Avicenna J Dent Res. 14(4):190-193.
doi: 10.34172/ajdr.2022.532
Case Report
Deep Margin Elevation With Resin-modified Glass Ionomer in Posterior Adhesive Indirect Restorations Based on Biomimetic Principles: A Case Report
Elham Farhadi 1  , Ladan Ranjbar Omrani 2
, Ladan Ranjbar Omrani 2  , Taraneh Estedlal 3, Elham Ahmadi 3, *
, Taraneh Estedlal 3, Elham Ahmadi 3, * 
Author information:
1Restorative Department, Dental school, Arak university of medical sciences, Arak, Iran
2Restorative Department, Dental School, Tehran University of Medical Sciences, Tehran, Iran
3Department of Restorative Dentistry, School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran
Abstract
A ceramic onlay restoration is a more conservative treatment than full-coverage crowns for endodontically treated teeth (ETT); thus, it helps preserve the tooth structure. Deep margin elevation (DME) is a method to relocate subgingival margins into a more coronal position with resin-modified glass ionomer (RMGI) or direct composite resin before the cementation of the indirect restoration. A 33-year-old male was referred to restore two ETT (teeth N. 46 and 47) with extensive coronal defects extending subgingivally between two teeth. Tooth N. 47 could not undergo a crown lengthening (CL) procedure due to its short root trunk. DME with RMGI was done for both teeth before preparation for ceramic onlays. In this case, by following the principles of biomimetic dentistry, we aimed to restore the tooth defect with a material that bore all functional stresses, in addition to achieving esthetic. It seems that DME in combination with ceramic onlay restoration can be a conservative method to restore ETT in the posterior region. The goal of considering the principles of biomimetic dentistry is to maintain the function of teeth using a good bond to hard tissue that unifies the tooth and its restoration hence distributing the stresses through the tooth as a unit with near-normal functional, biological, and esthetic features.
Keywords: Biomimetic, Dental onlays, Endodontically-treated teeth
Copyright and License Information
© 2022 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Farhadi E, Ranjbar Omrani, L, Estedlal T, Ahmadi E.Deep margin elevation with resin-modified glass ionomer in posterior adhesive indirect restorations based on biomimetic principles: a case report. Avicenna J Dent Res. 2022; 14(4):190- 193. doi:10.34172/ajdr.2022.532
Introduction
Resorting the crown of endodontically treated teeth (ETT) is challenging. ETT are much more likely to fracture than vital teeth. A cusp coverage restoration is recommended, especially when the defect is extensive (1,2). Partial coverage crowns similar to ceramic onlays can be more conservative than full-coverage crowns for ETT (3,4).
Deep defects in teeth are associated with several clinical challenges, including difficulties in accessing, isolating, and controlling marginal adaptation and emergence profile. Two treatment options are used to manage these defects: crown lengthening (CL) surgery and deep margin elevation (DME). The CL procedure is limited when roots are short and bone removal leads to an undesirable crown/root ratio or exposure to furcation (5). Coronal relocation of subgingival margins, called DME, results in a more coronal margin by bonding several layers of direct resin composite to the deep margins (5,6). We can also use resin-modified glass ionomer (RMGI) in the DME procedure, which is biocompatible and much less sensitive to the technique and releases fluoride (7-9).
Biomimetic dentistry focuses on replicating natural tooth structures utilizing artificial materials which are called biomimetic materials. These attempts have been made to restore tooth structure by a hard tissue bond and to achieve its full function that unifies the tooth and its restoration and distributes the stresses throughout the tooth with near-normal functional, biological, and esthetic features (10,11).
Case Report
A 33-year-old male was presented to restore endodontically treated right lower molars one day after completing endodontic therapy (Figure 1A-C). Examination revealed deep margins in the distal wall of tooth N.46 and the mesial wall of tooth N.47. Based on clinical and radiographic findings and considering the opposing dentition with zirconia restorations, the fabrication of a direct restoration was ruled out. Following consultation with a periodontist, there were limitations to the CL procedure because when the roots are short, bone removal may lead to an undesirable crown/root ratio or exposure to furcation. The patient chose to save the teeth and restore them with indirect adhesive restoration, then teeth were isolated by a rubber dam (DermaDam, Ultradent Products).
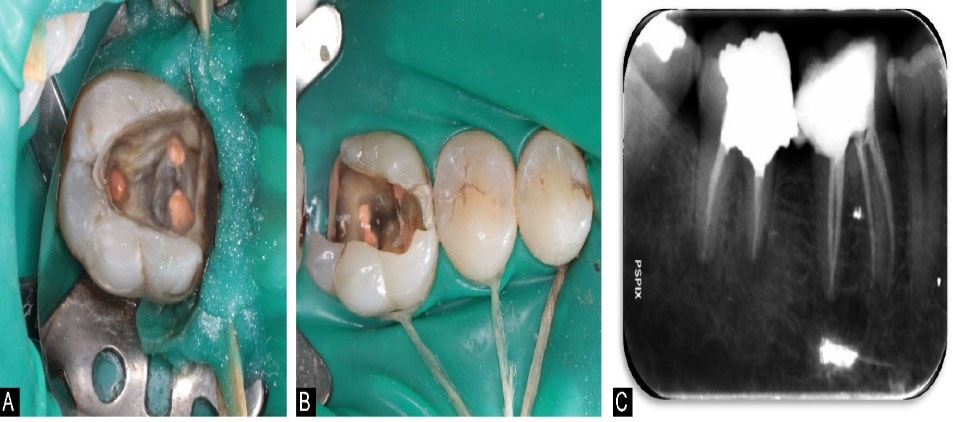
Figure 1.
(A) Clinical View of Tooth #47 Before Treatment. (B) Clinical View of Tooth #46 Before Treatment. (C) Periapical Radiograph of Teeth #46 and 47 Before Treatment
.
(A) Clinical View of Tooth #47 Before Treatment. (B) Clinical View of Tooth #46 Before Treatment. (C) Periapical Radiograph of Teeth #46 and 47 Before Treatment
Using an RMGI restorative material (Fuji II LC, GC Tokyo, Japan), deep margins were relocated coronally to prevent the violation of biological width in those areas. After placing a Matrix band (Dentsply Sirona, USA) and wooden wedges which were stabilized with a resin material (Gingival barrier), gingival dentin was conditioned (Fuji Conditioner, GC America), and the mixed Fuji II LC material was syringed into the location as much as the capacity of gingival papilla for 2 mm. Then, a LED-based curing light (Valo, Ultradent Products, 1000 mW/cm2, South Jordan, USA) was used to cure RMGI for 30 seconds. The RMGI layer was light-cured considering the buccal and lingual aspects for 30 seconds, after eliminating the matrix band (Figure 2). The cavity buildup was then completed with posterior resin composite (Filtek P60, 3M ESPE, Germany) and preparations were made for overlays (12). As observed in Figure 3, the preparation was done using butt joint preparation in the buccal and lingual walls on the enamel surface and slot preparation in the mesial and distal walls in both teeth (13).

Figure 2.
Teeth # 46, 47 After DME Procedure. Note. DEM: Deep margin elevation
.
Teeth # 46, 47 After DME Procedure. Note. DEM: Deep margin elevation

Figure 3.
The Cavity Build up With Posterior Resin Composite and in Teeth #46 and 47. Note. The preparation was completed using butt joint preparation in buccal and lingual walls on the enamel surface and slot preparation in the mesial and distal walls in both teeth.
.
The Cavity Build up With Posterior Resin Composite and in Teeth #46 and 47. Note. The preparation was completed using butt joint preparation in buccal and lingual walls on the enamel surface and slot preparation in the mesial and distal walls in both teeth.
Impressions were made using polyvinyl siloxanes (Express 3M ESPE) in a stock tray along with an impression using alginate (Alginoplast EM, Aroma Fine, Coe Alginate, and Jeltrate Plus) for the opposing arch. Lithium disilicate overlays (IPS e.max Press, Ivoclar Vivadent) were fabricated. Before cementation, restorations were examined for fitness and occlusion. A fine-grit football diamond bur (No. 8379 0014, Komet USA. Rock Hill, USA) was used to adjust restorations. We used diamond silicone polishing points (Dialite, Brasseler, USA) for the polishing step. The inner surface of overlays was etched and rinsed with 5% hydrofluoric acid (IPS Ceramic Etching Gel, Ivoclar Vivadent) for 20 seconds. Afterward, 37% phosphoric acid (BISCO Dental Products, USA) was rubbed on the etched area with a microbrush for 30 seconds and rinsed to eliminate porcelain residuum produced after hydrofluoric acid etching. An ultrasonic (Ultrasound Vita-Sonic II, Germany) was used to clean restorations for 5 minutes. After drying with air, a thin layer of silane (silane, Ultradent products) was applied for 1 minute, and a two-step etch and rinse dentin bonding system (Opti Bond Solo Plus, Kerr Corporation) was applied on the inner surface of the restorations and air-thinned. Next, a light protective barrier was placed on the restorations.
Enamel margins were etched for 15 seconds with the same 37% phosphoric acid, and more etchant was applied to build up material for 10 extra seconds and was rinsed for 15 seconds. High-volume suction was used to dry the surface. We applied two layers of a two-step etch and rinse dentin bonding system (OptiBond Solo Plus, Kerr Corporation) on the preparation surfaces of teeth and thinned them with a microbrush. After air-drying of the second layer and vaporization of its excessive solvent, it was polymerized for 20 seconds using a curing light.
For the cementation step, we used clear shade resin composite cement PANAVIA F.2 (PF2, Kuraray Noritake Dental). The extra resin cement was eliminated with the aid of a microbrush and dental floss. The polymerization of the resin cement was done for 20 seconds considering all aspects using a LED-based curing light. To polymerize any oxygen-inhibited layer, glycerin gel was applied to the margins, and they were light polymerized for 20 seconds again.
A minor occlusal adjustment was made, and the surface was polished using rubber points and fine grit diamond bur (Figure 4). A periapical radiograph was then taken to check marginal adaptation and removal of extra composite resin cement (Figure 5).

Figure 4.
Lithium Disilicate Overlays After Cementation
.
Lithium Disilicate Overlays After Cementation

Figure 5.
Preapical Radiograph of Teeth #46 and 47 After Overlays Cementation
.
Preapical Radiograph of Teeth #46 and 47 After Overlays Cementation
The restorations were followed with visual examination and radiographies six months later (Figure 6). The patient was asymptomatic without any evidence of fractures in restorations or teeth, carious lesions, or periodontal inflammation.

Figure 6.
Periapical Radiograph Six Months After Cementation
.
Periapical Radiograph Six Months After Cementation
Discussion
ETT may have deep subgingival margins which are technically challenging. For instance, placement of rubber dam, making an impression, and cementation are difficult, which affect the survival rate and health of periodontal tissue (14).
CL surgery has limitations in teeth with short root trunks, root proximity, and root concavities. DME is another method to relocate subgingival margins with RMGI or direct composite resin (15). The overall cumulative survival rate of 197 posterior teeth treated by DME technique followed by partial indirect restorations was reported to be 95.9% in12 years follow-up (16).
For the restoration described in the present study, RMGI restorative material was chosen for the DME procedure due to its ability to adhere chemically to the tooth structure, release of fluoride, biocompatibility to tissues, lower elastic modulus, resistance in streptococcus mutans, minor shrinkage stress, and hydrophilic nature which leads to unaffected microtensile bond strength when it has contact with water (17-19).
The build-up of the pulp chamber was performed (1) to follow the fundamental principle of IDS since it increases microtensile bond strength compared with delayed dentin sealing, (2) to block out the undercuts, (3) to achieve an accurate cavity geometry, and (4) to produce an optimal restoration material thickness (12).
Author Contributions
Conceptualization: Elham Farhadi.
Data curation: Elham Farhadi.
Formal Analysis: Elham Farhadi.
Funding acquisition: Elham Farhadi.
Investigation: Elham Farhadi.
Methodology: Elham Ahmadi.
Project administration: Elham Ahmadi.
Resources: Ladan Ranjbar Omrani.
Software: Elham Farhadi.
Supervision: Ladan Ranjbar Omrani.
Validation: Elham Ahmadi.
Visualization: Elham Farhadi.
Writing – original draft: Elham Farhadi.
Writing – review & editing: Taraneh Estedlal.
Conflict of Interest Disclosures
The authors declare that they have no conflict of interests.
Ethical Statement
Informed consent was obtained from the patient for the publication of this report.
References
- Atlas A, Grandini S, Martignoni M. Evidence-based treatment planning for the restoration of endodontically treated single teeth: importance of coronal seal, post vs no post, and indirect vs direct restoration. Quintessence Int 2019; 50(10):772-81. doi: 10.3290/j.qi.a43235 [Crossref] [ Google Scholar]
- Forster A, Braunitzer G, Tóth M, Szabó BP, Fráter M. In vitro fracture resistance of adhesively restored molar teeth with different MOD cavity dimensions. J Prosthodont 2019; 28(1):e325-e31. doi: 10.1111/jopr.12777 [Crossref] [ Google Scholar]
- Valizadeh S, Ranjbar Omrani L, Deliperi S, Sadeghi Mahounak F. Restoration of a nonvital tooth with fiber reinforce composite (wallpapering technique). Case Rep Dent 2020; 2020:9619787. doi: 10.1155/2020/9619787 [Crossref] [ Google Scholar]
- Abduo J, Sambrook RJ. Longevity of ceramic onlays: a systematic review. J Esthet Restor Dent 2018; 30(3):193-215. doi: 10.1111/jerd.12384 [Crossref] [ Google Scholar]
- Sarfati A, Tirlet G. Deep margin elevation versus crown lengthening: biologic width revisited. Int J Esthet Dent 2018; 13(3):334-56. [ Google Scholar]
- Magne P, Spreafico RC. Deep margin elevation: a paradigm shift. Am J Esthet Dent 2012; 2(2):86-96. [ Google Scholar]
- Santamaria MP, Suaid FF, Carvalho MD, Nociti FH Jr, Casati MZ, Sallum AW. Healing patterns after subgingival placement of a resin-modified glass-ionomer restoration: a histometric study in dogs. Int J Periodontics Restorative Dent 2013; 33(5):679-87. doi: 10.11607/prd.0396 [Crossref] [ Google Scholar]
- Valizadeh S, Farhadi E, Moradi A, Hashemikamangar SS. Evaluation of the Effect of Cold Plasma Treatment on the Microshear Bond Strength of Composite Resin Restorations to Dentin using Different Adhesive Systems and the Effect of Thermocycling. The Open Dentistry Journal 2021; 31:734-741. doi: 10.2174/1874210602115010734 [Crossref] [ Google Scholar]
- Gomes SC, Miranda LA, Soares I, Oppermann RV. Clinical and histologic evaluation of the periodontal response to restorative procedures in the dog. Int J Periodontics Restorative Dent 2005; 25(1):39-47. [ Google Scholar]
- Goswami S. Biomimetic dentistry. J Oral Res Rev 2018; 10(1):28-32. doi: 10.4103/jorr.jorr_3_17 [Crossref] [ Google Scholar]
- Zafar MS, Amin F, Fareed MA, Ghabbani H, Riaz S, Khurshid Z. Biomimetic aspects of restorative dentistry biomaterials. Biomimetics (Basel) 2020; 5(3):34. doi: 10.3390/biomimetics5030034 [Crossref] [ Google Scholar]
- Veneziani M. Posterior indirect adhesive restorations: updated indications and the morphology driven preparation technique. Int J Esthet Dent 2017; 12(2):204-30. [ Google Scholar]
- Ferraris F. Posterior indirect adhesive restorations (PIAR): preparation designs and adhesthetics clinical protocol. Int J Esthet Dent 2017; 12(4):482-502. [ Google Scholar]
- Opdam N, Frankenberger R, Magne P. From ‘Direct Versus Indirect’ Toward an Integrated Restorative Concept in the Posterior Dentition. Oper Dent 2016; 41(S7):S27-S34. doi: 10.2341/15-126-LIT [Crossref] [ Google Scholar]
- Dietschi D, Spreafico R. Current clinical concepts for adhesive cementation of tooth-colored posterior restorations. Pract Periodontics Aesthet Dent 1998; 10(1):47-54. [ Google Scholar]
- Bresser RA, Gerdolle D, van den Heijkant IA, Sluiter-Pouwels LMA, Cune MS, Gresnigt MMM. Up to 12 years clinical evaluation of 197 partial indirect restorations with deep margin elevation in the posterior region. J Dent 2019; 91:103227. doi: 10.1016/j.jdent.2019.103227 [Crossref] [ Google Scholar]
- Dragoo MR. Dragoo MRResin-ionomer and hybrid-ionomer cements: part IComparison of three materials for the treatment of subgingival root lesions. Int J Periodontics Restorative Dent 1996; 16(6):594-601. [ Google Scholar]
- Grubbs TD, Vargas M, Kolker J, Teixeira EC. Efficacy of direct restorative materials in proximal box elevation on the margin quality and fracture resistance of molars restored with CAD/CAM onlays. Oper Dent 2020; 45(1):52-61. doi: 10.2341/18-098-l [Crossref] [ Google Scholar]
- Dragoo MR. Resin-ionomer and hybrid-ionomer cements: part II, human clinical and histologic wound healing responses in specific periodontal lesions. Int J Periodontics Restorative Dent 1997; 17(1):75-87. [ Google Scholar]