Avicenna J Dent Res. 13(4):148-150.
doi: 10.34172/ajdr.2021.28
Case Report
Displacement and Arrest of Root Formation in a Permanent Maxillary Central Incisor Subsequent to Trauma to the Primary Predecessor: A Case Report
Arghavan Kamali Sabeti 1  , Parisa Vahedi 2, Niloofar Entezari Moghaddam 2, *
, Parisa Vahedi 2, Niloofar Entezari Moghaddam 2, * 
Author information:
1DDS, Assistant Professor of Pediatric Dentistry, Department of Pediatric Dentistry, Faculty of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran.
2DDS, Post-Graduate Student of Pediatric Dentistry, Department of Pediatric Dentistry, Faculty of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran.
3DDS, Post-Graduate Student of Pediatric Dentistry, Department of Pediatric Dentistry, Faculty of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran.
Abstract
The present report aimed to explore the case of an 8-year-old patient with chief complaint of the lack of eruption of the maxillary right permanent central incisor, referring to the Department of Pediatric Dentistry, Faculty of Dentistry, Hamadan University of Medical Sciences. The corresponding tooth on the contralateral side had fully erupted. The patient’s history revealed that the predecessor deciduous tooth had sustained a trauma, resulting in the partial intrusion of the tooth into the alveolar bone, that is, the relative intrusion of the deciduous central incisor. CBCT examinations were ordered for further evaluation, which showed the upward displacement of the permanent tooth bud in the alveolar bone as a result of the trauma, adhering to the floor of the nasal cavity. Therefore, root formation was halted, making the tooth embedded.
Keywords: Dental trauma, Intrusion, Computed tomography
Copyright and License Information
© 2021 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Kamali Sabeti A, Vahedi P, Entezari Moghaddam N. Displacement and arrest of root formation in a permanent maxillary central incisor subsequent to trauma to the primary predecessor: a case report. Avicenna J Dent Res. 2021;13(4):148-150. doi: 10.34172/ajdr.2021.28.
Background
Highlights
The prevalence of trauma in deciduous teeth is higher than that in permanent ones, and approximately 23% of children experience trauma to deciduous teeth. The majority of traumas to the deciduous dentition are inflicted on anterior teeth, especially on maxillary central incisors (1).
Due to the proximity of the apex of deciduous teeth and the buds of succedaneous permanent teeth, traumas to deciduous teeth might result in developmental disturbances in permanent teeth (2). In most cases, there is no separating hard tissue between the deciduous teeth and the buds of permanent teeth (3). Some of the sequelae in the permanent teeth after the deciduous teeth being traumatized include white or yellow-brown enamel discoloration, enamel hypoplasia, crown dilacerations, odontoma-like malformations, root duplication, root angulation or dilaceration, partial or complete cessation of root development, sequestration of the whole tooth bud, ectopic, delayed, and incomplete eruption of the tooth, and tooth impaction (4).
Partial or complete cessation of root development of a permanent tooth is a rare occurrence after trauma to the predecessor tooth and comprises 2% of the sequelae. Direct trauma to the Hertwig’s epithelial sheath gives rise to the cessation of root development. Some of these teeth remain embedded, while some other teeth erupt, which are lost due to insufficient periodontal support. The severity of these malformations depends on the permanent tooth’s developmental stage as well as the severity of the trauma (4,5).
This report aimed to illustrate a rare case concerning a clinically displacement of the bud of a maxillary permanent central incisor and the cessation of its root development after a trauma to the anterior deciduous teeth during childhood.
Case Presentation
An 8-year-old Iranian girl was referred to the Department of Pediatric Dentistry, Faculty of Dentistry, Hamadan University of Medical Science, with a chief complaint of missing maxillary central incisor. Her medical history was unremarkable, with no problem found in family history. However, the patient’s dental history showed that she had fallen from the stairs at the age of three, receiving a severe dental trauma in the anterior maxilla due to her face hitting the ground. During the incident, the deciduous right central incisor had partially intruded into the hard tissue. A local dentist had visited the child at the time of trauma; however, no dental treatment had been performed. The dentist had only recommended periodic follow-ups. The child’s parents noticed the problem when the right maxillary central incisor failed to erupt, while the contralateral tooth erupted fully; therefore, they referred to the Faculty of Hamadan Dentistry for possible treatment (Figure 1).

Figure 1.
Oblique Close up Smile Photography.
.
Oblique Close up Smile Photography.
The extraoral examination revealed a relatively convex facial profile, facial symmetry, and competent lips. Intraoral examination showed the absence of the right central incisor and the full eruption of the central incisor on the left side; however, due to the absence of the adjacent tooth on the right side, the tooth had drifted toward the midline, resulting in maxillary dental midline displacement. The molar relationship was determined as class I, with normal overjet and overbite.
After performing clinical examinations and considering a history of dental trauma, the panoramic radiographic (Figure 2) evaluation revealed that the dental bud of the right central incisor was not in its normal position since it had been displaced upwards in the alveolar bone and had undergone ankylosis at the level of the anterior nasal spine on the nasal floor bone. The tooth did not exhibit root development, while the root of the left central incisor was fully developed. The adjacent permanent teeth had fully erupted, with no pathological condition.
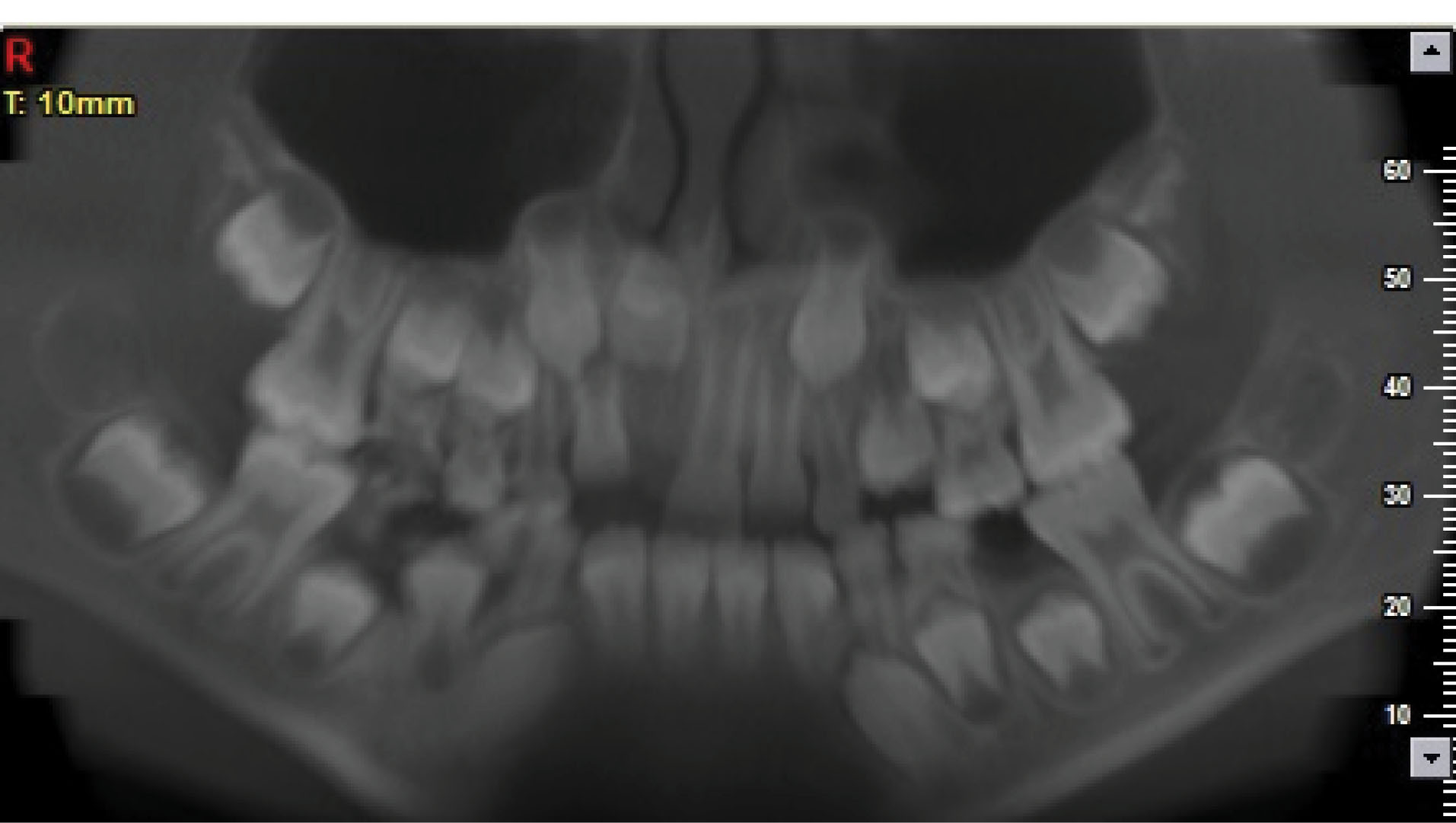
Figure 2.
Panoramic Radiograph Showing 11 Tooth Impaction.
.
Panoramic Radiograph Showing 11 Tooth Impaction.
The patient was referred to the Department of Radiology for cone beam computed tomography (Figure 3A, B, C).
The root development was evaluated at the axial cross-section, which confirmed the cessation of root development at its early stages (Nola stage 7).
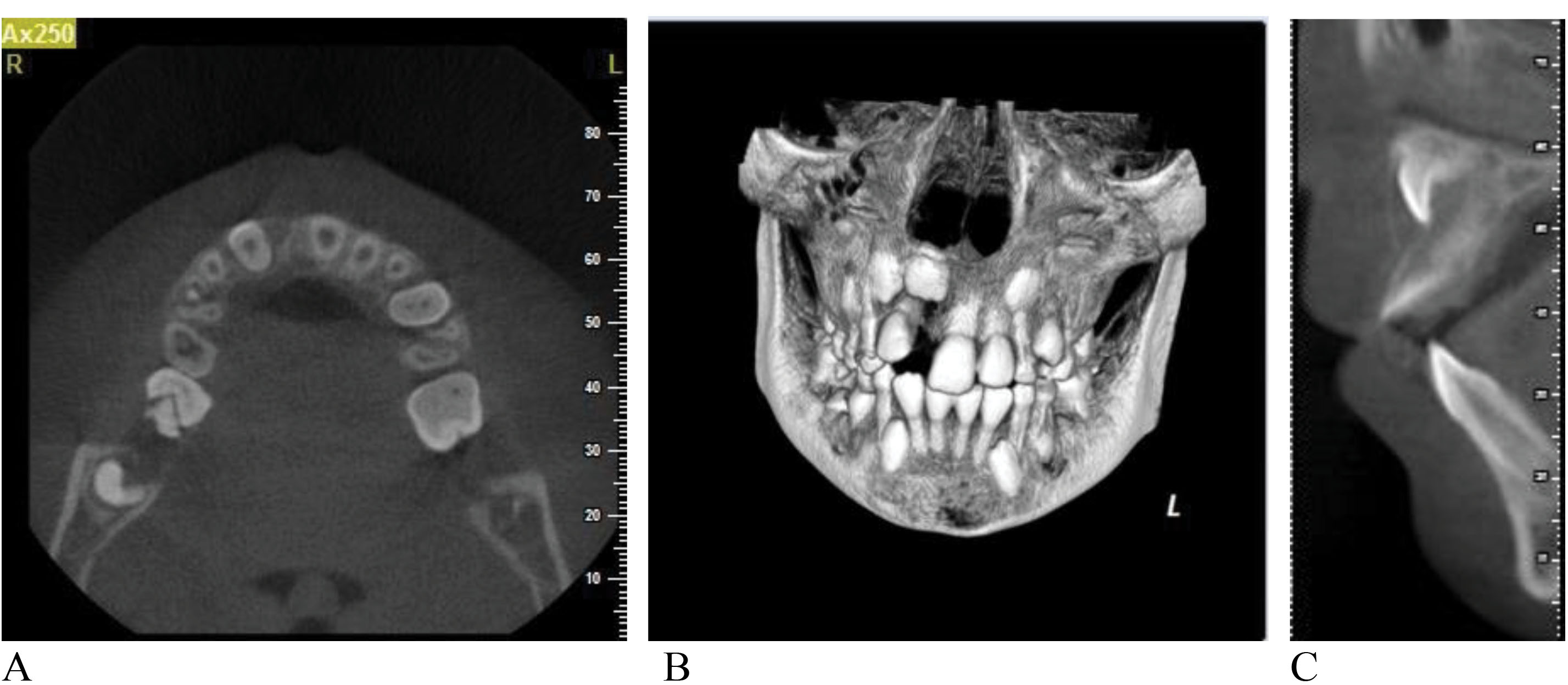
Figure 3.
CBCT View Show the Tooth Bud at the Floor of Nasal Cavity.
.
CBCT View Show the Tooth Bud at the Floor of Nasal Cavity.
A: Cross Sectional Cut, B:3D Structure, C: Axial Cut
Since the space of the permanent right central incisor had relatively been occupied by the adjacent teeth, medical counseling was conducted with the Orthodontic Department to carry out orthodontic treatment in order for regaining the lost space or the possibility of forced eruption of the impacted central incisor. The forced eruption intervention was excluded from the treatment alternatives due to the very short root of the tooth and the long route of movement until the tooth reached into the oral cavity, which increased the risk of root resorption. Furthermore, since any surgical intervention in the area could have exacerbated the bone resorption and caused the loss of the alveolar bone, it was decided that a proper dental implant would be the best option available by placing the implant in the area at the age of 18, along with the surgical removal of the impacted tooth. All things considered, the patient was put in regular dental follow ups.
Discussion
Trauma during odontogenesis stages may seriously affect the morphogenic development of the teeth. Partial or complete cessation of root development is a rare occurrence, resulting from a trauma to deciduous teeth that affects 2% of the permanent teeth (4,5). The severity of these disturbances depends on the severity of the trauma and the developmental stage of the tooth.
Maxillary central incisors are the most commonly traumatized teeth during the deciduous dentition period. The tooth buds of permanent teeth are palatal to the roots of deciduous teeth. Therefore, any trauma resulting in the palatal displacement of deciduous tooth roots might traumatize the underlying permanent tooth, and even displace it (6).
Root development follows crown development. Root development is guided by the enamel organ that forms the Hertwig’s epithelial root sheath, a developmental structure that, in turns, forms the root. Any trauma to this structure during root development might give rise to morphologic anomalies or even the cessation of root development. Therefore, these traumas occur after the completion of crown development, and before the initiation of root development (7).
According to a study by Amorim et al, the most frequent sequela in permanent teeth after trauma to deciduous teeth occurs when the children sustain the trauma at 1–3 years of age; the younger the child at the time of trauma, the higher the prevalence and severity of developmental anomalies in the buds of permanent teeth (8).
Most tooth developmental problems could be attributed to medications, genetic diseases, and systemic or metabolic diseases; therefore, the condition is usually bilateral or symmetrical, or involves several teeth (9). Besides, one of the reasons for the incidence of a rootless tooth or teeth in which the root development is halted might be dentin dysplasia, chemotherapy, and radiotherapy in the head and neck region, the management of fractures in childhood – including the use of mini-plates and surgeries during childhood – including surgeries in maxillary sinuses or the nasal cavity (5). In the present case, the patient had no diseases and took no medications. According to the usual pattern of traumatic dental injuries, moreover, only one tooth was affected unilaterally.
From among all the traumatic injuries to deciduous teeth, intrusive injuries carry the highest risk of traumas to permanent teeth (9). In the present case, and after the intrusion of the maxillary right deciduous central incisor, the succedaneous permanent tooth sustained a rare and severe sequela – that is, the cessation of the tooth root development, finally resulting in the transalveolar displacement of the tooth toward the nasal cavity floor.
Conclusions
According to the findings from this case report, it was concluded that patients who had experienced dental trauma must go through a systematic clinical and radiographic follow-up(10). It was also revealed that the severity of the damage to the permanent teeth depended on the direction and intensity of impacting force, age of the child, stage of the development of permanent tooth germ, and the amount of dissipation of the impacting force (11). Furthermore, this report found that the severe nature of trauma in the present case had led to intrusion of primary left central incisor and impaction of permanent substitute tooth (11). Finally, the longitudinal radiographic follow-up was proved extremely important to the success of the treatment.
Conflict of Interest Disclosures
The authors declare that they have no conflict of interests.
Ethical Statement
Informed consent was obtained from the parents of patient.
References
- Petti S. Andersson L, Day P, Kenny K, Glendor U, Andreasen JO. Textbook and Color Atlas of Traumatic Dental Injuries to the Teeth. 5th ed. Wiley; 2019. Chapter 11: Classification, Epidemiology and Etiology; p.262,266.
- Smith RJ, Rapp R. A cephalometric study of the developmental relationship between primary and permanent maxillary central incisor teeth. ASDC J Dent Child 1980; 47(1):36-41. [ Google Scholar]
- Andreasen JO. The influence of traumatic intrusion of primary teeth on their permanent successors A radiographic and histologic study in monkeys. Int J Oral Surg 1976; 5(5):207-19. doi: 10.1016/s0300-9785(76)80016-6 [Crossref] [ Google Scholar]
- Andreasen JO, Sundström B, Ravn JJ. The effect of traumatic injuries to primary teeth on their permanent successors I A clinical and histologic study of 117 injured permanent teeth. Scand J Dent Res 1971; 79(4):219-83. doi: 10.1111/j.1600-0722.1971.tb02013.x [Crossref] [ Google Scholar]
- Subramaniam P, Gupta M, Gona H. Arrest of root formation in relation to permanent mandibular incisors: a rare case report. J Contemp Dent Pract 2013; 14(3):552-5. doi: 10.5005/jp-journals-10024-1361 [Crossref] [ Google Scholar]
- Moss SJ, Maccaro H. Examination, evaluation and behavior management following injury to primary incisors. N Y State Dent J 1985; 51(2):87-92. [ Google Scholar]
- Sicher H, Bhasker SN. Orban’s Oral Histology and Embryology. 7th ed. St. Louis: CV Mosby Co; 1972. p. 17-37.
- de Fátima Guedes de Amorim F, Estrela C, da Costa LR. Effects of traumatic dental injuries to primary teeth on permanent teeth--a clinical follow-up study. Dent Traumatol 2011; 27(2):117-21. doi: 10.1111/j.1600-9657.2010.00959.x [Crossref] [ Google Scholar]
- von Arx T. Developmental disturbances of permanent teeth following trauma to the primary dentition. Aust Dent J 1993; 38(1):1-10. doi: 10.1111/j.1834-7819.1993.tb05444.x [Crossref] [ Google Scholar]
- Miranda C, Luiz BK, Cordeiro MM. Consequences of dental trauma to the primary teeth on the permanent dentition. RSBO 2012; 9(4):457-62. [ Google Scholar]
- Tewari N, Pandey RK. Multiple abnormalities in permanent maxillary incisors following trauma to the primary dentition. J Indian Soc Pedod Prev Dent 2011; 29(2):161-4. doi: 10.4103/0970-4388.84691 [Crossref] [ Google Scholar]