10±0.57 |
7.10±1.10 |
0.029* |
| Fourth month |
8.60±0.87 |
7.20±1.40 |
0.018* |
| Sixth month |
8.90±1.60 |
7.40±1.58 |
0.049* |
Note. * Mann-Whitney U test; ** Student’s t-test.
Based on the results of the variance analysis test of repeated observations, a significant difference (P = 0.031) was found between the patients in the intervention and control groups regarding satisfaction with the dorsum (Figure 2). Moreover, there was a significant difference (P = 0.018) between the surgeon’s satisfaction with the appearance of the nose in the intervention and control groups (Figure 3).

Figure 2.
Score Frequency of Patients’ Satisfaction From Dorsum Six Months After Surgery.
.
Score Frequency of Patients’ Satisfaction From Dorsum Six Months After Surgery.
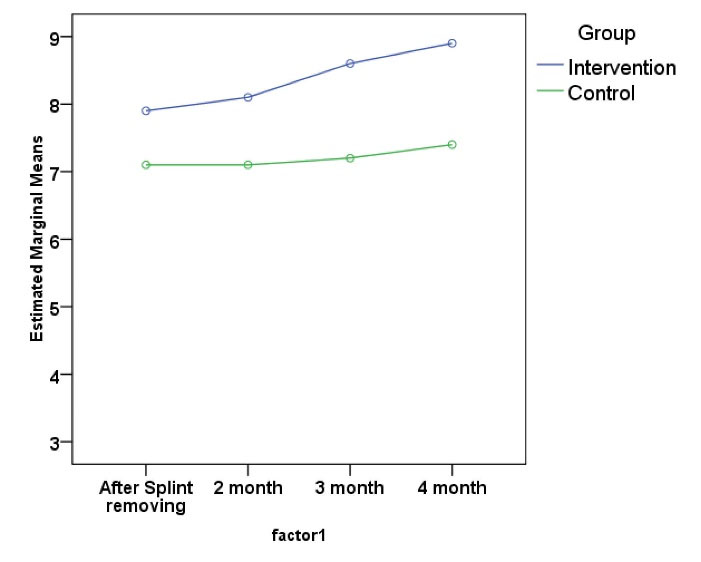
Figure 3.
Score Frequency of Surgeon Satisfaction From the Dorsum Area Six Months After Surgery.
.
Score Frequency of Surgeon Satisfaction From the Dorsum Area Six Months After Surgery.
Discussion
The idea of using buccal fat to prevent dorsum changes was taken from two studies conducted by Zhang et al (17) and Khiabani et al (16). In their study, Zhang et al used buccal fat to repair the nose in eight children with cleft palates and reported no postoperative complications, including infection, perforation, facial nerve damage, and duct stenosis. No change was observed in the contour following the follow-up. Similarly, the site of the buccal fat was not easily distinguishable, and no asymmetry was found in the face. In the clinical trial of Khiabani et al, the buccal fat was employed to repair the cheek and strengthen the malar in 13 trauma patients. No complications were reported, including prolonged bruising, extensive hematoma, severe pain, asymmetry, and parotid duct damage. In the present study, the buccal fat was used to repair the dorsum in rhinoplasty surgery. No major complication was found at the fat removal site; only two cases of abscess and hematoma were recovered based on reports.
In a study by Baptista et al, in 20 patients with dorsal irregularities, inverted V-deformity, visible lateral osteotomies, and dorsum depressions, the irregular area was healed using autologous fat removed from the under-skin of the abdomen. Patients were followed up for 18-24 months. Overall, 90% of patients were satisfied with the postoperative cosmetic results, and two cases needed re-surgery. Researchers believe that repairing dorsum irregularities with fat is a simple and reliable method to correct defects after rhinoplasty (18). In the present study, 20 patients were examined, and the difference was that patients were randomly allocated to intervention and control groups. Buccal fat was used instead of belly fat to prevent irregularities rather than for correcting irregularities. Consistent with the findings of Baptista et al, in the present study, using buccal fat for preventing changes in the dorsal region of the nose following primary rhinoplasty increased patients’ satisfaction with the appearance of the nose.
Regarding the other applications of buccal fat in oral and maxillofacial surgeries, Singh et al identified 27 related articles (2004-2009) that were all in the form of case series or case reports. The results of the study showed that buccal fat was used more to close oral fistulas and then maxillary defects, cleft palate and mucosal defects, and buccal fat, due to its favorable anatomical position, high blood vessels, ease of access, and low refractive index, has become a selective flap for the reconstruction of oral and maxillary defects (19). The present study was performed as a clinical trial which is more valuable than the case series or case report studies due to the selection of the control group and the random allocation of patients to the intervention and control groups. In the current study, buccal fat was considered to prevent changes in the dorsum following primary rhinoplasty, which had good results both at the removal and plant sites of the graft.
Regarding the complications of the buccal fat removal site and its effect on facial beauty, Moura et al reviewed 5 related clinical trials and found that 8.45% of patients had minor complications. No cases of parotid duct injury and facial nerve injury were observed in their study (20). In the present study, no major complication was detected at the buccal fat removal site. There were two minor complications (i.e., abscess and hematoma) during splint resection, which improved with medication and care recommendations.
In another study, Kim et al reported how cut, harvested, and harvested buccal fat was used to repair facial lesions and improve beauty. According to their findings, buccal fat removal, without causing damage at the removal site, is an easy and accessible graft in repairing the minor deformities of the facial contour. This graft can be employed to replace the volume and strengthen the tip of the nose for the beauty of rhinoplasty (12). As mentioned earlier, the current study investigated the effect of the buccal graft on changes in the dorsum area, which was satisfactory for both patients and surgeons.
Likewise, Chakrabarti et al studied their clinical experiences regarding the indications, benefits, and complications of using the buccal fat in the repair of cancerous lesions removed orally. Their results revealed that most patients have no complications immediately after the surgery. The signs of epithelialization occur in the first week after buccal fat transplantation and complete epithelialization at the end of the first month. The thin layer of the fibrous tissue under the epithelialized mucosa is then replaced with the buccal fat. The observed complications included bleeding (10.3%) and hematoma, leading to severe fibrosis (3.4%). The researchers concluded that the buccal fat with ease of access and low morbidity is a reliable method for repairing mild to moderate oral lesions even in the elderly who cannot tolerate long procedures (21). Similarly, Toshihiro et al evaluated the effect of buccal fat grafts on the repair of oral lesions caused by surgery and reported that it seems possible to use buccal fat grafts to repair defects caused by oral surgery (22). Based on the available observations, buccal fat with minimal complications and adverse consequences can have several applications in the repair of oral and facial lesions. It is safe to indicate that the present study is the first of its kind to investigate the effect of buccal fat on changes in the dorsum using a clinical trial.
Conclusions
The use of buccal fat in the dorsum area during primary rhinoplasty in patients aged 18-40 years who have a reduction in the dorsal area of 3 mm and more, could increase the patient’s and surgeon’s satisfaction with the beauty of the dorsum area of the nose in addition to reducing changes in the dorsum area. Conducting research in the form of a clinical trial by the selection of a control group and random assignment of groups is one of the strengths of the study. However, due to the lack of sample size in the intervention and control groups, the results should be generalized with caution.
Authors’ Contributions
AE, Mj, and MF contributed to the study design, data collection, analysis, and interpretation, and manuscript preparation.
Conflict of Interest Disclosures
The authors declare that they have no conflict of interests.
Ethical Statement
The research Ethics Committee of Hamadan University of Medical Sciences approved this study (code: IR.UMSHA.REC.1398.006).
References
- Berghaus A, Stelter K. Alloplastic materials in rhinoplasty. Curr Opin Otolaryngol Head Neck Surg 2006; 14(4):270-7. doi: 10.1097/01.moo.0000233599.14671.4a [Crossref] [ Google Scholar]
- Davis RE. Rhinoplasty and concepts of facial beauty. Facial Plast Surg 2006; 22(3):198-203. doi: 10.1055/s-2006-950178 [Crossref] [ Google Scholar]
- Springer IN, Zernial O, Nölke F, Warnke PH, Wiltfang J, Russo PAJ. Gender and nasal shape: measures for rhinoplasty. Plast Reconstr Surg 2008; 121(2):629-37. doi: 10.1097/01.prs.0000298095.18943.72 [Crossref] [ Google Scholar]
- Mizuno T. A new technique for augmentation rhinoplasty using hybrid autologous grafts with septal extension grafts in Asian patients. Facial Plast Surg 2019; 35(1):58-64. doi: 10.1055/s-0038-1666992 [Crossref] [ Google Scholar]
- Kridel RW, Sturm AK. Dorsal augmentation with homologous rib. Facial Plast Surg 2017; 33(2):195-201. doi: 10.1055/s-0037-1598031 [Crossref] [ Google Scholar]
- Wee JH, Park MH, Oh S, Jin HR. Complications associated with autologous rib cartilage use in rhinoplasty: a meta-analysis. JAMA Facial Plast Surg 2015; 17(1):49-55. doi: 10.1001/jamafacial.2014.914 [Crossref] [ Google Scholar]
- Erlich MA, Parhiscar A. Nasal dorsal augmentation with silicone implants. Facial Plast Surg 2003; 19(4):325-30. doi: 10.1055/s-2004-815652 [Crossref] [ Google Scholar]
- Mojallal A, Lequeux C, Shipkov C, Breton P, Foyatier JL, Braye F. Improvement of skin quality after fat grafting: clinical observation and an animal study. Plast Reconstr Surg 2009; 124(3):765-74. doi: 10.1097/PRS.0b013e3181b17b8f [Crossref] [ Google Scholar]
- Rohrich RJ, Adams WP, Ahmad J, Gunter J, editors. Dallas rhinoplasty: nasal surgery by the masters. CRC Press; 2014 Mar 4.
- Çöloğlu H, Uysal A, Tiftikçioğlu Y, Oruç M, Koçer U, Coşkun E. Comparison of autogenous cartilage, acellular dermis, and solvent-dehydrated pericardium for the prevention and correction of dorsal nasal irregularities: an experimental study. Aesthetic Plast Surg 2012; 36(3):732-41. doi: 10.1007/s00266-011-9865-y [Crossref] [ Google Scholar]
- Egyedi P. Utilization of the buccal fat pad for closure of oro-antral and/or oro-nasal communications. J Maxillofac Surg 1977; 5(4):241-4. doi: 10.1016/s0301-0503(77)80117-3 [Crossref] [ Google Scholar]
- Kim JT, Ho SYM, Hwang JH, Sung KY. Efficacy of the buccal fat pad graft in facial reconstruction and aesthetic augmentation. Plast Reconstr Surg 2014; 133(1):83e-5e. doi: 10.1097/01.prs.0000436800.27670.dd [Crossref] [ Google Scholar]
- Dubin B, Jackson IT, Halim A, Triplett WW, Ferreira M. Anatomy of the buccal fat pad and its clinical significance. Plast Reconstr Surg 1989; 83(2):257-64. doi: 10.1097/00006534-198902000-00009 [Crossref] [ Google Scholar]
- Tideman H, Bosanquet A, Scott J. Use of the buccal fat pad as a pedicled graft. J Oral Maxillofac Surg 1986; 44(6):435-40. doi: 10.1016/s0278-2391(86)80007-6 [Crossref] [ Google Scholar]
- Vuillemin T, Raveh J, Ramon Y. Reconstruction of the maxilla with bone grafts supported by the buccal fat pad. J Oral Maxillofac Surg 1988; 46(2):100-6. doi: 10.1016/0278-2391(88)90258-3 [Crossref] [ Google Scholar]
- Khiabani K, Keyhan SO, Varedi P, Hemmat S, Razmdideh R, Hoseini E. Buccal fat pad lifting: an alternative open technique for malar augmentation. J Oral Maxillofac Surg 2014; 72(2):403.e1-403. doi: 10.1016/j.joms.2013.10.002 [Crossref] [ Google Scholar]
- Zhang Q, Li L, Tan W, Chen L, Gao N, Bao C. Application of unilateral pedicled buccal fat pad for nasal membrane closure in the bilateral complete cleft palate. J Oral Maxillofac Surg 2010; 68(8):2029-32. doi: 10.1016/j.joms.2010.02.042 [Crossref] [ Google Scholar]
- Baptista C, Nguyen PS, Desouches C, Magalon G, Bardot J, Casanova D. Correction of sequelae of rhinoplasty by lipofilling. J Plast Reconstr Aesthet Surg 2013; 66(6):805-11. doi: 10.1016/j.bjps.2013.02.020 [Crossref] [ Google Scholar]
- Singh J, Prasad K, Lalitha RM, Ranganath K. Buccal pad of fat and its applications in oral and maxillofacial surgery: a review of published literature (February) 2004 to (July) 2009. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 110(6):698-705. doi: 10.1016/j.tripleo.2010.03.017 [Crossref] [ Google Scholar]
- Kim JT, Sasidaran R. Buccal fat pad: an effective option for facial reconstruction and aesthetic augmentation. Aesthetic Plast Surg 2017; 41(6):1362-74. doi: 10.1007/s00266-017-0962-4 [Crossref] [ Google Scholar]
- Chakrabarti J, Tekriwal R, Ganguli A, Ghosh S, Mishra PK. Pedicled buccal fat pad flap for intraoral malignant defects: a series of 29 cases. Indian J Plast Surg 2009; 42(1):36-42. doi: 10.4103/0970-0358.53010 [Crossref] [ Google Scholar]
- Toshihiro Y, Nariai Y, Takamura Y, Yoshimura H, Tobita T, Yoshino A. Applicability of buccal fat pad grafting for oral reconstruction. Int J Oral Maxillofac Surg 2013; 42(5):604-10. doi: 10.1016/j.ijom.2012.07.009 [Crossref] [ Google Scholar]