Avicenna J Dent Res. 14(1):14-19.
doi: 10.34172/ajdr.2022.03
Original Article
Study of the Focal Aggregations of Cholesterol Crystals and Foamy Macrophages in the Chronic Periapical Lesions of Young and Elderly Patients
Parviz Deyhimi 1, *  , Saeedeh Khalesi 2
, Saeedeh Khalesi 2 
Author information:
1Professor of Oral and Maxillofacial Pathology, Department of Oral and Maxillofacial Pathology, Dental Research Center, School of Dentistry, Isfahan University of Medical Sciences, Isfahan, Iran
2Assistant Professor of Oral and Maxillofacial Pathology, Department of Oral and Maxillofacial Pathology, Dental Research Center, School of Dentistry, Isfahan University of Medical Sciences, Isfahan, Iran
*
Corresponding author: Parviz Deyhimi, Professor of Oral and Maxillofacial Pathology, Department of Oral and Maxillofacial Pathology, Dental Research Center, School of Dentistry, Isfahan University of Medical Sciences, Isfahan, Iran. Tel:+989133108898,+98-311- 37925579, Email:
Deihimy@dnt.mui.ac.ir
Abstract
Background: Cholesterol crystals and foamy macrophages can delay the healing of inflammatory periapical lesions. The purpose of this study was to evaluate the relationship between age and the presence of focal aggregations of cholesterol crystals and foamy macrophages in these lesions.
Methods: In this descriptive-analytic study, 770 samples of inflammatory periapical lesions including 335 periapical granulomas, 329 radicular cysts, and 106 residual periapical cysts were evaluated histopathologically in order to find at least two focal aggregations of cholesterol crystals and foamy macrophages in two age groups of young (20-35 years old) and elderly (over 50 years old) adults. Finally, the data were entered into SPSS version 23.0 and analyzed using chi-square and Fisher’s exact tests.
Results: In the present study, 74.3% of the samples lacked at least two focal aggregations of foamy macrophages, and 84% of the samples lacked at least two focal aggregations of cholesterol crystals. The frequency of focal aggregations of cholesterol crystals was not significantly different between the two age groups (P=0.14). However, the frequency of foamy macrophages was significantly higher in the age group of young adults than in elderly adults (P=0.002).
Conclusions: According to the obtained results, it does not appear that the healing rate of periapical lesions in young and elderly adults has necessarily significant difference; and whereas, it is lower in the elderly adults than in young adults, probabely relates to factors other than the accumulation of cholesterol crystals or foamy macrophages.
Keywords: Cholesterol crystals, Foam cells, Periapical lesions
Copyright and License Information
© 2022 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Deyhimi P, Khalesi S. Study of the focal aggregations of cholesterol crystals and foamy macrophages in the chronic periapical lesions of young and elderly patients. Avicenna J Dent Res. 2022; 14(1):14-19. doi:10.34172/ajdr.2022.03
Background
One of the histopathological features of chronic periapical lesions that plays an important role in the persistence of these lesions is the aggregation of cholesterol crystals (1-4). Because these factors are present outside the root canal system, endodontic re-treatment is unlikely to eliminate these factors, thereby enhancing or sustaining the periapical lesion after treatment (5). In addition, bone erosion may be found in cholesterol granulomas that have expansive growth (6).
Cholesterol crystals can be found in both the lumen and the connective tissue wall of the radicular cysts as well as dental granuloma. Generally, foreign body giant cells and sometimes macrophages containing hemosiderin or fat (foam cells) are visible around these crystals (1,6-9). The prevalence of cholesterol crystals in periapical lesions varies between 18% and 44% of all lesions (10-13).
Although the mechanism of cholesterol crystal formation has not been clarified, studies have shown that these crystals are more common in cases where hemosiderin pigment is present. Therefore, the main reason for the formation of cholesterol crystals may be the disintegration of erythrocytes (9).
A close correlation between the occurrence of cholesterol and macrophages containing hemosiderin as well as free hemosiderin in tissues was found by Trott et al, but the results of regression analysis showed that only 35% of cholesterol may be formed from this association. Therefore, they suggested that slow but considerable accumulation of cholesterol could occur through degeneration and disintegration of lymphocytes, plasma cells, and macrophages taking part in the inflammatory process, with consequent release of cholesterol from their walls (11).
Based on the process of atheroma formation in atherosclerosis, Shear considered circulating plasma lipids as well as phospholipids absorbed by lymphatic vessels as other sources of cholesterol crystals in periapical cysts (14,15).
Slutzky-Goldberg et al investigated the prevalence of cholesterol crystals in periapical lesions in the age group of adolescents (aged 13 to 21) and the older group over 60 years old and found that the prevalence of these crystals was higher in the older age group than in the juvenile group. They concluded that the mechanism of accumulation of cholesterol crystals is probably similar to the process of developing atherosclerosis in coronary artery disease (16).
Additionally, foamy macrophages or foam cells, when present in large numbers or extensive clusters, are suggestive of a proliferative process or a localized bone reaction and periapical lesions exhibiting an abundance of these cells seem to be more aggressive (17,18). Their prevalence in these lesions has been found to be about 28% (13,16).
The prevalence of cholesterol crystals has been reported to be higher in radicular cysts than in periapical granuloma, but the prevalence of foamy macrophages has not been different between the two lesions which indicates that the presence of these two tissue elements does not necessarily correlate with each other (1,7,10,19,20).
Considering the negative role of cholesterol crystals and foamy macrophages in the healing of periapical lesions and the possible effect of aging on the further occurrence of these two tissue elements, the aim of this study was to determine the frequency of cholesterol crystals and foamy macrophages in two age groups of young and elderly adults and also the possibility of correlation between these two tissue elements.
Materials and Methods
In this cross-sectional, descriptive-analytic study, all samples registered in the archive of the Department of Oral & Maxillofacial Pathology of School of Dentistry at Isfahan University of Medical Sciences with the diagnosis of radicular cyst, periapical granuloma, and residual periapical cyst during the period of 20 years from 1996 to 2016 were investigated. All periapical lesions were caused by a defect in endodontic treatment. Diagnosis of residual periapical cyst was made based on clinical, radiographical, and histopathological features as well as dental history including the history of tooth extraction due to periapical lesion. Data of the patients were extracted from the records of the samples and then microscopic slides were studied histopathologically in two age groups of young (20-35 years) and elderly (over 50 years) adults.
All slides prepared from paraffin blocks and stained with hematoxylin-eosin were examined using an optical microscope (Nikon YS100, Japan) by two oral pathologists for the presence of at least two focal aggregations of cholesterol crystals and foamy macrophages at a magnification of 100X. For each sample, all microscopic slides in the archive (at least 3 slides) were examined and if needed, serial sections were prepared and stained based on tissue volume in paraffin blocks. Finally, the data were entered into SPSS version 23.0 and analyzed by chi-square and Fisher’s exact tests.
In contrast with other studies, in the present study, in order to accurately examine the presence of these two tissue elements, the presence of at least two focal aggregations of cholesterol crystals and foamy macrophages at a magnification of 100X was considered as a definite criterion for their presence. The presence of two focal aggregations was selected because in Sjogren’s syndrome which is an inflammatory and autoimmune process, the presence of at least two focal aggregations of lymphocytes (50 cells or more) at a microscopic magnification of 100X or field of 4 mm2 in lip biopsy has been suggested as a criterion for diagnosing Sjogren’s syndrome in order to differentiate it from usual sialadenitis (1).
Results
In the present study, 770 recorded samples with histopathologic diagnosis of inflammatory periapical lesions including 335 cases (43.5%) of periapical granuloma, 329 cases (42.7%) of radicular cysts and 106 cases (13.8%) of residual periapical cysts were investigated.
According to the obtained results, of the 770 samples studied, 572 cases (74.3%) did not have at least two focal aggregations of foamy macrophages, and 198 cases (25.7%) had at least two focal aggregations of foamy macrophages (Figure 1). Moreover, 647 cases (84%) did not have at least two focal aggregations of cholesterol crystals and 123 cases (16%) had at least two focal aggregations of cholesterol crystals (Figure 2).
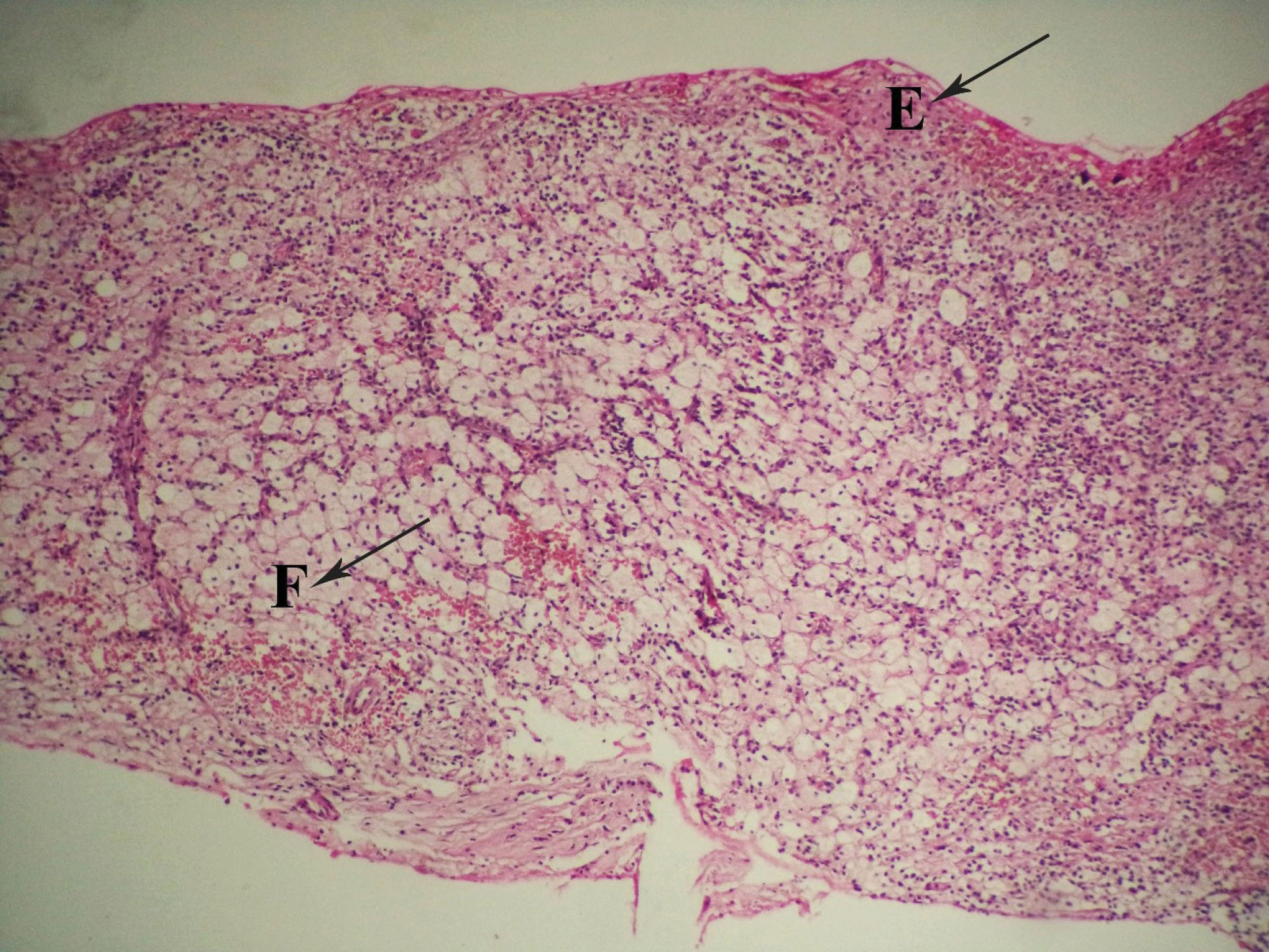
Figure 1.
Focal Aggregation of Foamy Macrophages in Radicular Cyst at a magnification of 100X (E: epithelium of radicular cyst, F: foamy macrophages).
.
Focal Aggregation of Foamy Macrophages in Radicular Cyst at a magnification of 100X (E: epithelium of radicular cyst, F: foamy macrophages).
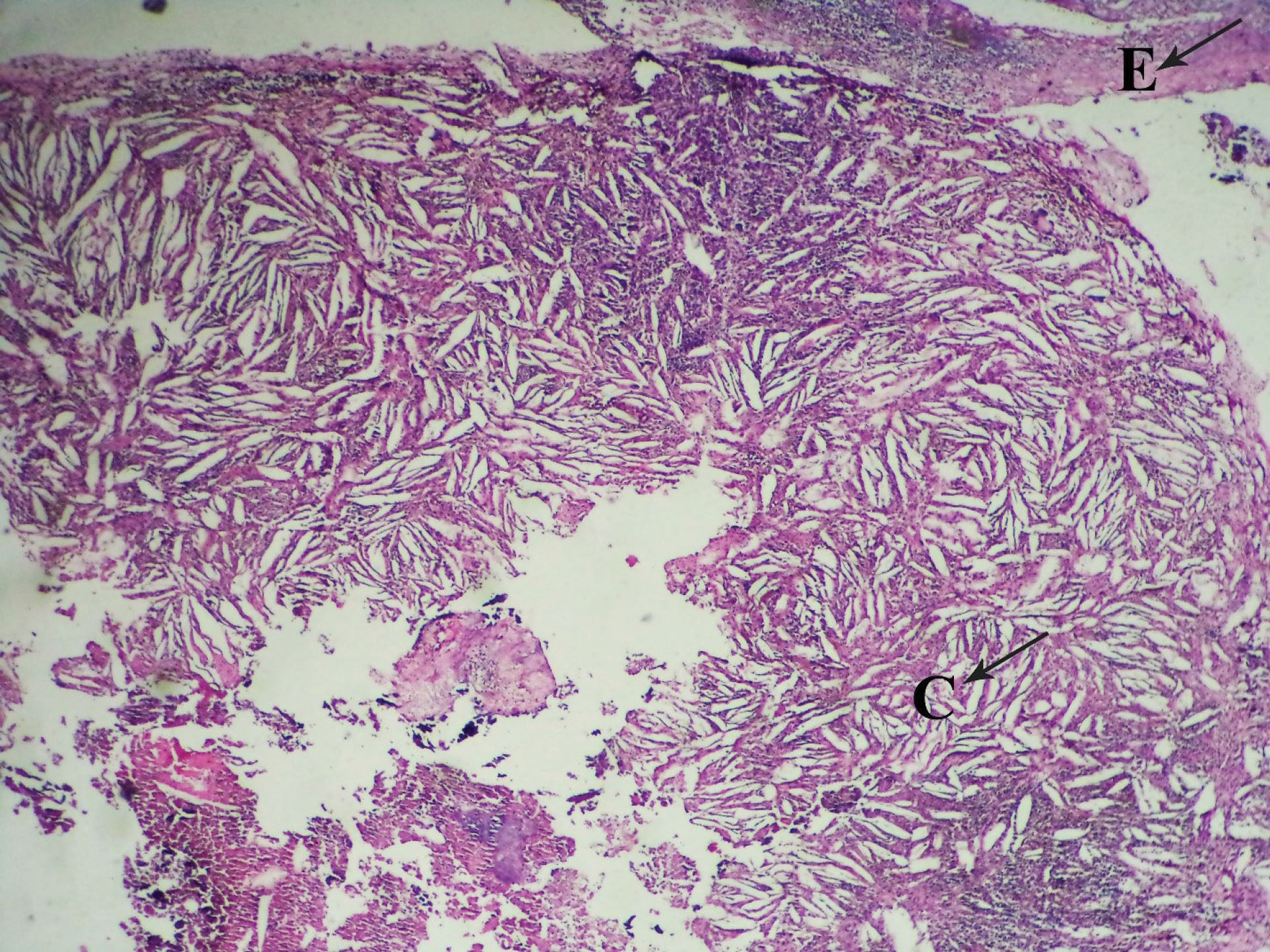
Figure 2.
Focal Aggregation of Cholesterol Crystals in Radicular Cyst at a magnification of 100X (E: epithelium of radicular cyst, C: cholesterol crystals).
.
Focal Aggregation of Cholesterol Crystals in Radicular Cyst at a magnification of 100X (E: epithelium of radicular cyst, C: cholesterol crystals).
Tables 1 and 2 show the frequency distribution of these structures among the three groups. According to the obtained results, the highest frequency of focal aggregations of cholesterol crystals was found in radicular cyst, followed by residual periapical cyst and periapical granuloma, respectively, indicating a significant difference between the three lesions (P = 0.014). Additionally, the highest frequency of focal aggregations of foamy macrophages was found in periapical granuloma, followed by radicular cyst and residual periapical cyst, respectively, indicating a significant difference between the three lesions (P < 0.001).
Table 1.
Frequency Distribution of Periapical Inflammatory Lesions Based on Presence of At Least Two Focal Aggregation of Cholesterol Clefts
|
Two Aggregation of Cholesterol Clefts
|
Periapical Granuloma
No. (%)
|
Radicular Cyst
No. (%)
|
Residual Periapical Cyst
No. (%)
|
Total
No. (%)
|
| Yes |
39 (11.6) |
65 (19.8) |
19 (17.9) |
123 (16) |
| No |
296 (88.4) |
264 (80.2) |
87 (82.1) |
647 (84) |
| Total |
335 (100) |
329 (100) |
106 (100) |
770 (100) |
Table 2.
Frequency Distribution of Periapical Inflammatory Lesions Based on Presence of At Least Two Focal Aggregation of Foamy Macrophages
|
Two Aggregation of Foam Cells
|
Periapical Granuloma
No. (%)
|
Radicular Cyst
No. (%)
|
Residual Periapical Cyst
No. (%)
|
Total
No. (%)
|
| Yes |
110 (32.8) |
79 (24) |
9 (8.5) |
198 (25.7) |
| No |
225 (67.2) |
250 (76) |
97 (91.5) |
572 (74.3) |
| Total |
335 (100) |
329 (100) |
106 (100) |
770 (100) |
Tables 3 and 4 show the frequency distribution of focal aggregations of cholesterol crystals and foamy macrophages according to the age range. According to the obtained results, there was no significant difference in the frequency of focal aggregations of cholesterol crystals between age groups of 20 to 35 years old and older than 50 years old (P = 0.14), but the frequency of focal aggregations of foamy macrophages was significantly higher in the age group of 20-35 years old than that in the age group of over 50 years old (P = 0.002).
Table 3.
Frequency Distribution of at Least Two Focal Aggregation of Cholesterol Clefts Based on Age Range
|
Age
|
Yes
n (%)
|
No
n (%)
|
Total
n (%)
|
| < 20 |
8 (6.5) |
109 (16.8) |
117 (15.2) |
| 20-35 |
59 (48) |
298 (46.1) |
357 (46.4) |
| 36-50 |
46 (37.4) |
155 (24) |
201 (26.1) |
| < 50 |
10 (8.1) |
85 (13.1) |
95 (12.3) |
| Total |
123 (100) |
647 (100) |
770 (100) |
Table 4.
Frequency Distribution of at Least Two Aggregation of Foamy Macrophages Based on Age Range
|
Age
|
Yes
n (%)
|
No
n (%)
|
Total
n (%)
|
| < 20 |
24 (12.1) |
93 (16.3) |
117 (15.2) |
| 20-35 |
106 (53.5) |
251 (43.9) |
357 (46.4) |
| 36-50 |
55 (27.8) |
146 (25.5) |
201 (26.1) |
| < 50 |
13 (6.6) |
82 (14.3) |
95 (12.3) |
| Total |
198 (100) |
572 (100) |
770 (100) |
Discussion
Various studies have been performed on the relationship between the presence of cholesterol crystals and foamy macrophages with age of the onset of periapical lesions; however, the results are inconsistent. For example, Slutzky-Goldberg et al observed a higher incidence of cholesterol crystals in elderly patients than in adolescent patients and considered this finding as a disruptive factor in the healing of these lesions in the elderly patients (16).
On the contrary, Plengwitthaya et al found no association between the presence of cholesterol crystals and age, gender, and location of periapical lesions (21).
Unfortunately, many studies on cholesterol crystals or foamy macrophages do not have a precise criterion for examining the presence of these two tissue elements.
Due to the fact that periapical lesions are inflammatory processes that occur following pulpitis, the scattered presence of cholesterol crystals and foamy macrophages in them is a common phenomenon. Therefore, only when their presence is considered a special and unusual phenomenon that their focal aggregations (at least two ones) can be taken into account.
In the present study, to achieve more accurate results, the aforementioned criterion was used and the number of samples was selected much higher than similar samples so that the results are more consistent with the population.
Indeed, the major reason for the difference in the results of different researches is the lack of precise or identical criteria for measuring these two tissue elements. In addition, the difference in the number of samples has not been ineffective in these discrepancies.
Although it is necessary to follow up the patients at different time intervals to compare carefully the extent of healing of periapical lesions in the above-mentioned two age groups, access to all the patients included in the study was not possible for us because we used archival samples from the oral pathology department over a period of 20 years. In addition, many patients may have lost their involved teeth within 20 years and patients over 50 years may have died for other reasons. Therefore, our conclusions from obtained results are based on various studies of reputable researchers about the negative role of cholesterol crystals and foamy macrophages in the healing of periapical lesions. However, we have not made a definite conclusion.
According to the results of the present study, because cholesterol crystals did not show a significant difference in the two age groups, it can be concluded that the healing of periapical lesions in the elderly patients is not necessarily lower compared to young patients, unless other factors are effective in healing which are not fully known.
Moreover, the prevalence of foamy macrophages in the young patients was significantly higher compared to the elderly patients, which confirms the above-mentioned conclusion. However, according to these findings, there appeared to be a difference in the occurrence of focal aggregations of cholesterol crystals and foamy macrophages. The question now is whether there is essentially a relationship between the occurrence of cholesterol crystals and foamy macrophages.
In many studies, such as the study conducted by Santos et al (18) and also the present study, the contiguity or concomitant presence of cholesterol crystals and foamy macrophages was not observed in most cases, while in some other studies such as the study by Slutzky-Goldberg et al (16), the close relationship between cholesterol crystals and foamy macrophages has been noted. However, in the study conducted by Slutzky-Goldberg et al (16), although foamy macrophages of periapical lesions were often found adjacent to cholesterol crystals, unlike cholesterol crystals, the difference in the incidence of foamy macrophages between the elderly and the young patients was not significant, which indicates that in many cases, as the study by Santos et al (18) and the present study, cholesterol crystals have been found alone without contiguity with foamy macrophages. In fact, although both cholesterol crystals and foamy macrophages are sometimes seen in a lesion, they are not necessarily adjacent to each other. Therefore, their occurrence may not be related to each other. Based on this, it can be concluded that the fat ingested by macrophages, which produces foam cells, is probably non-cholesterol fat or small cholesterol crystals in many cases. In confirmation of the above-mentioned conclusion, Santos et al according to their findings, concluded that the lack of correlation between these two tissue elements may be due to the fact that foamy macrophages already phagocytosed small lipid accumulations before the formation of larger crystals (18). Indeed, as various researchers have pointed out, phagocytosis by macrophages and foreign body giant cells may not occur in the presence of some large-diameter crystals, an event that releases cytokines such as IL-1 and damages the healing process after endodontic treatment which cause further bone loss and enlargement of the lesion. In other words, large cholesterol crystals resist internalization by macrophages and spread around to form the multinucleated giant cells. It is necessary to investigate whether these two types of phagocytic cells have no cholesterol digestive enzymes or cholesterol crystals are so large that they are not engulfed (3,4,13,18,22-25).
Moreover, according to various studies (19,21), including the present study, the prevalence of cholesterol crystals was significantly higher in radicular cysts compared with dental granulomas; however, the foamy macrophages were either not differentiated between the two lesions (19) or their prevalence was significantly higher in periapical granulomas compared with radicular cysts as reported in the present study. These findings also confirm the above-mentioned results indicating that there is not necessarily a correlation between the prevalence of cholesterol crystals and foamy macrophages.
The other hypothesis in this regard, which has been suggested by Slutzky-Goldberg et al, is that foamy macrophages may have been damaged during the preparation of sections, and if serial sections are performed, the correlative incidence of cholesterol crystals and foamy macrophages may be more recognizable in both young and old age groups (16). This argument does not seem logical. Due to the fact that the tissue cells have been fixed in the fixation solution, there is no reason that they are so damaged during the preparation of the sections that cannot be detected.
The relationship between the prevalence of cholesterol crystals and foamy macrophages with atherosclerotic plaques or atherosclerosis has been suggested by some researchers (16,26-28). Slutzky-Goldberg et al believe that the difference in the incidence of cholesterol crystals in periapical lesions among different age groups can be explained by the same risk factors associated with atherosclerosis, such as age, gender, and genetics (16). Moreover, Shear conclude that the level of blood lipids increases as age advances, which can increase the probability of occurrence of cholesterol crystals in periapical lesions, similar to the process that occurs in atherosclerosis (14,15).
It should be noted that the atheromatous plaques are characterized by the accumulation of smooth muscle cells, foamy macrophages, T lymphocytes, extracellular matrix including collagen, elastic fibers, proteoglycans, and intracellular and extracellular lipids, primarily cholesterol and cholesterol esters (29); however, it is noteworthy that the atherosclerotic plaques with the above-mentioned structural characteristics are not formed in the periapical region, and formation of these plaques is really an intimal reaction of the arterioles and arteries. Therefore, comparing their histopathologic characteristics with histopathological characteristics of periapical lesions does not seem logical. Additionally, although age is the most important cause of occurrence of atherosclerosis, in the present study, there was no significant difference in the prevalence of cholesterol crystals in the two age ranges of young and elderly patients, and the prevalence of foamy macrophages was significantly higher in the young age group. Therefore, there appeared to be no relationship between atherosclerosis and the presence of cholesterol crystals and foamy macrophages in periapical lesions.
According to the results obtained in this study, it does not appear that the origin of cholesterol crystals in periapical lesions is plasma lipids, because the amount of systemic lipids, in contrast with the obtained findings, increases with age. These results suggest that the origin of cholesterol crystals in the periapical lesions is more localized than that of systemic lipids. The obtained results may seem contradictory to the finding of a study by Alghofaily et al (30). In the study conducted by Alghofaily et al, a significant association was found between long-term statin intake and healing of periapical lesions after root canal treatment (30). Statins decrease the production of cholesterol and increase their elimination in patients with atherosclerosis; moreover, they have anti-inflammatory effects, stimulate the expression of bone anabolic factors and inhibit osteoclastogenesis (16,30). Therefore, their potential healing effects on the periapical lesions do not necessarily mean the similar mechanism of treatment of atherosclerosis.
Conclusions
According to the obtained results, it does not appear that the healing rate of periapical lesions in young and elderly adults has necessarily significant difference and whereas it is lower in the elderly adults than in young adults, probably relates to factors other than the accumulation of cholesterol crystals or foamy macrophages. However, for a definite conclusion, it is recommended that the healing stages of these lesions should be followed up in the above-mentioned two age groups at different time periods.
Authors’ Contribution
The role of Parviz deyhimi as first and corresponding author in this research is presentation of the study concept, study design, literature review, histopathological study, statistical analysis, manuscript preparation, editing and review.
The role of Saeedeh khalesi as second author in this research is literature review, histopathological study and statistical analysis.
Conflict of Interest Disclosures
The authors declare that there is no conflict of interest regarding the publication of this study.
Ethical Statement
The present study was adopted from the proposal number 297070 approved by vice-chancellery for research of Isfahan University of Medical Sciences (1397/255).
References
- Neville B, Damm DD, Allen C, Chi A. Oral and Maxillofacial Pathology. 4th ed. St. Louis: Elsevier; 2016. p. 111-39.
- Deyhimi P. Pathology of Tooth and Odontogenic Lesions. 1st ed. Isfahan: Kankash, Isfahan University of Medical Sciences Publication; 2006. p. 137-221. [Persian].
- Nair PN. Pathobiology of the periapex. In: Cohen S, Burns R, eds. Pathways of the Pulp. 8th ed. St. Louis: Mosby; 2002. p. 457-500.
- Nair PN. Cholesterol as an aetiological agent in endodontic failures--a review. Aust Endod J 1999; 25(1):19-26. doi: 10.1111/j.1747-4477.1999.tb00063.x [Crossref] [ Google Scholar]
- Bohra S, Bhede R, Saraf H, Chaudhary M, Swastika N, Hande A. Radicular cyst or odontogenic keratocyst? A case report. IOSR J Dent Med Sci 2014; 13(6):53-7. [ Google Scholar]
- Alkan A, Etoz O, Candirli C, Ulu M, Dayisoylu EH. Cholesterol granuloma of the jaws: report of two cases. J Pak Med Assoc 2014; 64(1):86-8. [ Google Scholar]
- Shafer W, Hine M, Levy B. Textbook of Oral Pathology. 4th ed. Philadelphia: Saunders; 1983. p. 479-510.
- Lee JH, Alrashdan MS, Ahn KM, Hong SP, Kim SM. Cholesterol granuloma in the wall of a mandibular dentigerous cyst: a rare case report. J Clin Exp Dent 2010; 2(2):e88-90. doi: 10.4317/jced.2.e88 [Crossref] [ Google Scholar]
- Browne RM. The origin of cholesterol in odontogenic cysts in man. Arch Oral Biol 1971; 16(1):107-13. doi: 10.1016/0003-9969(71)90141-5 [Crossref] [ Google Scholar]
- Dhirawani RB, Tegginamani AS, Sonalika WG. Evaluation of 115 radicular cysts: Histologic and etiopathogenic aspects for clinicians. Res Rev J Dent Sci 2014; 2(2):122-6. [ Google Scholar]
- Trott JR, Chebib F, Galindo Y. Factors related to cholesterol formation in cysts and granulomas. J Can Dent Assoc (Tor) 1973; 39(8):550-5. [ Google Scholar]
- Trott JR, Esty C. An analysis of 105 dental cysts. J Can Dent Assoc (Tor) 1972; 38(2):75-8. [ Google Scholar]
- Nair PN, Sjögren U, Sundqvist G. Cholesterol crystals as an etiological factor in non-resolving chronic inflammation: an experimental study in guinea pigs. Eur J Oral Sci 1998; 106(2 Pt 1):644-50. doi: 10.1046/j.0909-8836.1998.eos106206.x [Crossref] [ Google Scholar]
- Shear M. Cholesterol in dental cysts. Oral Surg Oral Med Oral Pathol 1963; 16:1465-73. doi: 10.1016/0030-4220(63)90384-0 [Crossref] [ Google Scholar]
- Shear M, Speight P. Cysts of the Oral Regions. 4th ed. Oxford: Blackwell Munksgaard; 2007. p. 123-42.
- Slutzky-Goldberg I, Baev V, Volkov A, Zini A, Tsesis I. Incidence of cholesterol in periapical biopsies among adolescent and elderly patients. J Endod 2013; 39(12):1477-80. doi: 10.1016/j.joen.2013.08.008 [Crossref] [ Google Scholar]
- Richardson J, Morgan P. Foam cell transformation in periapical lesions of endodontic origin. J Endod 1982; 8(12):563-6. doi: 10.1016/s0099-2399(82)80018-6 [Crossref] [ Google Scholar]
- Santos LC, Vilas Bôas DS, Oliveira GQ, Ramos EA, Gurgel CA, dos Santos JN. Histopathological study of radicular cysts diagnosed in a Brazilian population. Braz Dent J 2011; 22(6):449-54. doi: 10.1590/s0103-64402011000600002 [Crossref] [ Google Scholar]
- Lin HP, Chen HM, Yu CH, Kuo RC, Kuo YS, Wang YP. Clinicopathological study of 252 jaw bone periapical lesions from a private pathology laboratory. J Formos Med Assoc 2010; 109(11):810-8. doi: 10.1016/s0929-6646(10)60126-x [Crossref] [ Google Scholar]
- Chen JH, Tseng CH, Wang WC, Chen CY, Chuang FH, Chen YK. Clinicopathological analysis of 232 radicular cysts of the jawbone in a population of southern Taiwanese patients. Kaohsiung J Med Sci 2018; 34(4):249-54. doi: 10.1016/j.kjms.2018.01.011 [Crossref] [ Google Scholar]
- Plengwitthaya C, Dhanuthai K, Chantarangsu S, Ratisoontorn C. Cholesterol crystals in periapical lesions of root filled teeth. Int Endod J 2019; 52(4):484-90. doi: 10.1111/iej.13030 [Crossref] [ Google Scholar]
- Sjögren U, Mukohyama H, Roth C, Sundqvist G, Lerner UH. Bone-resorbing activity from cholesterol-exposed macrophages due to enhanced expression of interleukin-1alpha. J Dent Res 2002; 81(1):11-6. doi: 10.1177/002203450208100104 [Crossref] [ Google Scholar]
- Yashima M, Ogura N, Abiko Y. Studies on cholesterol accumulation in radicular cyst fluid--origin of heat-stable cholesterol-binding protein. Int J Biochem 1990; 22(2):165-9. doi: 10.1016/0020-711x(90)90179-7 [Crossref] [ Google Scholar]
- Yamazaki M, Cheng J, Hao N, Takagi R, Jimi S, Itabe H. Basement membrane-type heparan sulfate proteoglycan (perlecan) and low-density lipoprotein (LDL) are co-localized in granulation tissues: a possible pathogenesis of cholesterol granulomas in jaw cysts. J Oral Pathol Med 2004; 33(3):177-84. doi: 10.1111/j.0904-2512.2004.00087.x [Crossref] [ Google Scholar]
- Kamboj M, Devi A, Gupta S. Cholesterol granuloma in odontogenic cyst: an enigmatic lesion. Case Rep Dent 2016; 2016:6105142. doi: 10.1155/2016/6105142 [Crossref] [ Google Scholar]
- Rajesh E, Masthan KMK, Aravindha Babu N, Balachander N, Anitha N, Jayasri Krupaa R. Association of cholesterol crystals in odontogenic cysts: a histological review. Res J Pharm Biol Chem Sci 2014; 5(2):1334-9. [ Google Scholar]
- Petersen J, Glaßl EM, Nasseri P, Crismani A, Luger AK, Schoenherr E. The association of chronic apical periodontitis and endodontic therapy with atherosclerosis. Clin Oral Investig 2014; 18(7):1813-23. doi: 10.1007/s00784-013-1156-3 [Crossref] [ Google Scholar]
- Grebe A, Latz E. Cholesterol crystals and inflammation. Curr Rheumatol Rep 2013; 15(3):313. doi: 10.1007/s11926-012-0313-z [Crossref] [ Google Scholar]
- Mitchel R. Blood vessels. In: Kumar V, Abbas AK, Aster JC, eds. Robbins & Cotran Pathologic Basis of Disease. 9th ed. Philadelphia: Elsevier Saunders; 2015. p. 483-522.
- Alghofaily M, Tordik P, Romberg E, Martinho F, Fouad AF. Healing of apical periodontitis after nonsurgical root canal treatment: the role of statin intake. J Endod 2018; 44(9):1355-60. doi: 10.1016/j.joen.2018.06.013 [Crossref] [ Google Scholar]