Avicenna J Dent Res. 13(1):13-17.
doi: 10.34172/ajdr.2021.03
Original Article
Comparing Periodontal Status Between Pregnant Women with Preeclampsia and Normal Women
Ilnaz Farhoodi 1, Zahra Mortazavi 2, *, Roghayeh Dargahi 3, Abbas Naghizadeh Baghi 4
Author information:
1Assistant Professor of Periodontology, Ardabil University of Medical Sciences, Ardabil, Iran.
2Dental Student, Faculty of Dentistry, Ardabil University of Medical Sciences, Ardabil, Iran.
3Associate Professor of Gynecology, Ardabil University of Medical Sciences, Ardabil, Iran.
4Associate Professor of Sport Management, Department of Physical Education, Sport & Psychology, University of Mohaghegh Ardebili, Ardabil, Iran.
Abstract
Background: Periodontal disease is a common disorder in approximately 5%-10% of all pregnant women. The evidence suggests that periodontitis can increase the risk of preeclampsia. It seems that chronic systemic inflammation resulting from periodontal disease may be an important factor. However, some studies have ruled out any correlation between periodontal disease parameters and blood pressure. Therefore, this study was conducted to determine the correlation between periodontal disease and preeclampsia in Iranian pregnant women.
Methods: This case-control study was conducted on 40 randomly selected preeclamptic patients as the case group and 40 randomly selected healthy pregnant women as the control group aged up to 35 years with gestational age of less than 34 weeks. Preeclampsia was diagnosed by a gynecologist as sustained pregnancy-induced hypertension (BP≥140/90 mm Hg within 6 hours) with proteinuria (with urine protein concentrations ≥1 mg/dl on a catheterized urine sample). All the participants underwent periodontal examinations, including the measurements of the pocket depth (PD), clinical attachment loss (CAL), bleeding on probing (BOP), and plaque index (PI) in all the teeth except the third molar and second distal molar teeth. Statistical analysis was performed using the Mann-Whitney U test and P<0.05 was considered as statistically significant.
Results: The results showed that prevalence of periodontal disease was significantly higher in the preeclamptic group. The quantitative analysis of periodontal parameters between the groups indicated that mean values of the BOP, CAL, PD, and PI were significantly higher in the preeclamptic group, compared to those reported for the control group (P<0.001).
Conclusions: The results of the present study showed that periodontal indices are more severe in pregnant women with preeclampsia, compared to those reported for normal pregnant subjects.
Keywords: Periodontal disease, Periodontitis, Preeclampsia, Pregnancy
Copyright and License Information
© 2021 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Farhoodi I, Mortazavi Z, Dargahi R, Naghizadeh Baghi A. Comparing periodontal status between pregnant women with preeclampsia and normal women. Avicenna J Dent Res. 2021;13(1):13-17. doi: 10.34172/ajdr.2021.03.
Background
Highlights
-
The prevalence of periodontal disease was significantly higher in the preeclamptic group.
-
The amount of bleeding on probing (BOP) was significantly higher in the preeclamptic group.
-
The clinical attachment loss (CAL) ratio was significantly higher in the preeclamptic group.
-
The pocket depth (PD) ratio was significantly higher in the preeclamptic group.
-
The plaque index (PI) increased in the preeclamptic group.
Periodontal disease is a common disorder that arises from the chronic infection of gingiva and dental supportive structures (1,2). It is a high-prevalence disorder affecting about 20-50% of pregnant women (3,4). Smoking, systemic disease, steroids, anti-epileptic drugs, cancer drugs, contraceptive pills, pregnancy, crooked teeth, and ill-fitting bridges are the risk factors for periodontal diseases (5,6). Moreover, scientific evidence suggests that periodontal disease can increase the risk of such diseases as atherosclerosis, myocardial infarction, diabetes mellitus, and recently preeclampsia (7). Among the aforementioned cases, preeclampsia is a vascular disorder of pregnancy defined by sustained hypertension with proteinuria after week 20 of pregnancy (2,4,8).
Preeclampsia is one of the major causes of maternal mortality worldwide with a prevalence of 5-10% in all pregnancies (9). Although the exact etiology and pathogenesis of preeclampsia are still elusive, it seems that chronic systemic inflammation resulting from periodontal disease may be an important risk factor. In this regard, the results of some studies revealed that periodontal disease parameters, such as the pocket depth (PD), clinical attachment loss (CAL), plaque index (PI), and bleeding on probing (BOP) are significantly associated with high blood pressure (BP) (10-12). Therefore, it is possible to associate maternal periodontitis with an increased risk of preeclampsia. However, some results are contradictory due to differences in the sample size, sociodemographic characteristics, and heterogeneity in diagnostic criteria used to identify periodontal disease. Accordingly, some scientists have argued that there is no correlation between the parameters of periodontal disease and BP (13,14). Unfortunately, there is limited literature about the association between maternal periodontal disease and preeclampsia in Iranian pregnant women. Therefore, the present study was conducted on pregnant women admitted to Alavi Educational and Medical Center in Ardabil, Iran from September 2019 to March 2020.
Methods
This case-control study was conducted on 80 randomly selected Iranian pregnant women to determine the correlation between maternal periodontal disease and preeclampsia in them. Using simple random sampling, the participants were assigned to experimental groups, including 40 pregnant patients suffering from preeclampsia as the case group and 40 healthy pregnant women as the controls. The sample size was estimated according to the sample size estimation formula (15,16). The inclusion criteria were the age up to 35 years, gestational age of less than 34 weeks, having at least 15 teeth, no history of infection during pregnancy, and no periodontal therapy within six months before pregnancy. The oral hygiene status was scored for all teeth using PI index. Moreover, the participants with a history of diabetes, alcoholism, chronic hypertension, severe tooth decays, collagen diseases, kidney diseases, and the need for antibiotics were excluded from the study.
Periodontal Examination
All the participants underwent a full-mouth periodontal examination by the assessment of PD, CAL, BOP, and PI parameters in all teeth except the third molar and second distal molar teeth. The PI parameter was measured according to O’Leary (17) and the measurements were performed by a calibrated examiner at six sites per tooth (17). In this regard, the CAL index was measured in six points, including mesiobuccal, midbuccal, distobuccal, mesiolingual, midlingual, and distolingual by William’s probe in millimeters. For this purpose, the distance between cementoenamel junctions through the depth of the pocket in the six aforementioned points was measured, and the average for each participant was recorded. Furthermore, the BOP was calculated according to Lenox and Kopczyk (18). The BOP was considered positive if hemorrhage occurred within 30-60 seconds after probing. To evaluate PI, the subjects in both groups were given disclosing tablets (Eviplac, Biodinamica Quim), and the presence of plaque on tooth mesial, distal, buccal, and lingual surfaces was determined (19).
Preeclampsia Diagnosis
The patients suffering from preeclampsia were diagnosed by a gynecologist. According to the definition by the American College of Obstetricians and Gynecologists (ACOG), preeclampsia is defined as sustained pregnancy-induced hypertension (BP≥140/90 mm Hg within 6 hours) with proteinuria (with urine protein concentrations ≥1 mg/dL on a catheterized urine sample) (8).
Statistical Analysis
All the statistical analyses were performed by SPSS software (version 24.0). Since the acquired data had no normal distribution, statistical analysis was carried out using the Mann-Whitney U test for the determination of the significant differences among the seven groups (Table 1). All the data are expressed as mean ± standard error of the mean, and p-values of less than 0.05 were considered as statistically significant.
Table 1.
Normal and Non-Normal Distribution Assessment of the Data
|
Periodontal Parameters
|
Group
|
Average
|
Standard Deviation
|
Skewness
|
Kurtosis
|
| Pocket Depth (mm) |
Control |
1.92 |
0.23 |
0.27 |
1.25 |
| Preeclamptic |
2.95 |
0.51 |
-1.47 |
2.12 |
| Clinical Attachment Loss (mm) |
Control |
0.59 |
0.38 |
-0.48 |
-1.02 |
| Preeclamptic |
1.99 |
1.04 |
2.99 |
15.16 |
| Bleeding on Probing (%) |
Control |
25.17 |
7.16 |
-0.12 |
-0.09 |
| Preeclamptic |
45.12 |
10.45 |
1.93 |
4.98 |
| Plaque Index (%) |
Control |
52.90 |
6.09 |
-1.86 |
4.93 |
| Preeclamptic |
66.25 |
7.04 |
-0.64 |
5.70 |
Results
The present study was carried out on a total of 80 pregnant women, including 40 patients with preeclampsia and 40 normal pregnant subjects. The mean values of participants’ age were reported as 27.87±4.56 and 27.8±4.91 years in the control and preeclamptic groups, respectively (Table 2). None of the subjects in both groups had a history of urinary system infection, chronic hypertension, diabetes, and systemic disease. As shown in Table 2 and Figure 1, there was no significant difference between preeclamptic patients and healthy controls in terms of literacy level, occupation, gestational age, and dental history. In addition, oral hygiene status was evaluated using PI score. According to results, there was a significant difference between the mean PI score of the preeclamptic subjects (58.61) and healthy controls (22.39, P < 0.001). The mean duration values of gestation in the control and preeclamptic groups were reported as 30.70±1.92 and 29.72±2.81 weeks, respectively (Table 2). According to the results, the prevalence of periodontal disease was significantly higher in the preeclamptic group. As shown in Table 3, the quantitative analysis of the periodontal parameters in the experimental groups indicated that mean values of BOP, CAL, PD, and PI were significantly higher in the preeclamptic group compared to those reported for the control group. Furthermore, the number of teeth with periodontitis was significantly greater in the preeclamptic group (P˂ 0.001). The results showed that the amount of BOP was 59.54% in the preeclamptic group, which was significantly higher than that of the control group (21.46%; P < 0.001). Moreover, the periodontal evaluation showed that the CAL ratio in the preeclamptic group (58.86%) was significantly higher than that reported for the control group (22.14%) (P< 0.001). Likewise, the PI significantly increased in preeclamptic group (58.61%) compared to that of the control group (22.39%; P < 0.001). Based on statistical analysis, the PD ratio was also significantly higher in the preeclamptic group (58.04%) in comparison to the ratio in the control group (22.96%; P < 0.001; Table 3). Therefore, the obtained results of the current study demonstrated that pregnant women with periodontal disease were more susceptible to preeclampsia.
Table 2.
Demographic and Medical Characteristics of Preeclamptic and Control Groups
|
Group
|
Maternal Age (y)
Mean ± SD
|
Gestational Age (wk)
Mean ± SD
|
Employed
(n)
|
Dental History
(n)
|
| Control |
27.87±4.56 |
30.70±1.92 |
5 |
38 |
| Preeclamptic |
27.80±4.91 |
29.72±2.81 |
6 |
33 |
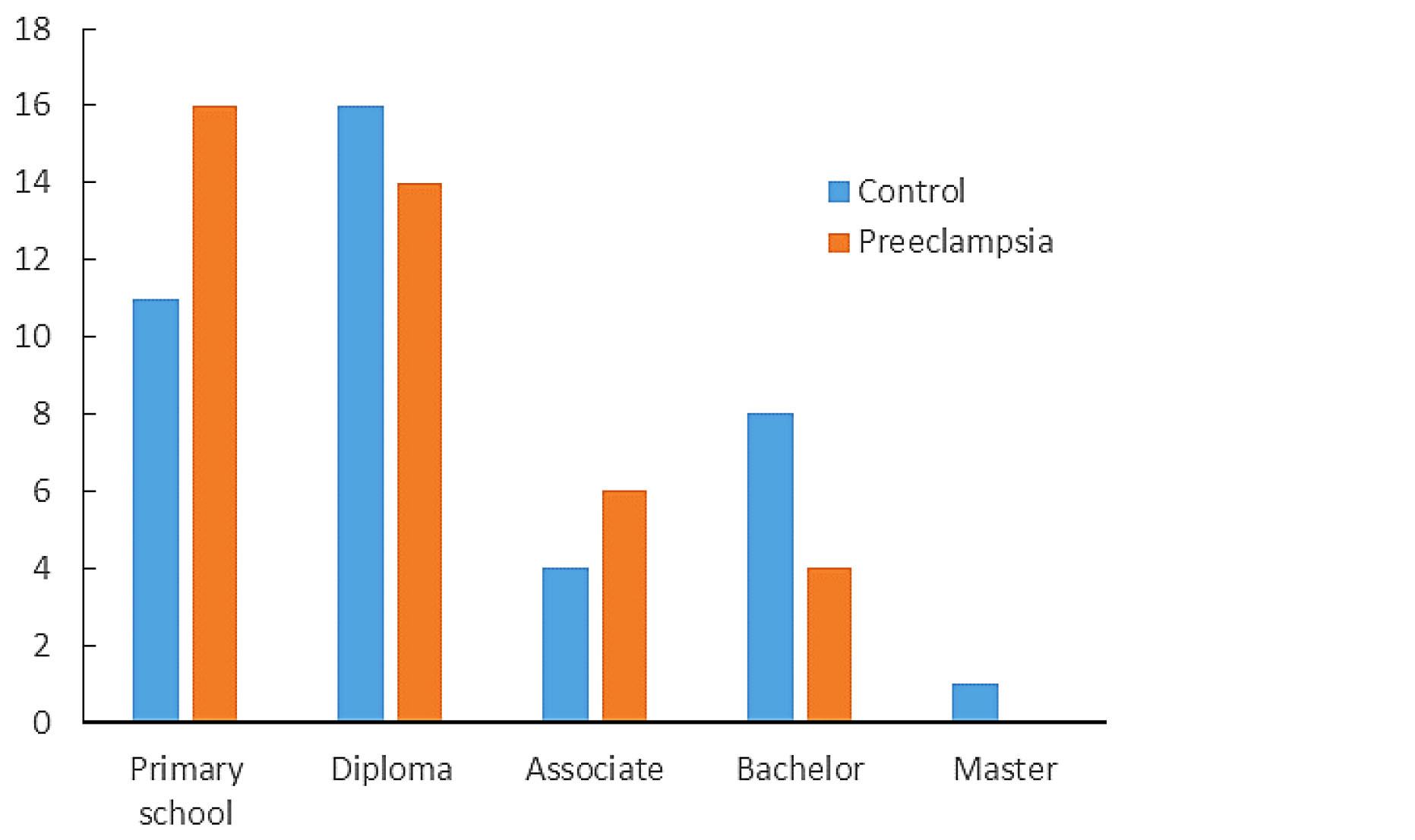
Figure 1.
The Literacy Level of Participants in Preeclamptic and Control Groups.
.
The Literacy Level of Participants in Preeclamptic and Control Groups.
Table 3.
Comparison of Periodontal Parameters Between Preeclamptic and Control Groups
|
Variables
|
Group
|
Average Grade
|
Sum
|
z
|
P
Value
|
| Bleeding on probing |
Control |
21.46 |
858.50 |
-7.33 |
0.001 |
| Preeclamptic |
59.54 |
2381.50 |
| Clinical attachment loss |
Control |
22.14 |
885.50 |
-7.07 |
0.001 |
| Preeclamptic |
58.86 |
2354.50 |
| Pocket depth |
Control |
22.96 |
918.50 |
-6.75 |
0.001 |
| Preeclamptic |
58.04 |
2321.50 |
| Plaque index |
Control |
22.39 |
895.50 |
-6.98 |
0.001 |
| Preeclamptic |
58.61 |
2344.50 |
Discussion
The present study aimed to evaluate the relationship between periodontal disease and the risk of preeclampsia in Iranian women. For this purpose, the association between periodontal disease and the risk of preeclampsia was investigated among 40 preeclamptic pregnant patients and 40 women with normal pregnancy aged up to 35 years and gestational age of less than 34 weeks. Periodontal examination was performed by the measurement of four periodontal disease parameters, including PD, CAL, PI, and BOP. The obtained data demonstrated an association between periodontal disease and preeclampsia. According to our results, periodontal diseases were significantly more severe in pregnant women with preeclampsia compared to those reported for the healthy controls. Although there was no significant difference in literacy level, occupation, gestational age, and dental history between the two groups, PI as oral hygiene index was significantly higher in the preeclamptic women (Table 3, P < 0.001). Moreover, as shown in Table 3, the PD, CAL, and BOP values were significantly higher in the preeclamptic women in comparison with healthy controls (P < 0.001). These findings suggest an association between the maternal periodontitis and an increased risk for preeclampsia. Periodontitis is a chronic inflammatory condition characterized by destruction of the supportive tissues of the teeth, including alveolar bone and periodontal ligament. Accumulation of dental plaque biofilm on the tooth is the most important etiological factor of the periodontal inflammation and destruction (20). Bactria in the dental plaque biofilm as a source of inflammatory mediators, such as interleukins, tumor necrosis factor (TNF), and prostaglandin E2 lead to intensive destruction of periodontal tissues. In addition, the alteration in CD34+ T-cells and some cytokines, such as Th2 has been shown in preeclampsia. The CD34+ T-cells and Th2 cytokine have an important role in attenuation of systemic inflammation and periodontitis. The relationship between periodontitis and preeclampsia may be mediated by maternal systemic inflammation (2,4,20). To support the aforementioned results, Boggess et al, for the first time, showed an association between maternal periodontitis and the risk of preeclampsia among pregnant women in the United States (21). Herrera et al demonstrated that severe periodontitis, but not moderate, may lead to preeclampsia (22). In a study carried out by Ruma et al, a relationship was observed between maternal periodontitis and systemic inflammation as measured by C-reactive protein and risk of preeclampsia (23). Moreover, Shetty et al examined the association between preeclampsia and periodontal disease (i.e., CAL and gingival indices) in 130 Indian pregnant women within 48 hours after delivery. In the aforementioned study, it was suggested that periodontitis can be related to a high risk of preeclampsia (24). Furthermore, Sayar et al demonstrated that preeclamptic women had higher attachment loss and gingival recession than normal pregnant women (25). Varshney and Gautam showed that the amount of gingival inflammation, oral hygiene levels, PD, and CAL were higher in preeclamptic women, indicating that maternal periodontal disease may increase the risk of preeclampsia (26). Moreover, Ha et al confirmed the association between periodontal disease and preeclampsia in Korean women (27,28). Furthermore, Desai et al evaluated PD and CAL in 1240 pregnant women and introduced maternal periodontitis as a risk factor for preeclampsia (16). As mentioned previously, inflammation induces systemic disease and preeclampsia. Consequently, it can be concluded that periodontal diseases during pregnancy can increase the risk of preeclampsia. Therefore, to decrease the risk of preeclampsia, pregnant women should pay more attention to periodontal disease. The relatively small sample size can be considered the limitation of the present study. Although some studies have been carried out on the underlying mechanisms of the effect of periodontal disease on preeclampsia, further studies are needed to confirm and elucidate the precise mechanisms of periodontal disease.
Conclusions
The present study measured periodontal health indices, including PD, CAL, BOP, and PI. Our results showed that periodontal diseases are more severe in pregnant women with preeclampsia compared to those reported for normal pregnant subjects. Therefore, it seems that the maternal periodontitis can be a risk factor for development of preeclampsia.
Conflict of Interest Disclosures
The authors declare that they have no conflict of interests.
Acknowledgements
The authors would like to thank the high-risk department staff of Alavi hospital for assisting with the research process.
Ethical Statement
All the procedures were conducted under the Declaration of Helsinki and guidelines of the Ethics Committee of the Ardabil University of Medical Sciences, Iran (IR.ARUMS.REC.1398.220). The participants were informed about the objective of the study and a written informed consent was obtained from all the participants.
Authors’ Contribution
IF and ZM contributed to study design, data collection, data analysis, results interpretation, and manuscript preparation. RD and ANB contributed to data collection, data analysis, and results interpretation
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Williams RC. Periodontal disease. N Engl J Med 1990; 322(6):373-82. doi: 10.1056/nejm199002083220606 [Crossref] [ Google Scholar]
- Scannapieco FA, Gershovich E. The prevention of periodontal disease-an overview. Periodontol 2000 2020; 84(1):9-13. doi: 10.1111/prd.12330 [Crossref] [ Google Scholar]
- Ide M, Papapanou PN. Epidemiology of association between maternal periodontal disease and adverse pregnancy outcomes--systematic review. J Periodontol 2013; 84(4 Suppl):S181-94. doi: 10.1902/jop.2013.134009 [Crossref] [ Google Scholar]
- Bobetsis YA, Graziani F, Gürsoy M, Madianos PN. Periodontal disease and adverse pregnancy outcomes. Periodontol 2000 2020; 83(1):154-74. doi: 10.1111/prd.12294 [Crossref] [ Google Scholar]
- Loesche WJ, Grossman NS. Periodontal disease as a specific, albeit chronic, infection: diagnosis and treatment. Clin Microbiol Rev 2001; 14(4):727-52. doi: 10.1128/cmr.14.4.727-752.2001 [Crossref] [ Google Scholar]
- Terzieva-Petrovska O, Petrovski M, Minovska A, Papakoca K, Spasov D. Assessment of Risk Factors for Periodontal Diseases Among High School Students in Stip. Tirana, Albania: University Goce Delcev Stip; 2019.
- Genco RJ, Borgnakke WS. Risk factors for periodontal disease. Periodontol 2000 2013; 62(1):59-94. doi: 10.1111/j.1600-0757.2012.00457.x [Crossref] [ Google Scholar]
- ACOG practice bulletin. Diagnosis and management of preeclamps ia and eclampsia Number 33, January 2002 American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet 2002; 77(1):67-75. [ Google Scholar]
- Young BC, Levine RJ, Karumanchi SA. Pathogenesis of preeclampsia. Annu Rev Pathol 2010; 5:173-92. doi: 10.1146/annurev-pathol-121808-102149 [Crossref] [ Google Scholar]
- Pralhad S, Thomas B, Kushtagi P. Periodontal disease and pregnancy hypertension: a clinical correlation. J Periodontol 2013; 84(8):1118-25. doi: 10.1902/jop.2012.120264 [Crossref] [ Google Scholar]
- Machado V, Aguilera EM, Botelho J, Hussain SB, Leira Y, Proença L. Association between periodontitis and high blood pressure: results from the study of periodontal health in Almada-Seixal (SoPHiAS). J Clin Med 2020; 9(5). doi: 10.3390/jcm9051585 [Crossref]
- Gordon JH, LaMonte MJ, Genco RJ, Zhao J, Cimato TR, Hovey KM. Association of clinical measures of periodontal disease with blood pressure and hypertension among postmenopausal women. J Periodontol 2018; 89(10):1193-202. doi: 10.1002/jper.17-0562 [Crossref] [ Google Scholar]
- Castaldi JL, Bertin MS, Giménez F, Lede R. [Periodontal disease: is it a risk factor for premature labor, low birth weight or preeclampsia?]. Rev Panam Salud Publica 2006; 19(4):253-8. doi: 10.1590/s1020-49892006000400005 [Crossref] [ Google Scholar]
- Khader YS, Jibreal M, Al-Omiri M, Amarin Z. Lack of association between periodontal parameters and preeclampsia. J Periodontol 2006; 77(10):1681-7. doi: 10.1902/jop.2006.050463 [Crossref] [ Google Scholar]
- Hazra A, Gogtay N. Biostatistics series module 5: determining sample size. Indian J Dermatol 2016; 61(5):496-504. doi: 10.4103/0019-5154.190119 [Crossref] [ Google Scholar]
- Desai K, Desai P, Duseja S, Kumar S, Mahendra J, Duseja S. Significance of maternal periodontal health in preeclampsia. J Int Soc Prev Community Dent 2015; 5(2):103-7. doi: 10.4103/2231-0762.155734 [Crossref] [ Google Scholar]
- O’Leary TJ, Drake RB, Naylor JE. The plaque control record. J Periodontol 1972; 43(1):38. doi: 10.1902/jop.1972.43.1.38 [Crossref] [ Google Scholar]
- Lenox JA, Kopczyk RA. A clinical system for scoring a patient’s oral hygiene performance. J Am Dent Assoc 1973; 86(4):849-52. doi: 10.14219/jada.archive.1973.0178 [Crossref] [ Google Scholar]
- Pretty IA, Edgar WM, Smith PW, Higham SM. Quantification of dental plaque in the research environment. J Dent 2005; 33(3):193-207. doi: 10.1016/j.jdent.2004.10.017 [Crossref] [ Google Scholar]
- Carrizales-Sepúlveda EF, Ordaz-Farías A, Vera-Pineda R, Flores-Ramírez R. Periodontal disease, systemic inflammation and the risk of cardiovascular disease. Heart Lung Circ 2018; 27(11):1327-34. doi: 10.1016/j.hlc.2018.05.102 [Crossref] [ Google Scholar]
- Boggess KA, Lieff S, Murtha AP, Moss K, Beck J, Offenbacher S. Maternal periodontal disease is associated with an increased risk for preeclampsia. Obstet Gynecol 2003; 101(2):227-31. doi: 10.1016/s0029-7844(02)02314-1 [Crossref] [ Google Scholar]
- Herrera JA, Parra B, Herrera E, Botero JE, Arce RM, Contreras A. Periodontal disease severity is related to high levels of C-reactive protein in pre-eclampsia. J Hypertens 2007; 25(7):1459-64. doi: 10.1097/HJH.0b013e3281139ea9 [Crossref] [ Google Scholar]
- Ruma M, Boggess K, Moss K, Jared H, Murtha A, Beck J. Maternal periodontal disease, systemic inflammation, and risk for preeclampsia. Am J Obstet Gynecol 2008; 198(4):389e1-5. doi: 10.1016/j.ajog.2007.12.002 [Crossref] [ Google Scholar]
- Shetty M, Shetty PK, Ramesh A, Thomas B, Prabhu S, Rao A. Periodontal disease in pregnancy is a risk factor for preeclampsia. Acta Obstet Gynecol Scand 2010; 89(5):718-21. doi: 10.3109/00016341003623738 [Crossref] [ Google Scholar]
- Sayar F, Hoseini MS, Abbaspour S. Effect of periodontal disease on preeclampsia. Iran J Public Health 2011; 40(3):122-7. [ Google Scholar]
- Varshney S, Gautam A. Poor periodontal health as a risk factor for development of pre-eclampsia in pregnant women. J Indian Soc Periodontol 2014; 18(3):321-5. doi: 10.4103/0972-124x.134569 [Crossref] [ Google Scholar]
- Ha JE, Oh KJ, Yang HJ, Jun JK, Jin BH, Paik DI. Oral health behaviors, periodontal disease, and pathogens in preeclampsia: a case-control study in Korea. J Periodontol 2011; 82(12):1685-92. doi: 10.1902/jop.2011.110035 [Crossref] [ Google Scholar]
- Ha JE, Jun JK, Ko HJ, Paik DI, Bae KH. Association between periodontitis and preeclampsia in never-smokers: a prospective study. J Clin Periodontol 2014; 41(9):869-74. doi: 10.1111/jcpe.12281 [Crossref] [ Google Scholar]