Avicenna J Dent Res. 13(3):109-112.
doi: 10.34172/ajdr.2021.21
Case Report
Drug-Induced Gingival Overgrowth in an 8-Year-Old Girl: A Case Report
Parviz Torkzaban 1  , Amir Talaie 2, *
, Amir Talaie 2, * 
Author information:
1Professor, Department of Periodontics, Hamedan University of Medical Sciences, School of Dentistry, Hamedan, Iran.
2Postgraduate Student, Department of Periodontics, Hamedan University of Medical Sciences, School of Dentistry, Hamedan, Iran.
Abstract
Systemic lupus erythematosus is a systemic autoimmune disease that involves multi organs. Genetic, endocrine, immunological, and environmental factors influence the loss of immunological tolerance against self-antigens leading to the formation of pathogenic autoantibodies that cause tissue damage through multiple mechanisms. The gingival overgrowth can be caused by three factors: noninflammatory, hyperplastic reaction to the medication; chronic inflammatory hyperplasia; or a combined enlargement due to chronic inflammation and drug-induced hyperplasia. Drug-Induced Gingival Overgrowth is associated with the use of three major classes of drugs, namely anticonvulsants, calcium channel blockers, and immunosuppressants. Due to recent indications for these drugs, their use continues to grow.
Keywords: Systemic lupus erythematosus, Drug-Induced gingival overgrowth, Cyclosporine, Amlodipine
Copyright and License Information
© 2021 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Torkzaban P, Talaie A. Drug-Induced Gingival Overgrowth in an 8-year-old girl: a case report. Avicenna J Dent Res. 2021;13(3):109-112. doi: 10.34172/ajdr.2021.21.
Background
Highlights
-
Drug-Induced Gingival overgrowth is associated with the use of immunosuppressants, CCBs, and anticonvulsants.
-
Drug-Induced Gingival overgrowth can be improved by removal of local factors, plaque control, and supportive periodontal therapy.
Systemic lupus erythematosus (SLE) is a severe chronic disease with a 10:1 predilection for women compared with men. SLE can affect the kidneys, heart, skin, and mucosa (1). Environmental triggers, genetic tendency and the hormonal factors interact in disease progression and activity. Clinical manifestations and the pattern of organ involvement of disease are heterogenous, and reflect the disrupted molecular pathways which manifest as SLE clinical signs and symptoms. The SLE complex pathogenesis affects multiple cellular components of the immune systems, presence of autoantibodies and immunocomplexes, involvement of the complement system and dysregulation of some of cytokines including interferon-1. Morbidity and mortality in SLE are the results of direct immune-mediated tissue damage, as well as treatment-associated complications such as accelerated coronary artery disease and increased risk of infection (2).
Gingival overgrowth (GO) has been defined as a diffused or local pathological growth of marginal gingiva, interdental papilla and/or attached gingiva. The etiopathogenetic mechanisms may derive from hereditary or idiopathic conditions, pregnancy, inflammatory conditions, vitamin C deficiency, Wegner’s granulomatosis, and leukemia or drugs (3,4). Drug induced gingival overgrowth (DIGO) is an adverse side-effect, which may occur after the administration of some systemic drugs whose target organ is not the gum (5); and it may manifest itself as a result of chronic regime of three classes of medications: immunosuppressants, calcium channel blockers (CCBs) and anticonvulsants (6-10).
CCBs are a main class of medications commonly used to treat angina pectoris, hypertension, cardiac arrhythmia, and coronary artery spasm (11). Phenylalkylamine derivatives (e.g., verapamil), Benzothiazepine derivatives (e.g., diltiazem) and dihydropyridines (e.g.,amlodipine, felodipine) are various types of CCBs that have been found to relate to DIGO (8,12-15).
Cyclosporin A has been the immunosuppressant of choice for preventing rejection of solid organ and bone marrow transplants and for treating autoimmune conditions (11).
The present study aimed to report a case where treatment of SLE by cyclosporin A and amlodipine caused GO and to introduce a method of resolving this problem.
Case Presentation
Our patient was an 8-year-old girl who was complaining from gingival enlargement. Her parents gave a history of slowly progressing enlargements on her gums, started from 9 months earlier. They were extremely worried about the appearance of their daughter in comparison to her classmates.
On intraoral examination, Grade II to Grade III GO was observed in the anterior sextants of maxilla and mandible, which was pink, diffuse, firm and nodular (Figure 1). There was no intrabony pathology associated with the soft tissue lesion in the panoramic view of the patient (Figure 2). Patient had poor oral hygiene and habit of irregular brushing. There was dental caries in deciduous molar teeth and permanent first molars. The teeth had no increased mobility.
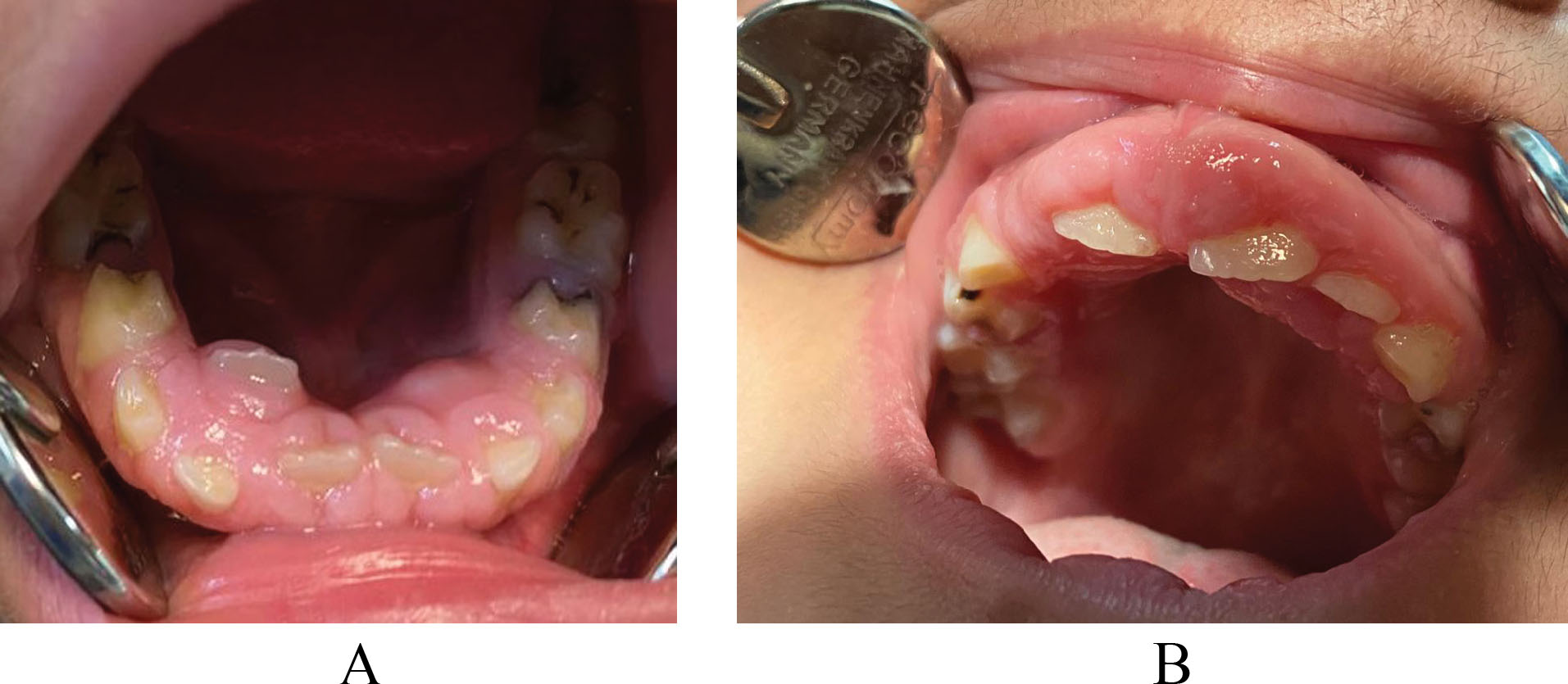
Figure 1.
Drug Induced Gingival Overgrowth (A) Mandibular (B) Maxillary.
.
Drug Induced Gingival Overgrowth (A) Mandibular (B) Maxillary.
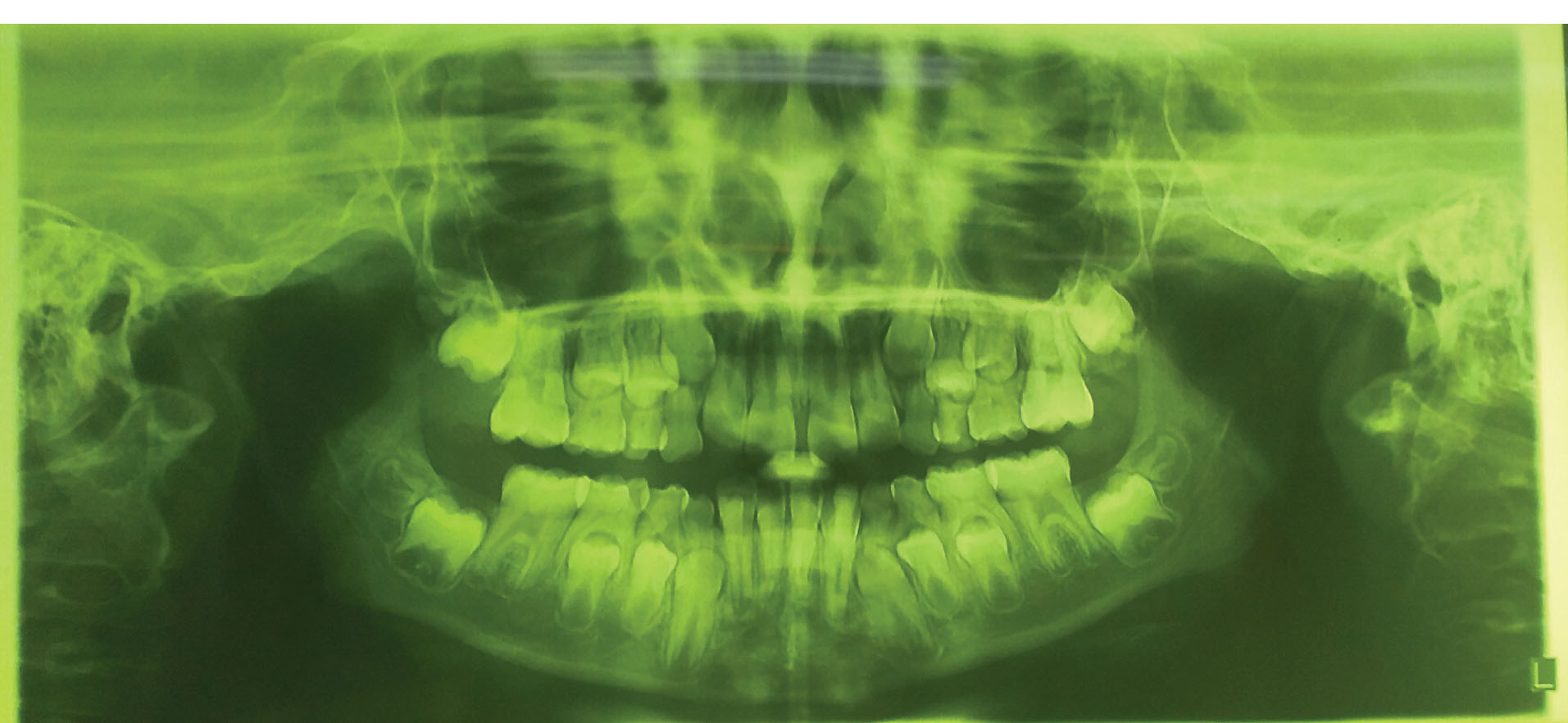
Figure 2.
Panoramic View showed no intrabony pathology associated with the soft tissue lesion.
.
Panoramic View showed no intrabony pathology associated with the soft tissue lesion.
The patient had a history of SLE, 12 months hospitalization because of proteinuria (3+) and surgery for pulmonary edema. Her mother had a history of SLE with symptoms including severe fatigue, joint pain, and butterfly rashes.
Blood and urine tests showed that SLE was under control. Medication history of the patient showed the usage of this drugs since last two years:
Tab. Prednisolone 5 mg daily;
Syrup. Sandimmun (Cyclosporine) 0.4 cc twice a day;
Tab. Hydroxychloroquine 200 mg/d;
Tab. Captopril 25 mg/d;
Tab. Losartan 25 mg/d;
Tab. Amlodipine 5 mg twice a day;
E.C.Tab. Acetylsalicylic acid 80 mg/d;
Tab. Calcium 500 mg/d.
The diagnosis of DIGO was established based on medical and drugs history, clinical examinations, and radiographic evaluations.
Treatment Done
Patient received standard oral hygiene instructions at the first session. The instructions included inter-dental plaque control, toothbrushing, and brushing of the tongue dorsum twice a day.
Patient was referred to physician for substitution of sandimmune and amlodipine with other medications or modulation of their dosage. She was asked to use Vi-one Junior Mouthwash on a weekly base for 1 minute for maintaining good plaque control and preventing tooth decay. Then she was asked to revist periodontist after two weeks.
Discussion
GO shows major difficulties for the maintenance of oral hygiene (16). Regardless of its etiology, GO could be problematic and result in an increased risk of poor oral health including periodontal disease and dental decay (17). It can lead to adverse aesthetic changes and clinical signs and symptoms such as bleeding, tenderness, pain, abnormal tooth movement, speech disturbances, and dental occlusion problems (18).
This paper aimed to report a case of cyclosporine and amlodipine-induced gingival enlargement in an 8-year-old girl who took cyclosporine at a dose of 0.4 cc twice a day, and amlodipine at a dose of 5 mg twice a day.
The incidence of amlodipine-induced GO is very low, whereas nifedipine may lead to GO in 20%-83% of the patients. The prevalence of amlodipine-induced GO has been reported to be 1.7%-3.3% (19-21).
The prevalence of cyclosporine A–induced GO has been found to be about 30% but it can be much higher, especially for pediatric populations (22). The first case of cyclosporin A–induced GO was reported in 1983 (23). Severity of the lesions can be similar to phenytoin and nifedipine induced GO. They affect the entire dentition and interfere with speech, mastication, and occlusion (24).
CCBs interfere with calcium metabolism and reduce calcium levels in gingival fibroblasts and T cells. They affect T-cell activation or proliferation and collagen biosynthesis (25-27). Cyclosporin A directly damages collagen synthesis by gingival fibroblasts (28), with an accompanying increase in the levels of type I collagen (29). Furthermore, cyclosporin A reduces expression of matrix metalloproteinase-1 (MMP-1) and MMP-3 (30).
Cyclosporin A stimulates the production of reactive oxygen species (ROS). This is the cause of cyclosporin A-induced GO which is improved by using antioxidants, comprising vitamin E and sulforaphane. In addition, the immunosuppressive effect of cyclosporin A is not hampered by antioxidant remedies (31).
Azithromycin has remarkable effects on the depletion of cyclosporine A-induced GO and bleeding on probing and, therefore, is a helpful substitute or supplement to surgical therapy (32,33).
The most effective treatment of DIGO is substitution or withdrawal of the drugs. A case report showed resolution of gingival lesions in one to eight weeks after discontinuing the medication (34). For example, changing nifedipine to another antihypertensive drug – isradipine, caused relapse of gingival overgrowth (35). Moreover, tacrolimus – used as an alternative for cyclosporine A – resulted in regression of gingival enlargement (36). As for patients taking medications associated with GO, a 3-month interval has been recommended for receiving periodontal maintenance therapy (21).
Conclusions
GO presents a clinical challenge by disrupting oral function and subsequent poor oral health. It is the result of inflammatory conditions, systemic conditions like pregnancy, puberty, vitamin C deficiency, systemic diseases including leukemia, sarcoidosis, Wegner’s granulomatosis, and some medications. If GO is left untreated, it can cause bleeding, ulceration, abscess, infection, or problems in mastication.
DIGO is associated with the use of three groups of medications, namely immunosuppressants, CCBs, and anticonvulsants. The pathogenesis of DIGO is complex and the main mechanism is mediated through defective function of gingival fibroblasts.
DIGO cannot be precluded by conventional approaches, but it can be improved by removal of local factors, plaque control, and supportive periodontal therapy on regular base. Patients should be provided with oral hygiene instructions, and periodontal prophylaxis and scaling and root planning (SRP) should be performed when required during recall visits.
Conflict of Interest Disclosures
The authors declare that they have no conflict of interests.
Ethical Statement
The authors published photos of the patient after obtaining her parents’ consent.
Authors’ Contribution
PT supervised the research. PT and AT wrote the paper.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- D’Cruz DP, Khamashta MA, Hughes GR. Systemic lupus erythematosus. Lancet 2007; 369(9561):587-96. doi: 10.1016/s0140-6736(07)60279-7 [Crossref] [ Google Scholar]
- Fava A, Petri M. Systemic lupus erythematosus: diagnosis and clinical management. J Autoimmun 2019; 96:1-13. doi: 10.1016/j.jaut.2018.11.001 [Crossref] [ Google Scholar]
- Gawron K, Łazarz-Bartyzel K, Potempa J, Chomyszyn-Gajewska M. Gingival fibromatosis: clinical, molecular and therapeutic issues. Orphanet J Rare Dis 2016; 11:9. doi: 10.1186/s13023-016-0395-1 [Crossref] [ Google Scholar]
- Tomar LR, Aggarwal A. Missing diagnosis: gingival hypertrophy due to amlodipine. Indian Heart J 2015; 67(5):491-2. doi: 10.1016/j.ihj.2015.06.011 [Crossref] [ Google Scholar]
- Tungare S, Paranjpe AG. Drug induced gingival overgrowth. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2021.
- Aimetti M, Romano F, Debernardi C. Effectiveness of periodontal therapy on the severity of cyclosporin A-induced gingival overgrowth. J Clin Periodontol 2005; 32(8):846-50. doi: 10.1111/j.1600-051X.2005.00774.x [Crossref] [ Google Scholar]
- Kose KN, Yilmaz S, Noyan U, Kuru B, Yildirim HS, Agrali OB. The gingival crevicular fluid levels of growth factors in patients with amlodipine-induced gingival overgrowth: a pilot study. Niger J Clin Pract 2020; 23(4):561-7. doi: 10.4103/njcp.njcp_532_19 [Crossref] [ Google Scholar]
- Morikawa S, Nasu M, Miyashita Y, Nakagawa T. Treatment of calcium channel blocker-induced gingival overgrowth without modifying medication. BMJ Case Rep 2021; 14(1):e238872. doi: 10.1136/bcr-2020-238872 [Crossref] [ Google Scholar]
- Morisaki I, Fukui N, Fujimori Y, Murakami J, Daikoku H, Amano A. Effects of combined oral treatments with cyclosporine A and nifedipine or diltiazem on drug-induced gingival overgrowth in rats. J Periodontol 2000; 71(3):438-43. doi: 10.1902/jop.2000.71.3.438 [Crossref] [ Google Scholar]
- Pundir AJ, Pundir S, Yeltiwar RK, Farista S, Gopinath V, Srinivas TS. Treatment of drug-induced gingival overgrowth by full-mouth disinfection: a non-surgical approach. J Indian Soc Periodontol 2014; 18(3):311-5. doi: 10.4103/0972-124x.134567 [Crossref] [ Google Scholar]
- Marshall RI, Bartold PM. A clinical review of drug-induced gingival overgrowths. Aust Dent J 1999; 44(4):219-32. doi: 10.1111/j.1834-7819.1999.tb00224.x [Crossref] [ Google Scholar]
- Yolcu A, Aydogdu I. Amlodipine-induced gingival hypertrophy. Eur J Intern Med 2020; 78:127-8. doi: 10.1016/j.ejim.2020.06.023 [Crossref] [ Google Scholar]
- Lauritano D, Martinelli M, Baj A, Beltramini G, Candotto V, Ruggiero F. Drug-induced gingival hyperplasia: an in vitro study using amlodipine and human gingival fibroblasts. Int J Immunopathol Pharmacol 2019; 33:2058738419827746. doi: 10.1177/2058738419827746 [Crossref] [ Google Scholar]
- Bullon P, Machuca G, Martinez Sahuquillo A, Rojas J, Lacalle JR, Rios JV. Clinical assessment of gingival size among patients treated with diltiazem. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995; 79(3):300-4. doi: 10.1016/s1079-2104(05)80223-9 [Crossref] [ Google Scholar]
- Matharu MS, van Vliet JA, Ferrari MD, Goadsby PJ. Verapamil induced gingival enlargement in cluster headache. J Neurol Neurosurg Psychiatry 2005; 76(1):124-7. doi: 10.1136/jnnp.2003.024240 [Crossref] [ Google Scholar]
- Trackman PC, Kantarci A. Molecular and clinical aspects of drug-induced gingival overgrowth. J Dent Res 2015; 94(4):540-6. doi: 10.1177/0022034515571265 [Crossref] [ Google Scholar]
- Nivethitha K, Ramesh A, Talwar A, Shenoy N. Rare phenomena of tacrolimus-induced gingival hyperplasia. J Oral Maxillofac Pathol 2020; 24(2):403. doi: 10.4103/jomfp.JOMFP_50_20 [Crossref] [ Google Scholar]
- Dongari-Bagtzoglou A. Drug-associated gingival enlargement. J Periodontol 2004; 75(10):1424-31. doi: 10.1902/jop.2004.75.10.1424 [Crossref] [ Google Scholar]
- Gopal S, Joseph R, Santhosh VC, Kumar VV, Joseph S, Shete AR. Prevalence of gingival overgrowth induced by antihypertensive drugs: a hospital-based study. J Indian Soc Periodontol 2015; 19(3):308-11. doi: 10.4103/0972-124x.153483 [Crossref] [ Google Scholar]
- Irokawa D, Fujita T, Yamamoto S, Masuda H, Saito A. A case report of chronic periodontitis with gingival overgrowth induced by cyclosporine A and cilnidipine. Nihon Shishubyo Gakkai Kaishi 2014; 56(1):72-81. doi: 10.2329/perio.56.72 [Crossref] [ Google Scholar]
- Ellis JS, Seymour RA, Steele JG, Robertson P, Butler TJ, Thomason JM. Prevalence of gingival overgrowth induced by calcium channel blockers: a community-based study. J Periodontol 1999; 70(1):63-7. doi: 10.1902/jop.1999.70.1.63 [Crossref] [ Google Scholar]
- Kilpatrick NM, Weintraub RG, Lucas JO, Shipp A, Byrt T, Wilkinson JL. Gingival overgrowth in pediatric heart and heart-lung transplant recipients. J Heart Lung Transplant 1997; 16(12):1231-7. [ Google Scholar]
- Rateitschak-Plüss EM, Hefti A, Lörtscher R, Thiel G. Initial observation that cyclosporin-A induces gingival enlargement in man. J Clin Periodontol 1983; 10(3):237-46. doi: 10.1111/j.1600-051x.1983.tb01272.x [Crossref] [ Google Scholar]
- Friskopp J, Klintmalm G. Gingival enlargement A comparison between cyclosporine and azathioprine treated renal allograft recipients. Swed Dent J 1986; 10(3):85-92. [ Google Scholar]
- Barclay S, Thomason JM, Idle JR, Seymour RA. The incidence and severity of nifedipine-induced gingival overgrowth. J Clin Periodontol 1992; 19(5):311-4. doi: 10.1111/j.1600-051x.1992.tb00650.x [Crossref] [ Google Scholar]
- Tipton DA, Fry HR, Dabbous MK. Altered collagen metabolism in nifedipine-induced gingival overgrowth. J Periodontal Res 1994; 29(6):401-9. doi: 10.1111/j.1600-0765.1994.tb01241.x [Crossref] [ Google Scholar]
- Gopinath S, Harishkumar VV, Santhosh VC, Puthalath S. Case report on low dose of cilnidipine: a fourth-generation calcium channel blocker-induced gingival overgrowth. J Indian Soc Periodontol 2019; 23(4):377-80. doi: 10.4103/jisp.jisp_557_18 [Crossref] [ Google Scholar]
- Mariotti A, Hassell T, Jacobs D, Manning CJ, Hefti AF. Cyclosporin A and hydroxycyclosporine (M-17) affect the secretory phenotype of human gingival fibroblasts. J Oral Pathol Med 1998; 27(6):260-6. doi: 10.1111/j.1600-0714.1998.tb01953.x [Crossref] [ Google Scholar]
- Schincaglia GP, Forniti F, Cavallini R, Piva R, Calura G, del Senno L. Cyclosporin-A increases type I procollagen production and mRNA level in human gingival fibroblasts in vitro. J Oral Pathol Med 1992; 21(4):181-5. doi: 10.1111/j.1600-0714.1992.tb00098.x [Crossref] [ Google Scholar]
- Bolzani G, Della Coletta R, Martelli Júnior H, Martelli Júnior H, Graner E. Cyclosporin A inhibits production and activity of matrix metalloproteinases by gingival fibroblasts. J Periodontal Res 2000; 35(1):51-8. doi: 10.1034/j.1600-0765.2000.035001051.x [Crossref] [ Google Scholar]
- Chin YT, Tu HP, Lin CY, Kuo PJ, Chiu HC, Liu SH. Antioxidants protect against gingival overgrowth induced by cyclosporine A. J Periodontal Res 2021; 56(2):397-407. doi: 10.1111/jre.12832 [Crossref] [ Google Scholar]
- Teshome A, Girma B, Aniley Z. The efficacy of azithromycin on cyclosporine-induced gingival enlargement: systematic review and meta-analysis. J Oral Biol Craniofac Res 2020; 10(2):214-9. doi: 10.1016/j.jobcr.2019.12.005 [Crossref] [ Google Scholar]
- Kumar SS, Mohammad H, Kar K. Management of cyclosporine-influenced gingival enlargement with azithromycin. Clin Adv Periodontics 2020; 10(3):140-4. doi: 10.1002/cap.10097 [Crossref] [ Google Scholar]
- Khocht A, Schneider LC. Periodontal management of gingival overgrowth in the heart transplant patient: a case report. J Periodontol 1997; 68(11):1140-6. doi: 10.1902/jop.1997.68.11.1140 [Crossref] [ Google Scholar]
- Westbrook P, Bednarczyk EM, Carlson M, Sheehan H, Bissada NF. Regression of nifedipine-induced gingival hyperplasia following switch to a same class calcium channel blocker, isradipine. J Periodontol 1997; 68(7):645-50. doi: 10.1902/jop.1997.68.7.645 [Crossref] [ Google Scholar]
- James JA, Boomer S, Maxwell AP, Hull PS, Short CD, Campbell BA. Reduction in gingival overgrowth associated with conversion from cyclosporin A to tacrolimus. J Clin Periodontol 2000; 27(2):144-8. doi: 10.1034/j.1600-051x.2000.027002144.x [Crossref] [ Google Scholar]