Avicenna J Dent Res. 12(4):142-147.
doi: 10.34172/ajdr.2020.28
Review Article
Examining the Effect of Laser Radiation on the Repair of Dental Composite Restorations: A Systematic Review
Loghman Rezaei-Soufi 1  , Fatemeh Maddah 2, *
, Fatemeh Maddah 2, *  , Younes Mohammadi 3
, Younes Mohammadi 3
Author information:
1Associate Professor of Restorative Dentistry, Department of Restorative Dentistry, School of Dentistry, Dental Research Center, Hamadan University of Medical Sciences, Hamadan, Iran.
2Postgraduate Student of Operative and Esthetic Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran.
3Associate Professor of Epidemiology, Department of Epidemiology, School of Health, Hamadan University of Medical Sciences, Hamadan, Iran.
Abstract
Background: This study aimed to determine the impact of laser radiation on the repair bond strength of dental composite restorations by gathering, assessing, and systematically reviewing previous articles referring to this issue.
Methods: Several previous studies relevant to the objectives of this research were found in PubMed, Scopus, and Web of Science databases. All prior articles indexed in these databases according to the selected keywords until 2018 were gathered and assessed. Some article abstracts showed the necessary basic conditions for inclusion in the study. Therefore, the full texts of these relevant articles were further evaluated in terms of the study objectives.
Results: A total of 300 relevant articles were obtained by searching the databases. Eight studies remained highly relevant after performing a title review, eliminating the duplicate articles, and implementing the selection criteria. The latest study was conducted in 2018. A statistically significant difference was observed between the impacts of laser and other methods in the seven of these final relevant studies. Of these articles, five indicated a better impact in the case of other methods, particularly the dental milling technique, and one study was related to the impacts of the laser method. Additionally, the Er,Cr: YSGG laser was considered the most adequate laser in these studies.
Conclusions: According to the review of prior studies on the impact of laser radiation on the repair bond strength of composite restorations, Er: YAG and Er,Cr: YSGG lasers are advised for surface preparation of composites. However, surface preparation by adopting the milling technique remains the adequate choice for repairing composites.
Keywords: Laser, Composite repair, Surface treatment
Copyright and License Information
© 2020 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Rezaei-Soufi L, Maddah F, Mohammadi Y. Examining the effect of laser radiation on the repair of dental composite restorations: a systematic review. Avicenna J Dent Res. 2020;12(4):142-147. doi: 10.34172/ajdr.2020.28.
Background
Highlights
-
The use of milling is still the best choice for repairing composite
-
The use of Er,cr: YSGG and Er:YAG laser is recommended for composite surface preparation
The demand for cosmetic restorations, the emergence of novel adhesives and curing systems alongside the progress made in material properties have rendered dental composites as the most prevalent direct restoration materials (1). Resin-based composites are materials selected for the restoration of anterior and posterior teeth. The annual failure rate for anterior and posterior composite restorations ranges approximately between 1% and 4% (2,3). Shrinkage resulting from polymerization, also known as polymerization shrinkage, is still regarded among the most critical consequences of conventional methacrylate-based composites (4). Shrinkage may cause microleakage, edge discoloration, and gap formation, further acting as one of the primary determinants in the occurrence of secondary caries (5). In most cases, intra-oral repair of restorations is preferred to total replacement (6).
However, defective restorations should be examined thoroughly for repair. Moreover, according to the concept of minimally invasive restorative dentistry, total replacement should be avoided, except in cases where a fracture in the composite, discoloration of the resin contact surface with the tooth, and secondary caries are observed (7). This method helps to preserve healthy dental tissues (8).
The dentist has three main methods to deal with defective restorations in the composite restoration failure cases, namely restoration, repair, and replacement. Restoration implies that no extra material or dental structure will be removed; however, additional restorative material will be applied to fix the defective structure (9,10). Meanwhile, the repair is a process that involves the relative removal of a defective repair, which is then repaired with brand new materials (10). Replacement involves complete removal of the defective composite (even clinically acceptable parts) to replace it with new material. Practically, the removal of a healthy tooth is inevitable in this method (11). Studies have shown that composite repair procedures may prolong the life of dental restorations (12,13).
Brosh et al indicated that devising a single bond between the old and the new composite during the repair process is attainable through three respective mechanisms, namely (a) chemical bond to the organic matrix, (b) chemical bond to the exposed fillers, and (c) micromechanical trap (8). Preceding studies have determined the efficacy of micromechanical traps created by diamond milling, sandblasting, or acid etching in the bond strength of repaired composites (14).
The use of lasers is another technique for generating surface abrasion. According to studies, Erbium group lasers, namely Nd: YAG and CO2 Cr: YSGG, have been employed in this process. It has been confirmed that Er: YSGG laser can be employed in dentistry for the removal of tooth decay and conditioning of dental surfaces, enamel, and dentin purposes. Özel Bektas et al examined the impact of Er: YAG laser, milling, and thermal cycle on the shear bond strength of repaired composite resins. The laser and milling procedure samples were confirmed to display similar results following the shear bond strength test. Aging with 10000 thermocycles significantly affected the restoration bond strength of composite resins (13).
Nevertheless, the results are not consistent in all cases. Accordingly, we tried to gather several articles in this field and review their results as an approach to examine the impact of laser application on the repair process of composite restorations given the extended use of lasers in modern dentistry and considering numerous prior studies that have produced diverse results. Furthermore, this study aimed to demonstrate the importance of restoring dental composites rather than replacement.
Materials and Methods
Protocol, Registration, Search, and Study Selection
The previous studies were searched in three international databases: Web of Science, PubMed, and Scopus. The selection procedure was conducted up to the publication date (2018). The adopted search strategy was Laser AND Composite repair AND Surface treatment. Additionally, reference and source lists, along with the related articles, were similarly reviewed to increase the search sensitivity (Figure 1).
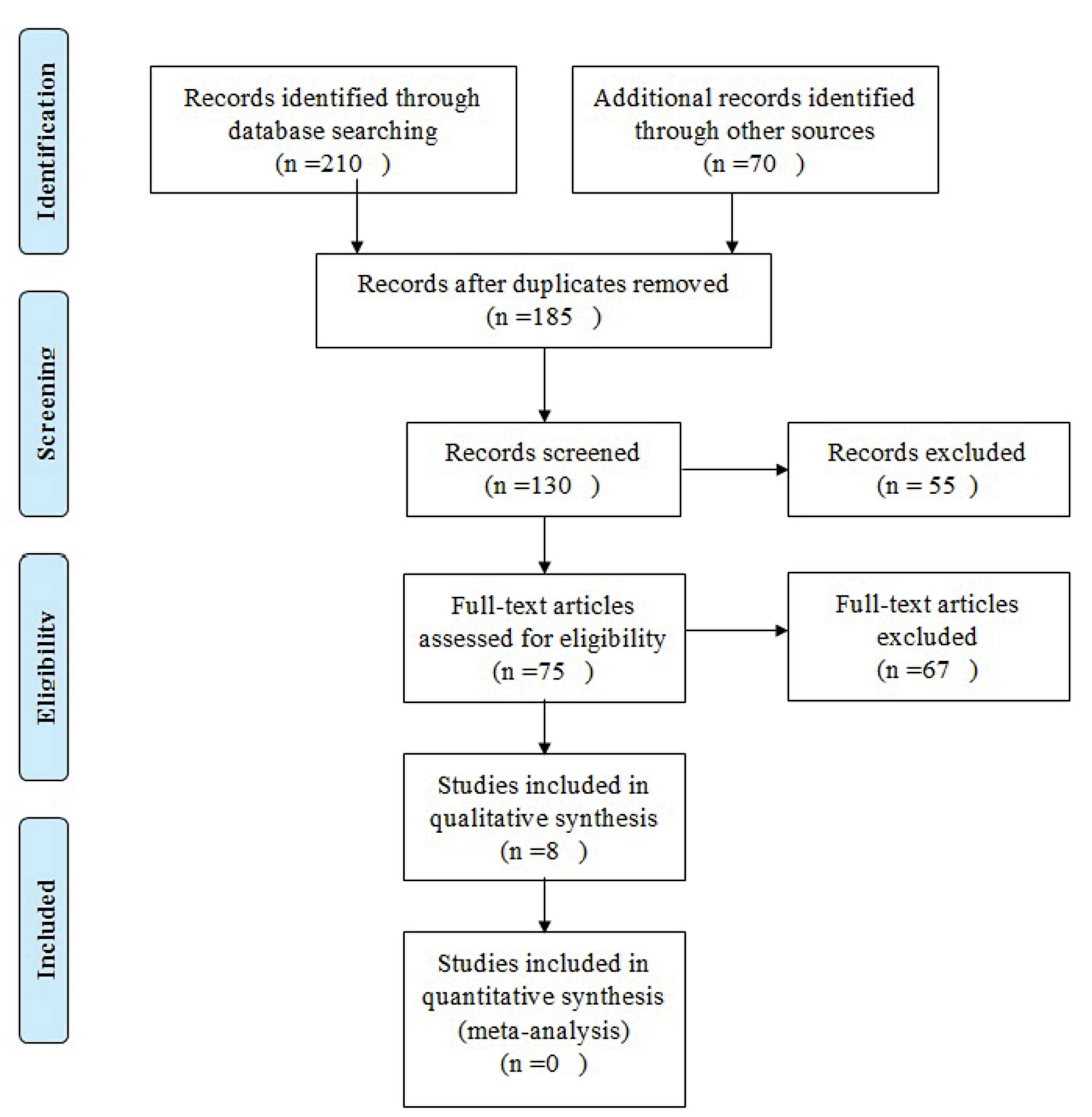
Figure 1.
Flowchart of the systematic review
.
Flowchart of the systematic review
Inclusion Criteria
-
All types of composites employed for dental composite repair studies
-
All types of lasers employed in dental composite repair studies
-
All surface preparation methods employed for the composite repair process
-
All types of aged or non-aged dental composites
-
All types of dental or composite samples for dental composite repair studies
Data Collection
We devised a data extraction form to gather the data, which included research information such as the corresponding author’s name, year of publication, country, journal name, sample size, mean, and standard deviation. Following the extraction, the retrieved articles from various databases were imported into the Endnote software and duplicate articles were eliminated. The respective titles and abstracts of the remaining relevant articles were then examined. At this point, articles that had examined the impact of laser application on the repair process of composite restorations were incorporated into the study.
Risk of Bias Across Studies
Two faculty members assessed each article at three levels of low, average, and adequate.
Results
A total of 300 relevant articles were obtained from three respective databases, namely Web of Science, PubMed, and Scopus. Eight studies remained relevant (4,15-21) after reviewing the title, eliminating duplicate articles, and evaluating the study selection criteria. The majority of these eight selected studies have been conducted in Iran, and the most recent study belonged to 2018 (20). The obtained studies indicated that three types of lasers including Er, Cr: YSGG, CO2, and Nd: YAG were studied and compared with the aid of methods including air abrasion, milling, silane, hydrofluoric acid, aluminum oxide, and sandblast. The highest bond strength (30.44) was reported by Dinç Ata et al (20) using the Er, Cr: YSGG laser. The lowest bond strength (4.75) pertained to a study done by Kiomarsi et al in 2017 (17). Moreover, the highest average bond strength of other methods (33.85) was also employed by Dinç Ata et al (20) using the milling method. On the other hand, the lowest average bond strength (2.60) was reported by Barcellos et al using silane and hydrofluoric acid (15). A statistically significant difference was observed between the impacts of laser and other methods in the seven of these final relevant studies, of which five studies indicated a better impact in the case of other methods, particularly dental milling technique, and one study dealt with the impacts of the laser method. Additionally, the Er. Cr: YSGG laser was deemed the most adequate laser in these studies (see Table 1).
Table 1.
Descriptive Characteristics of the Studies Entered the Systematic Stage of the Review
|
Author
|
Study Place
|
Year
|
Volume Sample
|
Method
|
Average (Bond Strength)
|
Standard Deviation (Bond Strength)
|
Highest Average Bond Strength In Each Study
|
Reference
|
Quality
|
| Barcellos et al |
Brazil |
2015 |
84 |
Laser |
7.50 |
3.50 |
Scotchbond |
15 |
Adequate |
| Scotchbond |
9.50 |
4.60 |
|
|
| Sandblast |
18.70 |
4.60 |
|
|
| Aluminum oxide |
18.80 |
4.70 |
|
|
| Silane |
2.60 |
2.30 |
|
|
| Hydrofluoric acid |
2.60 |
3.80 |
|
|
| Alizadeh Oskoee et al |
Iran |
2017 |
76 |
Er,Cr;YSGG laser |
8.99 |
1.16 |
Er,Cr;YSGG laser |
16 |
Adequate |
| CO2 laser |
7.20 |
1.27 |
|
|
| Nd;YAG Laser |
7.33 |
1.16 |
|
|
| No treatment |
6.69 |
1.68 |
|
|
| Kiomarsi et al |
Iran |
2017 |
120 |
Laser |
4.75 |
1.73 |
|
17 |
Average |
| Milling |
13.85 |
2.50 |
Milling |
|
| Duran et al |
Turkey |
2015 |
60 |
Laser |
19.65 |
0.72 |
|
18 |
Adequate |
| Sandblast |
33.41 |
1.16 |
Sandblast |
|
| Cho et al |
USA |
2013 |
60 |
Laser |
14.20 |
1.40 |
|
19 |
Adequate |
| Air abrasive |
18.8 |
1.3 |
Air abrasive |
|
| Tribochemical |
17.4 |
1.4 |
|
Adequate |
| Dinç Ata et al |
Turkey |
2018 |
60 |
Er,Cr;YSGG laser |
30.44 |
7.30 |
|
20 |
|
| Nd;YAG laser |
19.96 |
4.68 |
|
|
| Milling |
33.85 |
11.30 |
Milling |
|
| Rossato et al |
Brazil |
2009 |
60 |
Aluminum oxide |
8.91 |
2.53 |
Aluminum oxide |
21 |
Adequate |
| Er,Cr;YSGG Laser |
7.67 |
1.66 |
|
|
| Milling |
8.47 |
0.75 |
|
Average |
| Malekipour et al |
Iran |
2016 |
32 |
Sandblast |
19.51 |
1.56 |
Sandblast |
4 |
|
| Silane |
10.05 |
2.70 |
|
|
| Er,Cr;YSGG Laser |
16.46 |
1.65 |
|
|
Discussion
In this study, an attempt was made to compare the impact of laser radiation on the bond strength of the composite repair process and the other methods. The results obtained from prior studies reveal that the laser radiation method has an inadequate impact on bond strength compared to the other surface preparation methods. On the contrary, the laser displayed a more remarkable impact compared to the other methods used in a study by Alizadeh Oskoee et al, although this difference was not statistically significant (16). Dinç Ata et al (20) further showed that the highest bond strength obtained belonged to the milling method. Rodriguez et al and Costa et al in scanning electron microscope (SEM) evaluations of sandblasted composite surfaces revealed that slight surface roughness expands the surface area available for the bond, and thus reinforces the bond strength by implementing this preparation method (22,23). Denehy et al suggest that the success of composite resin repair depends on two measures, namely surface preparation and proper application of the adhesive system (24). According to Brosh et al, a solid bond can be formed between the new and old composites during the repair process through three respective mechanisms 1) chemical bonding to the organic matrix, 2) chemical bonding to the exposed fillers, and 3) micromechanical trapping (14). The same type of chemical bond between new and old monomers is suggested similarly in the process of repairing methacrylate bases with composites. However, relying on this type of bond without any surface preparation has not presented satisfactory results given the inadequate number of free radicals remaining during artificial or natural aging (22,23,25). Consequently, it is necessary to utilize valid surface preparation methods to attain convenient contact levels. However, a chemical bond between the two matrices is not conceivable in the case of methacrylate to silane-based bonds, given the distinct types of monomers and their unique polymerization methods. As a result, the other two previously discussed mechanisms are relevant in building an adequate bond (26). Several surface preparation methods have been proposed to increase micromechanical adhesion and the wettability of older composites, such as acid etching, milling, sandblasting, and laser radiation methods, respectively (27). Immediate repair of composite bond strength such as the cohesive strength repair brings forth the presence of an oxygen inhibitory layer. Nevertheless, further determinants such as the decrease concerning the number of active monomers, polishing, and structural change alter the composite bond strength, repair procedure, and post-aging process (28).
Differences observed in the matrix polymer structure and fillers can lead to consequent differences in bond strength (24,29). Beyer et al showed that the optimal clinical bond strength is equal to 60%-70% of the cohesive strength (23). An enamel composite strength that ranges between 15 and 30 MPa under clinical conditions is deemed adequate in this regard (30-32). Some authors maintain that the resulting interface bond must amount to higher than 18 MPa, or may range between 20 and 25 MPa, to be considered valid and perform adequately under clinical conditions (33,34). With the above explanations in mind, it is resolved that sandblasting with alumina or Erbium laser methods should be utilized in the composite repair processes (both methacrylate-based and silane-based), and disregarding the surface preparation process or silane use are not sufficient to obtain the adequate bond strength (5). The present study indicates that the highest bond strength obtained belonged to the milling method, followed by the laser preparation method, and then the sandblasting method. The use of Erbium laser in the removal of dental cement, as well as the associated selective ablation in the composite restoration procedures, has been further evaluated (35). Composite ablation with Er: YAG laser is performed through explosive evaporation, followed by hydrodynamic launching. Strong expansion forces are generated during this process of rapid melting and volume change is observed in the material. Protrusions emerge on the surface, and the molten material is subsequently withdrawn from the surface in the form of droplets due to the interaction of the generated forces and the structure of the composite (26,36,37). Accordingly, it appears that laser irradiation is not convenient for surface preparation of aged silane-based composites (38). The morphological properties of the surface resulting from laser ablation depend on the features of the radiated laser beam and the composite structure it impacts (13). Alizadeh Oskoee et al assessed the impact of various surface preparation methods, including sandblasting, Er: YAG laser, and diamond milling, on the bond strength of repaired silane-based composites. The results showed that both laser and diamond milling methods had performed effectively in repairing silane-based composite, indicating that the results of these two methods were superior to the sandblasting method. However, the laser bond strength was observed to be higher than the sandblast bond strength in a study by Alizadeh Oskoee et al, which is contrary to the results obtained from the present study. This disparity may be due to the differences in laser parameters of the two studies. Nevertheless, more SEM studies are required to compare the laser-irradiated and sandblasted surfaces (39). The findings of recent studies suggested that although the bond strength repair procedure by laser has been more prevalent compared to the other methods, this difference is not statistically significant (P > 0.05). A recent study has detailed the efficacy of the composite repair method using the Er, Cr: YSGG laser (40). The blue laser cuts the hard tissue with the aid of particles and high energy. Water molecules with surface energy wear the composite to maintain the surface temperatures low, leading to a decrease in the probability of the formation of subsurface microcracks that function as stress enhancers in the future. Water molecules with surface energy also generate a clean surface by eliminating composite debris during the abrasion process. This situation may provide a better composite strength repair outcome than the Nd: YAG application adopted in this study. Nevertheless, further studies are required to illustrate the advantages of employing Er, Cr: YSGG lasers in composite repair processes (41,42).
Limitations of the Study
-
The number of relevant articles or prior studies was limited and thus more studies are suggested to be conducted in this regard.
-
We could not conduct a meta-analysis due to the major disparities observed between studies, including differences between lasers, comparison groups, composite types, etc.
Conclusions
Er: YAG and Er,Cr: YSGG lasers are advised for surface preparation of composites according to the review of prior studies on the impact of laser radiation on the repair bond strength of composite restorations. However, surface preparation by adopting the milling technique remains the adequate choice for repairing composites.
Authors’ Contribution
FM as the responsible author - LR as the supervisor - YM as the statistical consultant participated in this study.
Ethical Statement
Not applicable.
Conflict of Interest Disclosures
The authors declare that they have no conflict of interests.
Acknowledgments
This article is the result of a research project approved by the Vice-Chancellor for Research at Hamadan University of Medical Sciences, with project number 9712077556. We hereby sincerely thank our esteemed colleagues for their guidance, help, and support.
References
- Papacchini F, Magni E, Radovic I, Mazzitelli C, Monticellia F, Goracci C. Effect of intermediate agents and pre-heating of repairing resin on composite-repair bonds. Oper Dent 2007; 32(4):363-71. doi: 10.2341/06-105 [Crossref] [ Google Scholar]
- Schmidt M, Kirkevang LL, Hørsted-Bindslev P, Poulsen S. Marginal adaptation of a low-shrinkage silorane-based composite: 1-year randomized clinical trial. Clin Oral Investig 2011; 15(2):291-5. doi: 10.1007/s00784-010-0446-2 [Crossref] [ Google Scholar]
- Demarco FF, Collares K, Coelho-de-Souza FH, Correa MB, Cenci MS, Moraes RR. Anterior composite restorations: a systematic review on long-term survival and reasons for failure. Dent Mater 2015; 31(10):1214-24. doi: 10.1016/j.dental.2015.07.005 [Crossref] [ Google Scholar]
- Malekipour MR, Shirani F, Hurmehr Z. Evaluation of the effect of surface treatments on shear bond strength of repaired silorane-based composites. J Mashhad Dent Sch 2016; 40(3):259-68. [ Google Scholar]
- Ferracane JL. Current trends in dental composites. Crit Rev Oral Biol Med 1995; 6(4):302-18. doi: 10.1177/10454411950060040301 [Crossref] [ Google Scholar]
- Oztas N, Alaçam A, Bardakçy Y. The effect of air abrasion with two new bonding agents on composite repair. Oper Dent 2003; 28(2):149-54. [ Google Scholar]
- Tyas MJ, Anusavice KJ, Frencken JE, Mount GJ. Minimal intervention dentistry--a review FDI Commission Project 1-97. Int Dent J 2000; 50(1):1-12. doi: 10.1111/j.1875-595x.2000.tb00540.x [Crossref] [ Google Scholar]
- Popoff DAV, Gonçalves FS, Ferreira RC, Magalhães CS, Moreira AN, Mjör IA. Repair of amalgam restorations with conventional and bonded amalgam: an in vitro study. Rev Odonto Ciênc 2010; 25(2):154-8. doi: 10.1590/s1980-65232010000200009 [Crossref] [ Google Scholar]
- Fernández E, Martín J, Vildósola P, Oliveira Junior OB, Gordan V, Mjor I. Can repair increase the longevity of composite resins? results of a 10-year clinical trial. J Dent 2015; 43(2):279-86. doi: 10.1016/j.jdent.2014.05.015 [Crossref] [ Google Scholar]
- Moncada G, Martin J, Fernández E, Hempel MC, Mjör IA, Gordan VV. Sealing, refurbishment and repair of Class I and Class II defective restorations: a three-year clinical trial. J Am Dent Assoc 2009; 140(4):425-32. doi: 10.14219/jada.archive.2009.0191 [Crossref] [ Google Scholar]
- Hickel R, Brüshaver K, Ilie N. Repair of restorations--criteria for decision making and clinical recommendations. Dent Mater 2013; 29(1):28-50. doi: 10.1016/j.dental.2012.07.006 [Crossref] [ Google Scholar]
- Bonstein T, Garlapo D, Donarummo J Jr, Bush PJ. Evaluation of varied repair protocols applied to aged composite resin. J Adhes Dent 2005; 7(1):41-9. doi: 10.3290/j.jad.a10084 [Crossref] [ Google Scholar]
- Özel Bektas Ö, Eren D, Herguner Siso S, Akin GE. Effect of thermocycling on the bond strength of composite resin to bur and laser treated composite resin. Lasers Med Sci 2012; 27(4):723-8. doi: 10.1007/s10103-011-0958-2 [Crossref] [ Google Scholar]
- Brosh T, Pilo R, Bichacho N, Blutstein R. Effect of combinations of surface treatments and bonding agents on the bond strength of repaired composites. J Prosthet Dent 1997; 77(2):122-6. doi: 10.1016/s0022-3913(97)70224-5 [Crossref] [ Google Scholar]
- Barcellos DC, Miyazaki Santos VM, Niu LN, Pashley DH, Tay FR, Pucci CR. Repair of composites: effect of laser and different surface treatments. Int J Adhes Adhes 2015; 59:1-6. doi: 10.1016/j.ijadhadh.2015.01.008 [Crossref] [ Google Scholar]
- Alizadeh Oskoee P, Savadi Oskoee S, Rikhtegaran S, Pournaghi Azar F, Gholizadeh S, Aleyasin Y. Effect of various laser surface treatments on repair shear bond strength of aged silorane-based composite. J Lasers Med Sci 2017; 8(4):186-90. doi: 10.15171/jlms.2017.34 [Crossref] [ Google Scholar]
- Kiomarsi N, Espahbodi M, Chiniforush N, Karazifard MJ, Hashemi Kamangar SS. In vitro evaluation of repair bond strength of composite: effect of surface treatments with bur and laser and application of universal adhesive. Laser Ther 2017; 26(3):173-80. doi: 10.5978/islsm.17-OR-12 [Crossref] [ Google Scholar]
- Duran İ, Ural Ç, Yilmaz B, Tatar N. Effects of Er:YAG laser pretreatment with different energy levels on bond strength of repairing composite materials. Photomed Laser Surg 2015; 33(6):320-5. doi: 10.1089/pho.2014.3859 [Crossref] [ Google Scholar]
- Cho SD, Rajitrangson P, Matis BA, Platt JA. Effect of Er,Cr:YSGG laser, air abrasion, and silane application on repaired shear bond strength of composites. Oper Dent 2013; 38(3):E1-9. doi: 10.2341/11-054-l [Crossref] [ Google Scholar]
- Dinç Ata G, Yilmaz B, Irmak Ö. Laser type effects on repair bond strength of ormocers and nanoceramic based composites. J Adhes Sci Technol 2018; 32(20):2204-19. doi: 10.1080/01694243.2018.1468523 [Crossref] [ Google Scholar]
- Rossato DM, Bandéca MC, Saade EG, Lizarelli RFZ, Bagnato VS, Saad JRC. Influence of Er:YAG laser on surface treatment of aged composite resin to repair restoration. Laser Phys 2009; 19(11):2144. doi: 10.1134/s1054660x09210105 [Crossref] [ Google Scholar]
- Rodriguez GDR, Pereira SNA. Current trends and evolution on dental composites. Acta Odontol Venez 2008; 46(3):1-18. [ Google Scholar]
- Costa TR, Ferreira SQ, Klein-Júnior CA, Loguercio AD, Reis A. Durability of surface treatments and intermediate agents used for repair of a polished composite. Oper Dent 2010; 35(2):231-7. doi: 10.2341/09-216-l [Crossref] [ Google Scholar]
- Denehy G, Bouschlicher M, Vargas M. Intraoral repair of cosmetic restorations. Dent Clin North Am 1998; 42(4):719-37. [ Google Scholar]
- Lührs AK, Görmann B, Jacker-Guhr S, Geurtsen W. Repairability of dental siloranes in vitro. Dent Mater 2011; 27(2):144-9. doi: 10.1016/j.dental.2010.09.009 [Crossref] [ Google Scholar]
- Correa-Afonso AM, Palma-Dibb RG, Pécora JD. Composite filling removal with erbium: yttrium-aluminum-garnet laser: morphological analyses. Lasers Med Sci 2010; 25(1):1-7. doi: 10.1007/s10103-008-0581-z [Crossref] [ Google Scholar]
- Özcan M, Barbosa SH, Melo RM, Galhano GA, Bottino MA. Effect of surface conditioning methods on the microtensile bond strength of resin composite to composite after aging conditions. Dent Mater 2007; 23(10):1276-82. doi: 10.1016/j.dental.2006.11.007 [Crossref] [ Google Scholar]
- Brendeke J, Ozcan M. Effect of physicochemical aging conditions on the composite-composite repair bond strength. J Adhes Dent 2007; 9(4):399-406. [ Google Scholar]
- Ramoglu SI, Usumez S, Buyukyilmaz T. Accelerated aging effects on surface hardness and roughness of lingual retainer adhesives. Angle Orthod 2008; 78(1):140-4. doi: 10.2319/112106-473.1 [Crossref] [ Google Scholar]
- Jafarzadeh Kashi TS, Erfan M, Rakhshan V, Aghabaigi N, Tabatabaei FS. An in vitro assessment of the effects of three surface treatments on repair bond strength of aged composites. Oper Dent 2011; 36(6):608-17. doi: 10.2341/10-386-l [Crossref] [ Google Scholar]
- Turner CW, Meiers JC. Repair of an aged, contaminated indirect composite resin with a direct, visible-light-cured composite resin. Oper Dent 1993; 18(5):187-94. [ Google Scholar]
- Teixeira EC, Bayne SC, Thompson JY, Ritter AV, Swift EJ. Shear bond strength of self-etching bonding systems in combination with various composites used for repairing aged composites. J Adhes Dent 2005; 7(2):159-64. [ Google Scholar]
- Puckett AD, Holder R, O’Hara JW. Strength of posterior composite repairs using different composite/bonding agent combinations. Oper Dent 1991; 16(4):136-40. [ Google Scholar]
- Kupiec KA, Barkmeier WW. Laboratory evaluation of surface treatments for composite repair. Oper Dent 1996; 21(2):59-62. [ Google Scholar]
- Lizarelli R, Moriyama LT, Bagnato VS. Ultraconservative ablation in operative and esthetic dentistry. J Oral Laser Applic 2003; 3:73-8. [ Google Scholar]
- Lizarelli R, Moriyama LT, Bagnato VS. Ablation of composite resins using Er:YAG laser--comparison with enamel and dentin. Lasers Surg Med 2003; 33(2):132-9. doi: 10.1002/lsm.10196 [Crossref] [ Google Scholar]
- Hossain M, Nakamura Y, Yamada Y, Murakami Y, Matsumoto K. Microleakage of composite resin restoration in cavities prepared by Er,Cr:YSGG laser irradiation and etched bur cavities in primary teeth. J Clin Pediatr Dent 2002; 26(3):263-8. doi: 10.17796/jcpd.26.3.q8747j711g425582 [Crossref] [ Google Scholar]
- Beyer E, Behter K, Petschke U. . Schweissen mit CO2-Lasern 1989.
- Alizadeh Oskoee P, Mohammadi N, Ebrahimi Chaharom ME, Kimyai S, Pournaghi Azar F, Rikhtegaran S. Effect of surface treatment with Er;Cr:YSSG, Nd:YAG, and CO2 lasers on repair shear bond strength of a silorane-based composite resin. J Dent Res Dent Clin Dent Prospects 2013; 7(2):61-6. doi: 10.5681/joddd.2013.011 [Crossref] [ Google Scholar]
- Kimyai S, Mohammadi N, Jafari Navimipour E, Rikhtegaran S. Comparison of the effect of three mechanical surface treatments on the repair bond strength of a laboratory composite. Photomed Laser Surg 2010; 28 Suppl 2:S25-30. doi: 10.1089/pho.2009.2598 [Crossref] [ Google Scholar]
- van As G. Erbium lasers in dentistry. Dent Clin North Am 2004; 48(4):1017-59. doi: 10.1016/j.cden.2004.06.001 [Crossref] [ Google Scholar]
- Iaria G. Clinical, morphological, and ultrastructural aspects with the use of Er:YAG and Er,Cr:YSGG lasers in restorative dentistry. Gen Dent 2008; 56(7):636-9. [ Google Scholar]