Avicenna J Dent Res. 13(4):113-118.
doi: 10.34172/ajdr.2021.22
Original Article
Effect of Different Bleaching Methods on Optical Behaviors of CAD/CAM Ceramics
Saeed Nikanjam 1  , Samaneh Abbasi 1, Sara Khazaei 1, *
, Samaneh Abbasi 1, Sara Khazaei 1, * 
Author information:
1Assistant Professor, Department of Prosthodontics, Faculty of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran.
Abstract
Background: The present study aimed to survey the influence of two different bleaching techniques on changes of color, translucency, and whiteness of the four CAD/CAM materials.
Methods: The monolithic blocks of Vita Suprinity, Vita Enamic, IPS e.max CAD, and Katana Zirconia were sectioned to discs with thickness of 2 mm (n=30 / each group). Samples from each type of ceramic were assigned to three subgroups: 1) the 40% hydrogen peroxide for 20 minutes; 2) the 16% carbamide peroxide for three hours/day for 2 weeks; and 3) the control. Then CIELab coordinates of each sample were evaluated before and after the intervention by a spectrophotometer. Final color change (ΔE), Whiteness (ΔWI D), and Translucency Parameter (ΔTP) were calculated. Two-way ANOVA test was adopted to analyze the data (α=0.05).
Results: Type of ceramic, bleaching subgroups, and interaction between them had a statistically significant influence on mean values of ΔE, ΔWID. The influence of bleaching subgroup on the mean value of ΔTP was also significant (P<0.001).
Conclusions: Carbamide peroxide 16% for three hours/day and for two weeks caused the most considerable changes in final color, whiteness, and translucency of the all tested CAD/CAM materials. Maximum color change and whiteness were detected in the Vita Enamic, which were clinically unacceptable.
Keywords: Optical behaviors, Bleaching, CAD/CAM ceramics, Spectrophotometry, Vita Suprinity, Vita Enamic, IPS e.max CAD, Katana Zirconia
Copyright and License Information
© 2021 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Nikanjam S, Abbasi S, Khazaei S. Effect of different bleaching methods on optical behaviors of CAD/CAM ceramics. Avicenna J Dent Res. 2021;13(4):113-118. doi: 10.34172/ajdr.2021.22.
Background
Highlights
-
Maximum color change and whiteness were detected in Vita Enamic, which was clinically unacceptable
-
Carbamide peroide 16% for 3 hours/ day for 14 days led to the most enormous changes in final color, whiteness and translucency of all tested CAD/CAM materials.
Esthetics has become the most crucial demand of dentistry patients recently. Esthetic restoration is expected to be an accurate replica of the natural tooth (1). All-ceramic restorations are widely used in esthetic regions due to their better optical behaviors than PFM restorations (2). Conventional methods or CAD/CAM technology can also be adopted in the fabrication of all-ceramic restorations (3). The development in CAD/CAM technology has substantially increased the fabrication of different types of ceramic restorations such as inlay, onlay, veneer, and crown (4). Moreover, monolithic CAD/CAM blocks have increased fracture resistance, homogenous structure, and negligible construction defects (5,6). There are great varieties of dental ceramics available for fabricating fixed prostheses using CAD/CAM technology. Some of the new generations of machinable ceramic materials include lithium disilicate, zirconium dioxide, Zirconia-reinforced Lithium Silicate, and polymer-infiltrated ceramic network (7).
Lithium disilicate-reinforced glass ceramics have different beneficial properties including excellent mechanical properties, translucency, and acid sensitivity (8). Monolithic zirconia restorations have shown outstanding strength, esthetics (e.g., colored by dipping in special colorants), low enamel abrasiveness, and less tooth reduction (7). Zirconia-reinforced Lithium Silicate (ZLS) ceramics have been presented as a type of material for the CAD/CAM technology with 10% zirconia weight, which has better mechanical properties compared to the lithium disilicate (4,9).
Polymer-infiltrated ceramic network materials have a dual network structure and outstanding features including reasonable brittleness index, lower hardness, and similar creep response to enamel are visible (7).
Today, bleaching agents are extensively used to eliminate different stains and produce ideal esthetic effects (10). The bleaching techniques are classified differently based on the vitality of the teeth and concentration of the bleaching material (11). A clinician may use in-office bleaching, a high concentration of the hydrogen peroxide (HP), or carbamide peroxide (CP) for 15 to 60 minutes. In an at-home bleaching, the patient may receive the lower concentration of CP or HP for one to four week(s) (8). HP and CP act as active components that are diffused to the spaces between enamel rods and dentinal tubules to oxidize stain particles (10). During this standard esthetic treatment, pre-existing restoration can be affected by the active components. Therefore, the optical properties of the restorative materials in esthetic regions can be changed because they may not be safe for restorative materials, despite the safety of these materials for the hard dental structure (12,13).
The color change can be quantified by measuring Commission Internationale de l’éclairage (CIE) L*a*b* values with a spectrophotometer. In the CIELab system, L* is proportional to value in the Munsell system; a* and b* do not correspond directly to Munsell’s Hue and Chroma (7).However, a * and b* are named “chromaticity coordinates” (14). Based on ΔE value and then comparing with a perceptional threshold of the human eye, even a slight color change was ascertained (15). According to the findings from a study by Della Bona (16), translucency attributes of a substance can be determined by contrast ratio (CR) and translucency parameter (TP). In addition, a new whiteness index (WID) developed especially for dentistry is handy for measuring whiteness efficacy (17).
There is extensive literature about the evaluation of the influence of the whitening agents on different esthetic restorations, including ceramics and composite materials (8,10,18,19). However, there are not sufficient scientific data about the influence of in-office and at-home bleaching on the lithium disilicate, zirconium dioxide, zirconia-reinforced lithium silicate, and polymer-infiltrated ceramic network. This study, therefore, aimed to investigate the influence of two different bleaching techniques on changes of color, translucency, and whiteness of the mentioned CAD/CAM material. The null hypothesis was that bleaching agents would not change the color, translucency, and whiteness of lithium disilicate, zirconium dioxide, zirconia-reinforced lithium silicate, and polymer-infiltrated ceramic network.
Materials and Methods
In this experimental study, four different CAD/CAM monolithic materials with A2 shade (high translucent) were evaluated. The given materials included: 1) Lithium disilicate-reinforced glass ceramic, IPS e.max CAD (Ivoclar Vivadent, AG, Schaan, Liechtenstein); 2) Zirconia dioxide material, Katana system (Noritake Dental Supply Co., Ltd., Miyoshi, Japan); 3) Zirconia-reinforced lithium silicate, Vita Suprinity (VITA Zahnfabrik, DeguDent, Germany); and 4) polymer-infiltrated ceramic network, Vita Enamic (Vita Zahnfabrik, Bad Säckingen, Germany). The characteristics of the four CAD/ CAM ceramics tested in this study are shown in Table 1.
Table 1.
The Material Tested in This Research
|
Brand Name
|
Type
|
Shade
|
Composition
|
Manufacture
|
| IPS e.max CAD |
Lithium disilicate-reinforced glass-ceramic |
A2, HT |
SiO2, LiO2, K2O, P2O5, ZrO2, ZnO, AL2O3, MgO, Pigments |
Ivoclar Vivadent, AG, Schaan, Liechtenstein |
| Katana Zirconia |
Zirconia ceramic |
A2, HT |
ZrO2, Y2O3 |
Noritake Dental Supply Co., Ltd., Miyoshi, Japan |
| Vita Suprinity |
Zirconia-reinforced Lithium Silicate |
A2, HT |
SiO2, Li2O, K2O, P2O5, Al2O3, ZrO2, CeO2, pigments |
VITA Zahnfabrik, DeguDent, Germany |
| Vita Enamic |
Polymer-infiltrated ceramic network |
A2, HT |
SiO2, AL2O3, Na2O, K2O, B2O3, CaO, TiO2, TEG-DMA, UDMA |
Vita Zahnfabrik, Bad Säckingen, Germany |
Taking into account the findings from recent studies with 80% power and.05 level of significance, 10 specimens were assigned to each subgroup (N = 120) in the present study. Monolithic blocks were sectioned to discs with thickness of 2.0 mm, using a cutting machine (CUTLAM®micro 2.0, France) with a diamond saw (series 15LCU, BUEHLER) under a constant water flow. The discs were for simulating monolithic restorations. The samples were purified in an ultrasonic cleaner (EURONDA, Vicenza, Italy) containing distilled water for 20 minutes according to the manufacturer’s instructions. All samples of IPS e.max CAD, Katana Zirconia, and Vita Suprinity were sintered according to the manufacturer’s instructions. Then all samples were adjusted by using 1200 grit SiC paper under running water to establish the predesignated thicknesses ( ± 0.02 mm). Those samples with any defects, including thickness and structure, were removed from the investigation.
There were four CAD/CAM ceramic groups each of which was divided into three subgroups. Samples of each CAD/CAM ceramic material were randomly assigned to three subgroups as follows: 1) samples were treated under Opalescence Boost (Ultradent Products Inc., South Jordan, UT, USA) with 40% HP according to the manufacturer’s instructions, simulating in-office technique; 2) samples were treated under Whiteness Perfect (FGM, Joinville, SC, Brazil) with 16% CP according to the manufacturer’s instructions, simulating at-home technique; 3) the samples kept in distilled water were replaced every day during two weeks as control subgroup.
The CIELab coordinating (L*, a*, b*) the samples was evaluated before and after the intervention with a spectrophotometer (VITA Easyshade V; VITA Zahnfabrik) which was calibrated according to the manufacturer’s recommendations, and employed for all measurements. A putty additional silicone material (DuosilTM, SHERA Werkstoff-Technologie, Germany) was adapted to the mouthpiece of the spectrophotometer to prevent external light, stabilize the position of the ceramics, backgrounds and the spectrophotometer, and replicate the condition for all measurements. The measurements were performed using standard light source D65. Furthermore, one drop of optical liquid (Cargille Labs, Cedar Grove NJ, USA) with refraction index 1.5 was applied to the backgrounds in order for establishing optical contact. The L*, a*, and b* values of the samples were evaluated using the device in the middle of each sample.
To evaluate the color change (ΔE), a 50% gray background (20) was used under each sample to measure the CIELab coordinates. To calculate changes of the final color, the following formula was applied (21):
1) ΔE = [(L*j – L*i)2 + (a*j – a*i)2 + (b*j – b*i)2]1/2, symbol j presented CIELab coordinates after the intervention, and symbol i presented CIELab coordinates before it. Values ΔE were compared with acceptability (ΔE = 5.5) and perceptibility (ΔE = 2.6) thresholds for the perception of the amount of the samples’ final color change (22-25).
To evaluate the changes of whitening index of the samples (ΔWID), the following formulas (17) were applied:
2) ΔWID = WI Dj – WI Di
3) WI D = 0.511L* – 2.324a* –1.100b*
In this study, ΔWI D values were compared with acceptability (ΔWI D = 2.6) and perceptibility (ΔWI D = 0.7) threshold for the perception of the amount of the samples’ whitening change (26).
To evaluate translucency parameter (TP) (8), CIELab coordinates on a black and a white background were measured before and after the intervention; then to calculate ΔTP, the following formulas were used:
4) ΔTP = TP j – TP i
5) TP = [(L*B – L*W)2 + (a*B – a*W)2 + (b*B – b*W)2] 1/2, symbol B presented CIELab coordinates on the black background and symbol W presented CIELab coordinates on the white background. In the present study, ΔTP values were compared with acceptability (ΔTP = 4.43) and perceptibility (ΔTP = 1.33) threshold for the perception of the amount of the samples’ translucency change (27). The CIELab coordinates of all backgrounds are displayed in Table 2.
Table 2.
The CIELab Coordinates of all Backgrounds Are Used in This Study
|
CIELab Coordinates
|
L*
|
a*
|
b*
|
| Gray |
50.6 |
-0.2 |
-0.13 |
| Black |
1.6 |
1.2 |
-1.0 |
| White |
92.6 |
-1.2 |
2.9 |
Statistical analysis of the data was performed using SPSS software (IBM SPSS Statistics v23; IBM Corp), and the normal distribution of them was tested by Kolmogorov-Smirnov and Shapiro-Wilk tests (P>.05). Two-way ANOVA was adopted to examine the influence of ceramic type, bleaching method, and interaction of them on ΔE, ΔWI D, ΔTP values among the groups. The pairwise comparison was performed between different subgroups for the mentioned dependent variables using Bonferroni post hoc test.
Results
The average results of ΔE, ΔWID, and ΔTP values of all subgroups for all the tested ceramic materials are diagrammed in Figures 1to3. The results demonstrated that type of ceramic, bleaching subgroups, and the interaction between them had a statistically significant influence on mean values of ΔE, ΔWID. Moreover, the significant influence of bleaching subgroup on the mean value of ΔTP was confirmed (P <0.001) (Table 3).
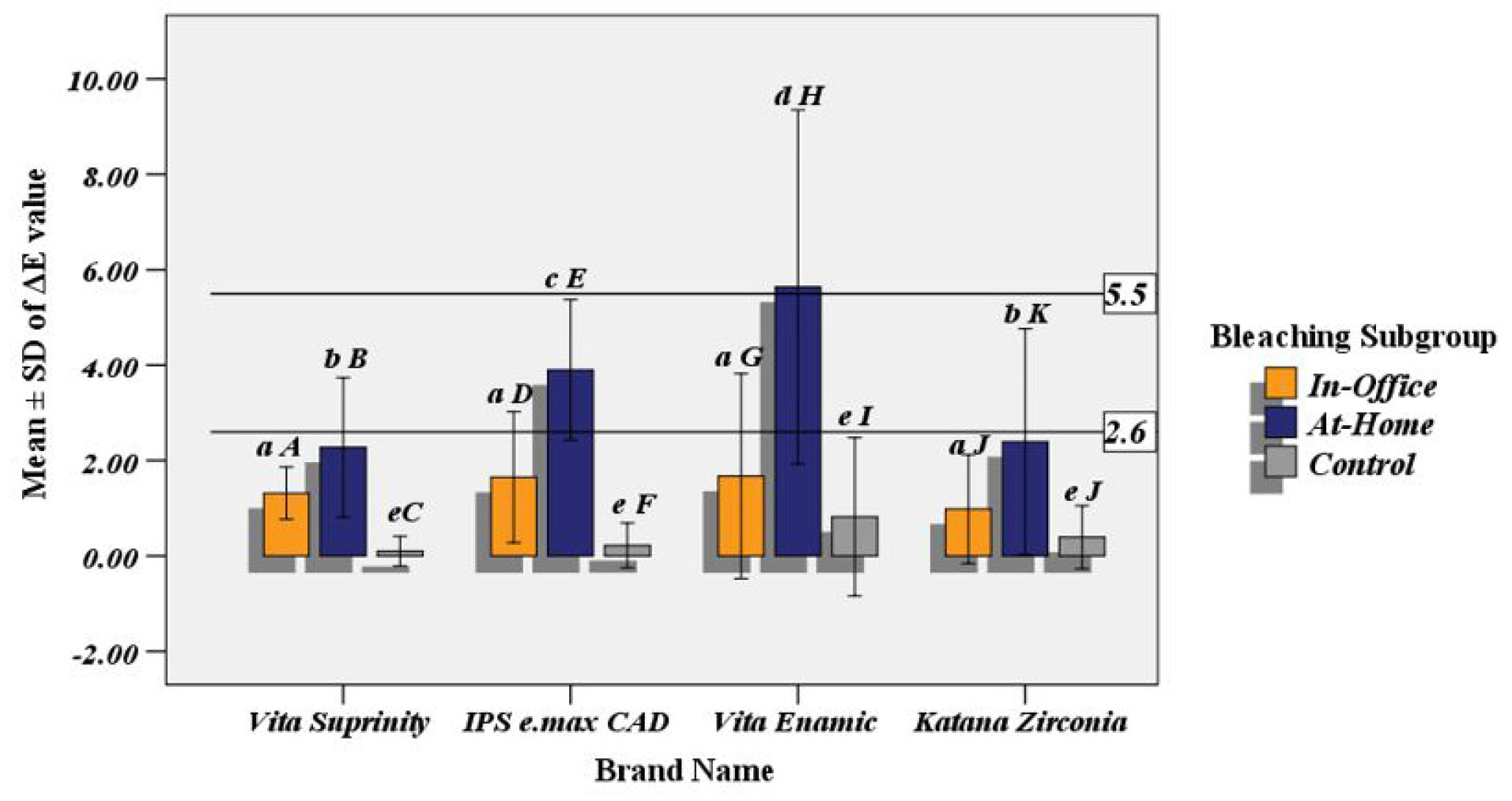
Figure 1.
Mean ± SD of ΔE value, different superscript lower case letters in a bleaching subgroup, and capital letters in a type of ceramic show statistically significant differences (P < 0.05).
.
Mean ± SD of ΔE value, different superscript lower case letters in a bleaching subgroup, and capital letters in a type of ceramic show statistically significant differences (P < 0.05).
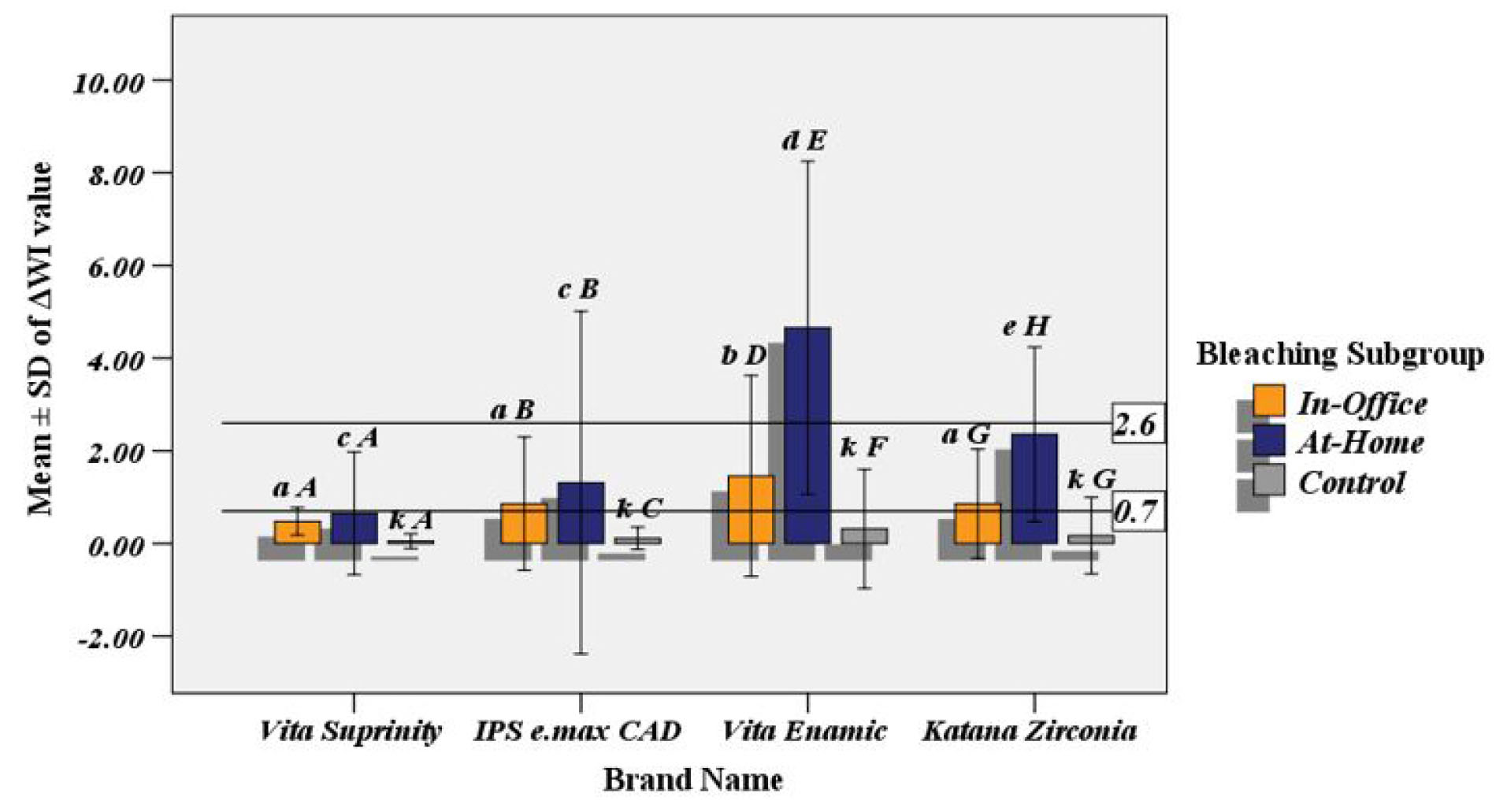
Figure 2.
Mean ± SD of ΔWID value, different superscript lower case letters in a bleaching subgroup, and capital letters in a type of ceramic show statistically significant differences (P < 0.05).
.
Mean ± SD of ΔWID value, different superscript lower case letters in a bleaching subgroup, and capital letters in a type of ceramic show statistically significant differences (P < 0.05).
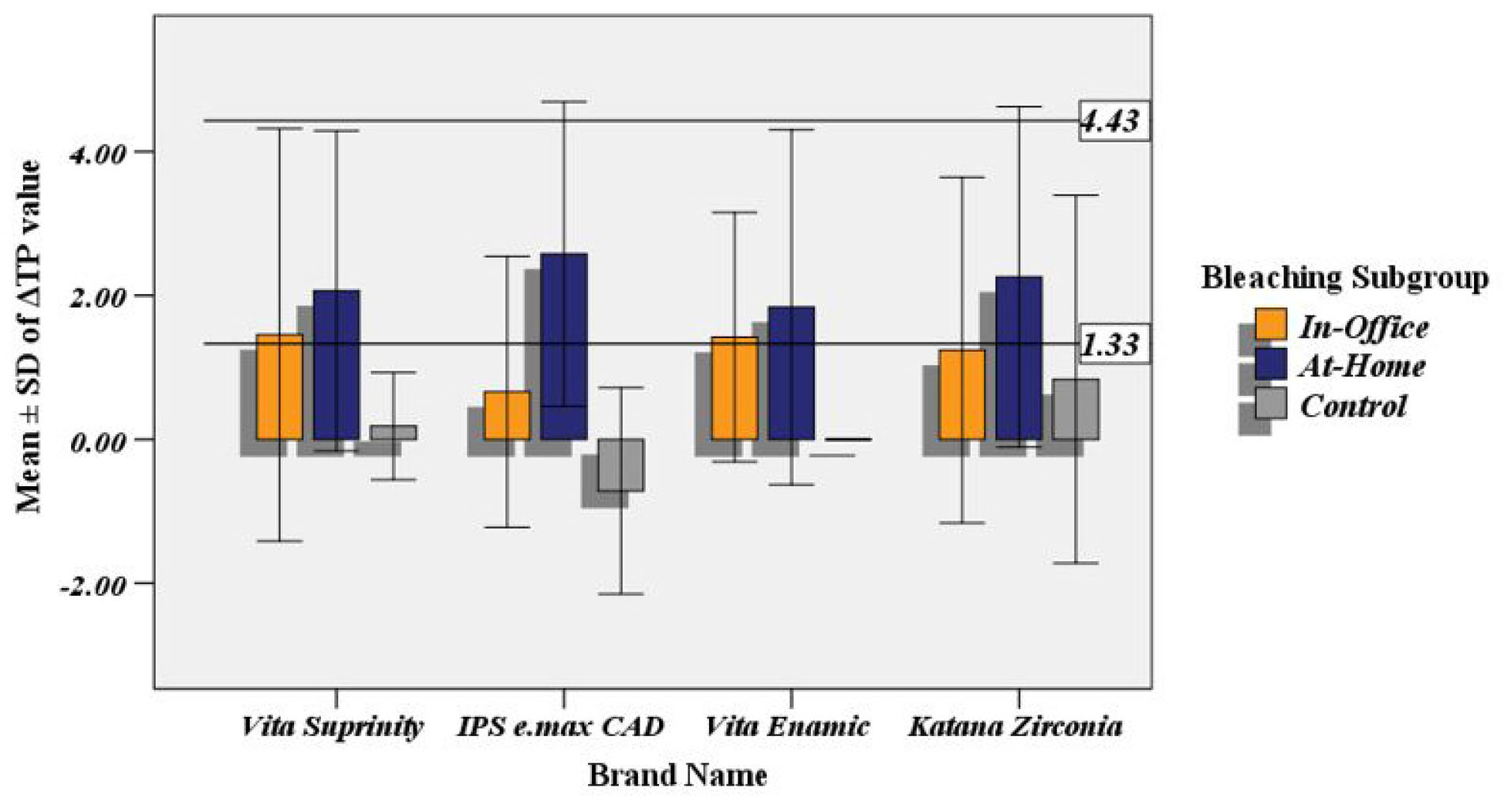
Figure 3.
Mean ± SD of ΔTP Value.
.
Mean ± SD of ΔTP Value.
Table 3.
Results of the Two-Way ANOVA Test for the Impact of the Type of Ceramic and Bleaching Subgroups on Mean ΔE, ΔWID, ΔTP Value
|
Dependent Variable
|
Fixed Factor
|
Mean Square
|
F
|
P
Value
|
|
ΔE
|
Bleaching subgroup |
104.649 |
142.375 |
<0.001 |
| Type of ceramic |
14.626 |
19.899 |
<0.001 |
| Bleaching subgroup* Type of ceramic |
6.129 |
8.338 |
<0.001 |
| Error |
0.735 |
|
|
|
ΔWI
D
|
Bleaching subgroup |
44.524 |
50.237 |
<0.001 |
| Type of ceramic |
17.032 |
19.218 |
<0.001 |
| Bleaching subgroup* Type of ceramic |
7.775 |
8.773 |
<0.001 |
| Error |
0.886 |
|
|
|
ΔTP
|
Bleaching subgroup |
44.553 |
42.093 |
<0.001 |
| Type of ceramic |
1.930 |
1.824 |
0.147 |
| Bleaching subgroup* Type of ceramic |
2.234 |
2.111 |
0.058 |
| Error |
1.058 |
|
|
Two sequences used for pairwise comparisons by Bonferroni post hoc test were as follows: 1) for each bleaching subgroup between different types of the ceramic (sequence 1, with superscript lower case letters in Figure 1 to 2) for each type of the ceramic between different bleaching subgroups (sequence 2, with superscript capital letters in Figure 1 to 2). These sequences were applied for ΔE, ΔWID because the interaction of two fixed factors was statistically significant (Figure 1 to 2).
Discussion
According to our study findings, the significant statistical differences observed in the final color and whiteness of the four tested CAD/CAM monolithic ceramic were attributed to the type of the ceramic material, bleaching subgroup, and interaction of them. Furthermore, the significant statistical difference detected in the translucency of the tested materials was related to the bleaching subgroup. Therefore, the null hypothesis for this research was rejected (Table 3).
The subjective methods (e.g., shade guide) as well as the objective ones (e.g., colorimeter, spectrophotometer, and digital image analysis) used to evaluate the optical behaviors of the esthetic restorative material in dentistry have already been detected and discussed in the literature (28,29). A 33% increase accuracy of the measurements has also been found using spectrophotometry. In this study, therefore, the changes in the final color, whitening, and translucency were evaluated by a spectrophotometer (10).
Particular formulas to evaluate the final color change have been presented in the literature; however, the latest formula (ΔE00) was presented in 2001 (10). These formulas are interchangeable and a high correlation among them has been reported (30,31). In this study, therefore, ΔE equation was applied for color measurement (32-34).
The ΔE equation is a sum of L*, a*, and b changes squares; and thus it always generates a positive result (18). For addressing this problem and determining the direction of the whiteness change, WID was used in the present study (17). Positive and negative results of ΔWID were interpreted as the effects of bleaching. Therefore, positive results indicated the positive effect of the bleaching (18).
In this study, the optical liquid with a refraction index about 1.5 was also added to improve the accuracy of spectrophotometric evaluation by a decrease in the phenomenon known as “edge-loss” (7,35).
White background as the standard background in some studies was used to evaluate the final color change (36,37). In a recent research by Ardu et al (20), however, it was reported that gray background simulated an intra-oral environment better than a white background. Therefore, a gray background was applied in this in vitro study to evaluate CIELab coordinates and to calculate ΔE and ΔWID.
The translucency of the ceramic was related to the transmission of the light through it, which could cause following alterations in the external surface texture or the body mass of the ceramic. In some studies, translucency has been quantified by calculating the TP, which is presented as a color change of a sample over a white and black backgrounds (38). The TP value for a completely transparent material is 100, which indicates the CIELab color difference between the standard white and black backgrounds.
According to our study results presented in Figures 1 and 2, the maximum value of the color change and whiteness was found in the Vita Enamic ceramic when it was exposed to the 16% CP for three hours/day for two weeks (at-home bleaching). This amount of change was clinically unacceptable. However, the concentration used in the at-home bleaching technique was lower than the in-office technique (40% HP for 20 minutes). This finding was in agreement with the results from the study by Karakaya and Cengiz-Yanardag (10) where it was reported that more considerable color change was detected when the hybrid ceramic material was exposed to a bleaching agent with 16% CP.
Given these results, it seemed that the time of exposure to the bleaching agent was a far more critical factor than the concentration of the bleaching agent. Increasing duration of exposure to bleaching agent led to a greater diffusion of free radicals and then dissolution of alkaline ions of ceramic network and destruction of chemical bonds. Another three CAD/CAM ceramic materials had a clinically acceptable value of ΔE and ΔWID. The difference between the tested materials may have been attributed to the different structures (e.g., tightness of polymer chains and homogeneity of the crystals) and the depth of diffusion of bleaching agents.
According to results displayed in Figure 3, at-home bleaching subgroups of four CAD/CAM monolithic ceramics had more considerable translucency change than that found for in-office subgroups. However, the mean values of ΔTP were clinically acceptable. This finding was in line with the results from a study by Karci and Demir (8) where it was revealed that the translucency of two CAD/CAM ceramic systems significantly changed due to the bleaching with 16% CP for six hours/day for one week. However, the opalescence parameter and contrast ratio did not change.
More enormous changes of translucency due to the exposure with 16% CP for three hours/day for two weeks may have been attributed to water sorption and chemical degradation (39) as well as to changes of the refractive index of the CAD/CAM ceramic materials in this duration.
According to our study results and contrary to the expectations of the bleaching agent manufacturer, changes in the optical behaviors of the CAD/CAM restorative materials may have occurred. Therefore, the dentists were strongly recommended to be cautious while applying the bleaching treatment to the patients who had restorations with CAD/CAM ceramics.
The present study faced some limitations including the brand and shade of the tested ceramic. Therefore, it was recommended that further studies be carried out to examine the different brands and shades of CAD/CAM material.
Conclusions
Within the limitations of the present study, it was concluded that:
-
Maximum color change and whiteness were detected in the Vita Enamic, which was clinically unacceptable;
-
Vita Suprinity, IPS e.max CAD, and Katana zirconia had clinically acceptable color and whiteness changes;
-
Carbamide peroxide 16% for 3 hours/day for 14 days led to the most enormous changes in final color, whiteness, and translucency of the all tested CAD/CAM materials;
-
Dentists were highly recommended to be cautious while performing bleaching treatment to the patients having had restorations with CAD/CAM ceramics.
Conflict of Interest Disclosures
The authors declare that they have no conflict of interests.
Ethical Statement
The research Ethics committee of Hamadan University of Medical Sciences approved this study(code:IR.UMSHA.REC.1400.47)
Authors’ Contribution
SN and SA contributed in study design, data collection and data analysis, SKH contributed in result interpretation and manuscript preparation.
References
- Saad SA, Shalaby YA, Azer AS, El-Sharkawy FM. Spectrophotometer analysis of CAD-CAM zirconia reinforced lithium silicate and lithium disilicate glass ceramics. Alex Dent J 2019; 44(3):53-8. doi: 10.21608/adjalexu.2019.63558 [Crossref] [ Google Scholar]
- Shadman N, Gorji Kandi S, Farzin Ebrahimi S, Azizi Shoul M. The minimum thickness of a multilayer porcelain restoration required for masking severe tooth discoloration. Dent Res J (Isfahan) 2015; 12(6):562-8. doi: 10.4103/1735-3327.170576 [Crossref] [ Google Scholar]
- Takaba M, Tanaka S, Ishiura Y, Baba K. Implant-supported fixed dental prostheses with CAD/CAM-fabricated porcelain crown and zirconia-based framework. J Prosthodont 2013; 22(5):402-7. doi: 10.1111/jopr.12001 [Crossref] [ Google Scholar]
- Firouz F, Izadi A, Fotovat F, Ghorbani Gholiabad S, Nikanjam S. The effect of different solutions on optical behavior of polished and glazed zirconia-reinforced lithium silicate ceramics. J Kerman Univ Med Sci 2018; 25(5):428-40. [ Google Scholar]
- Liu PR, Essig ME. Panorama of dental CAD/CAM restorative systems. Compend Contin Educ Dent 2008; 29(8):482-4. [ Google Scholar]
- Li RW, Chow TW, Matinlinna JP. Ceramic dental biomaterials and CAD/CAM technology: state of the art. J Prosthodont Res 2014; 58(4):208-16. doi: 10.1016/j.jpor.2014.07.003 [Crossref] [ Google Scholar]
- Rosenstiel SF, Land MF. Contemporary Fixed Prosthodontics-E-Book. Elsevier Health Sciences; 2015. p. 624-46.
- Karci M, Demir N. Effect of home bleaching on the translucency of CAD/CAM systems. J Prosthodont 2019; 28(3):310-4. doi: 10.1111/jopr.12701 [Crossref] [ Google Scholar]
- Denry I, Kelly JR. Emerging ceramic-based materials for dentistry. J Dent Res 2014; 93(12):1235-42. doi: 10.1177/0022034514553627 [Crossref] [ Google Scholar]
- Karakaya I, Cengiz-Yanardag E. Changes in optical characteristics and surface topography of CAD/CAM materials after bleaching applications: an AFM evaluation. J Prosthodont 2020; 29(3):226-36. doi: 10.1111/jopr.13134 [Crossref] [ Google Scholar]
- Attin T, Hannig C, Wiegand A, Attin R. Effect of bleaching on restorative materials and restorations--a systematic review. Dent Mater 2004; 20(9):852-61. doi: 10.1016/j.dental.2004.04.002 [Crossref] [ Google Scholar]
- Cengiz E, Kurtulmus-Yilmaz S, Ulusoy N, Deniz ST, Yuksel-Devrim E. The effect of home bleaching agents on the surface roughness of five different composite resins: a SEM evaluation. Scanning 2016; 38(3):277-83. doi: 10.1002/sca.21307 [Crossref] [ Google Scholar]
- Hafez R, Ahmed D, Yousry M, El-Badrawy W, El-Mowafy O. Effect of in-office bleaching on color and surface roughness of composite restoratives. Eur J Dent 2010; 4(2):118-27. [ Google Scholar]
- Poggio C, Vialba L, Berardengo A, Federico R, Colombo M, Beltrami R. Color stability of new esthetic restorative materials: a spectrophotometric analysis. J Funct Biomater 2017; 8(3):26. doi: 10.3390/jfb8030026 [Crossref] [ Google Scholar]
- Vichi A, Louca C, Corciolani G, Ferrari M. Color related to ceramic and zirconia restorations: a review. Dent Mater 2011; 27(1):97-108. doi: 10.1016/j.dental.2010.10.018 [Crossref] [ Google Scholar]
- Della Bona A. Bonding to Ceramics: Scientific Evidences for Clinical Dentistry. São Paulo: Artes Médicas; 2009.
- del Mar Pérez M, Ghinea R, Rivas MJ, Yebra A, Ionescu AM, Paravina RD. Development of a customized whiteness index for dentistry based on CIELAB color space. Dent Mater 2016; 32(3):461-7. doi: 10.1016/j.dental.2015.12.008 [Crossref] [ Google Scholar]
- Culic B, Gasparik C, Varvara M, Culic C, Dragos C, Silaghi Dumitrescu LA, Dudea D. Evaluation of bleaching on CAD/CAM hybrid ceramic material. Stud Univ Babeş-Bolyai Chem 2017; 62(1):61-71. doi: 10.24193/subbchem.2017.1.05 [Crossref] [ Google Scholar]
- Della Bona A, Pecho OE, Ghinea R, Cardona JC, Paravina RD, Perez MM. Influence of bleaching and aging procedures on color and whiteness of dental composites. Oper Dent 2019; 44(6):648-58. doi: 10.2341/18-209-l [Crossref] [ Google Scholar]
- Ardu S, Braut V, Di Bella E, Lefever D. Influence of background on natural tooth colour coordinates: an in vivo evaluation. Odontology 2014; 102(2):267-71. doi: 10.1007/s10266-013-0126-1 [Crossref] [ Google Scholar]
- Alharbi A, Ardu S, Bortolotto T, Krejci I. Stain susceptibility of composite and ceramic CAD/CAM blocks versus direct resin composites with different resinous matrices. Odontology 2017; 105(2):162-9. doi: 10.1007/s10266-016-0258-1 [Crossref] [ Google Scholar]
- Choi YJ, Razzoog ME. Masking ability of zirconia with and without veneering porcelain. J Prosthodont 2013; 22(2):98-104. doi: 10.1111/j.1532-849X.2012.00915.x [Crossref] [ Google Scholar]
- Oh SH, Kim SG. Effect of abutment shade, ceramic thickness, and coping type on the final shade of zirconia all-ceramic restorations: in vitro study of color masking ability. J Adv Prosthodont 2015; 7(5):368-74. doi: 10.4047/jap.2015.7.5.368 [Crossref] [ Google Scholar]
- Douglas RD, Steinhauer TJ, Wee AG. Intraoral determination of the tolerance of dentists for perceptibility and acceptability of shade mismatch. J Prosthet Dent 2007; 97(4):200-8. doi: 10.1016/j.prosdent.2007.02.012 [Crossref] [ Google Scholar]
- Douglas RD, Steinhauer TJ, Wee AG. Intraoral determination of the tolerance of dentists for perceptibility and acceptability of shade mismatch. J Esthet Restor Dent 2009; 21(2):133-4. [ Google Scholar]
- Pérez MM, Herrera LJ, Carrillo F, Pecho OE, Dudea D, Gasparik C. Whiteness difference thresholds in dentistry. Dent Mater 2019; 35(2):292-7. doi: 10.1016/j.dental.2018.11.022 [Crossref] [ Google Scholar]
- Salas M, Lucena C, Herrera LJ, Yebra A, Della Bona A, Pérez MM. Translucency thresholds for dental materials. Dent Mater 2018; 34(8):1168-74. doi: 10.1016/j.dental.2018.05.001 [Crossref] [ Google Scholar]
- Wee AG, Lindsey DT, Kuo S, Johnston WM. Color accuracy of commercial digital cameras for use in dentistry. Dent Mater 2006; 22(6):553-9. doi: 10.1016/j.dental.2005.05.011 [Crossref] [ Google Scholar]
- Cho BH, Lim YK, Lee YK. Comparison of the color of natural teeth measured by a colorimeter and Shade Vision System. Dent Mater 2007; 23(10):1307-12. doi: 10.1016/j.dental.2006.11.008 [Crossref] [ Google Scholar]
- Lee YK. Comparison of CIELAB DeltaE* and CIEDE2000 color-differences after polymerization and thermocycling of resin composites. Dent Mater 2005; 21(7):678-82. doi: 10.1016/j.dental.2004.09.005 [Crossref] [ Google Scholar]
- Arocha MA, Basilio J, Llopis J, Di Bella E, Roig M, Ardu S. Colour stainability of indirect CAD-CAM processed composites vs conventionally laboratory processed composites after immersion in staining solutions. J Dent 2014; 42(7):831-8. doi: 10.1016/j.jdent.2014.04.002 [Crossref] [ Google Scholar]
- Samra AP, Pereira SK, Delgado LC, Borges CP. Color stability evaluation of aesthetic restorative materials. Braz Oral Res 2008; 22(3):205-10. doi: 10.1590/s1806-83242008000300003 [Crossref] [ Google Scholar]
- Fontes ST, Fernández MR, de Moura CM, Meireles SS. Color stability of a nanofill composite: effect of different immersion media. J Appl Oral Sci 2009; 17(5):388-91. doi: 10.1590/s1678-77572009000500007 [Crossref] [ Google Scholar]
- Ardu S, Braut V, Gutemberg D, Krejci I, Dietschi D, Feilzer AJ. A long-term laboratory test on staining susceptibility of esthetic composite resin materials. Quintessence Int 2010; 41(8):695-702. [ Google Scholar]
- Abdelnaby YLA, Taymor M, Rabie ZH. Influence of the background color and thickness of zirconia reinforced glass ceramics on the optical properties compared to lithium disilicate glass ceramics. Egypt Dent J 2019; 65(4):3607-15. doi: 10.21608/edj.2019.75982 [Crossref] [ Google Scholar]
- Bagheri R, Burrow MF, Tyas M. Influence of food-simulating solutions and surface finish on susceptibility to staining of aesthetic restorative materials. J Dent 2005; 33(5):389-98. doi: 10.1016/j.jdent.2004.10.018 [Crossref] [ Google Scholar]
- Arocha MA, Mayoral JR, Lefever D, Mercade M, Basilio J, Roig M. Color stability of siloranes versus methacrylate-based composites after immersion in staining solutions. Clin Oral Investig 2013; 17(6):1481-7. doi: 10.1007/s00784-012-0837-7 [Crossref] [ Google Scholar]
- Ryan EA, Tam LE, McComb D. Comparative translucency of esthetic composite resin restorative materials. J Can Dent Assoc 2010; 76:a84. [ Google Scholar]
- Gasparik C, Culic B, Varvara MA, Grecu A, Burde A, Dudea D. Effect of accelerated staining and bleaching on chairside CAD/CAM materials with high and low translucency. Dent Mater J 2019; 38(6):987-93. doi: 10.4012/dmj.2018-335 [Crossref] [ Google Scholar]