Avicenna J Dent Res. 12(3):103-106.
doi: 10.34172/ajdr.2020.21
Original Article
Inferior Sclera Exposure and Maxillary Sagittal Position: Is there any Relationship?
Suleyman Kutalmış Buyuk 1, *  , Ferhat Ayrancı 2
, Ferhat Ayrancı 2  , Esra Genc 3
, Esra Genc 3  , Tugce Imamoglu 3
, Tugce Imamoglu 3 
Author information:
1Associate Professor, Department of Orthodontics, Faculty of Dentistry, Ordu University, Ordu, Turkey.
2Associate Professor, Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Ordu University, Ordu, Turkey.
3Specialist in Orthodontics, Private Practice, Kayseri, Turkey.
4Research Assistant, Department of Orthodontics, Faculty of Dentistry, Ordu University, Ordu, Turkey.
Abstract
Background: Maxillofacial hard and soft tissues play an essential role in the formation of facial aesthetics. The aim of this study was to determine the relationship between inferior scleral exposure and maxillary sagittal position.
Methods: The present study was performed on the lateral cephalometric radiographs and frontal facial photographs of 110 adolescent subjects. The participants were divided into two equal groups according to gender (55 subjects per group). Total eye height and inferior scleral heights were defined, and scleral exposure ratios were calculated on facial photographs. The measurements were performed for right and left eyes, and the mean value for inferior scleral exposure ratio was calculated. Soft and hard tissue measurements of maxilla were performed on lateral cephalometric radiographs. Independent t test, Mann-Whitney U test, and Pearson correlation test were used to analyze the data.
Results: There was no statistical difference between genders in the inferior scleral exposure ratio, NPerp_A, A’_True Vertical Line (TVL), and Upper Lip_TVL parameters (P>0.05). However, maxillary height was greater in male subjects than females (P<0.001). The inferior scleral exposure ratio was statistically significantly correlated with NPerp_A distance in males (r=0.286; P<0.05). However, there was no correlation between other maxillary parameters and inferior scleral exposure ratio in males (P>0.05). The inferior scleral exposure ratio was significantly correlated with maxillary height in females (r=-0.296; P<0.05). However, there was no correlation between other maxillary parameters and inferior scleral exposure ratio in females (P>0.05).
Conclusions: While the inferior scleral exposure ratio was correlated with NPerp_A distance in male adolescents, the inferior scleral exposure ratio was correlated with maxillary height in female adolescents.
Keywords: Orthognathic surgery, Inferior scleral exposure, Lateral cephalometry, Maxillary position
Copyright and License Information
© 2020 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Buyuk SK, Ayrancı F, Genc E, Imamoglu T. Inferior sclera exposure and maxillary sagittal position: is there any relationship?. Avicenna J Dent Res. 2020;12(3):103-106. doi: 10.34172/ajdr.2020.21.
Background
Highlights
-
The inferior scleral region may appear in maxillary retrognathia or insufficiency cases.
-
The inferior scleral exposure ratio was correlated with NPerp_A distance in male adolescents.
-
The inferior scleral exposure ratio was correlated with maxillary height in female adolescents.
Maxillofacial hard and soft tissues play an essential role in the formation of facial aesthetics. The position and symmetry of the periorbital region are substantial in acceptable facial aesthetics (1,2). The periorbital region consists of eye globe, extraocular muscles, eyelids, and surrounding soft tissue. Anatomical relationship between the eye area and soft tissues and eyeballs is of great importance in the aesthetic perception of the middle face region (3). The beauty of periorbital area is ultimately intuitive; however, various common features seem to span racial differences and can be loosely defined (4).
The appearance of the malar region becomes silent, and the appearance of the sclera between the iris and the lower eyelid occurs with the disappearance of the relationship between the eye globe and the surrounding periorbital tissues. The visible part of the eyeball consists of three main components: iris, pupil, and sclera. The inferior sclera should not be visible while the person is in a relaxed and natural head position frontal facial perspective.However, the inferior scleral region may appear in maxillary retrognathia or insufficiency cases. Maxillary orthognathic surgical procedures effect the periorbital region (5,6). The position of the lower eyelids can change after maxillary surgical movements and lead to a change in inferior sclera exposure (7). Exposure of the inferior sclera tends to give the face an elderly appearance and may cause aesthetic concerns (8).
The aim of this study was to determine relationship between the inferior scleral exposure and maxillary sagittal position on lateral cephalometric radiographs and facial frontal photographs.
Materials and Methods
This study was performed on subjects who applied to Department of Orthodontics Faculty of Dentistry Ordu University, Ordu, Turkey, and the research was designed as a retrospective study. Patients with any cranio-facial syndrome, cleft lip and palate, and previous orthodontic and orthognathic surgery treatment were excluded from the study. Subjects with frontal facial photographs, which can easily be measured with the surrounding anatomical structures of the eyes, as well as lateral cephalometric radiographs without simultaneous artefacts were included in this study.
The sample size was calculated based on a power analysis using G*Power (version 3.1.9.2, Universität Düsseldorf, Germany) and a 95% power for maxillary height (effect size d=1.5000000) at 0.05% alpha error probability (9). Power analysis showed that 11 samples were enough for each group, but for more reliable results, measurements were performed on 110 patients (55 males and 55 females). The mean age and vertical dimensions of the individuals included in the study are shown in Table 1.
Table 1.
Demographic Characteristics and Vertical Dimensions of Subjects
|
|
N
|
Age (y)
Mean (SD)
|
SN-GoMe (°)
Mean (SD)
|
| Male |
55 |
16.73 (1.41) |
34.55 (5.48) |
| Female |
55 |
16.77 (1.09) |
34.37 (6.35) |
|
P
|
|
0.874a |
0.558b |
Abbreviation: SD, standard deviation.
a Results of independent t test, b Results of Mann-Whitney U test.
All facial photographs were taken in the natural head position with a standard distance (about 1 m) and focusing on the mid-face area with the digital camera (EOS D300, Canon Inc., Tokyo, Japan). All photographs were enlarged at the same to measure easily on right and left eyes to perform scleral measurements. Three different anatomical points were defined for each eye. Total eye height and inferior scleral heights were defined, and scleral exposure ratios were calculated (Figure 1) (10). The measurements were performed for right and left eyes, and the mean value for inferior scleral exposure ratio was calculated.

Figure 1.
Anatomic Landmarks: (a) upper eyelid margin, (b) inferior limbus, (c) lower eyelid margin, (y) eye height, (x) inferior scleral exposure, (x/y) inferior scleral exposure ratio.
.
Anatomic Landmarks: (a) upper eyelid margin, (b) inferior limbus, (c) lower eyelid margin, (y) eye height, (x) inferior scleral exposure, (x/y) inferior scleral exposure ratio.
Soft and hard tissue measurements of the maxilla were performed on lateral cephalometric radiographs taken on a single radiographic device (Kodak 8000C Digital Panoramic and Cephalometric System, Cephalostat; Corestream Health Inc., Rochester, NY, USA) (Table 2, Figure 2). The measurements were N-Perp A, A’ point distance to TVL, upper lip anterior distance to TVL, and maxillary height on the lateral cephalometric radiographs.
Table 2.
Inferior Scleral Exposure Ratio and Other Maxillary Cephalometric Parameter Values
|
Parameters
|
Male
|
Female
|
P
|
|
Mean (SD)
|
Mean (SD)
|
| Inferior scleral exposure ratio |
0.09 (0.05) |
0.09 (0.04) |
0.888a |
| NPerp_A |
-1.31 (3.63) |
-1.68 (2.95) |
0.566a |
| A’_TVL |
-1.80 (1.75) |
-1.28 (1.18) |
0.075a |
| Upper Lip_TVL |
1.17 (3.39) |
2.25 (2.35) |
0.056a |
| Maxillary height |
24.75 (3.37) |
23.03 (2.65) |
0.001b |
Abbreviation: SD, standard deviation.
aResults of independent t test, bResults of Mann-Whitney U test.
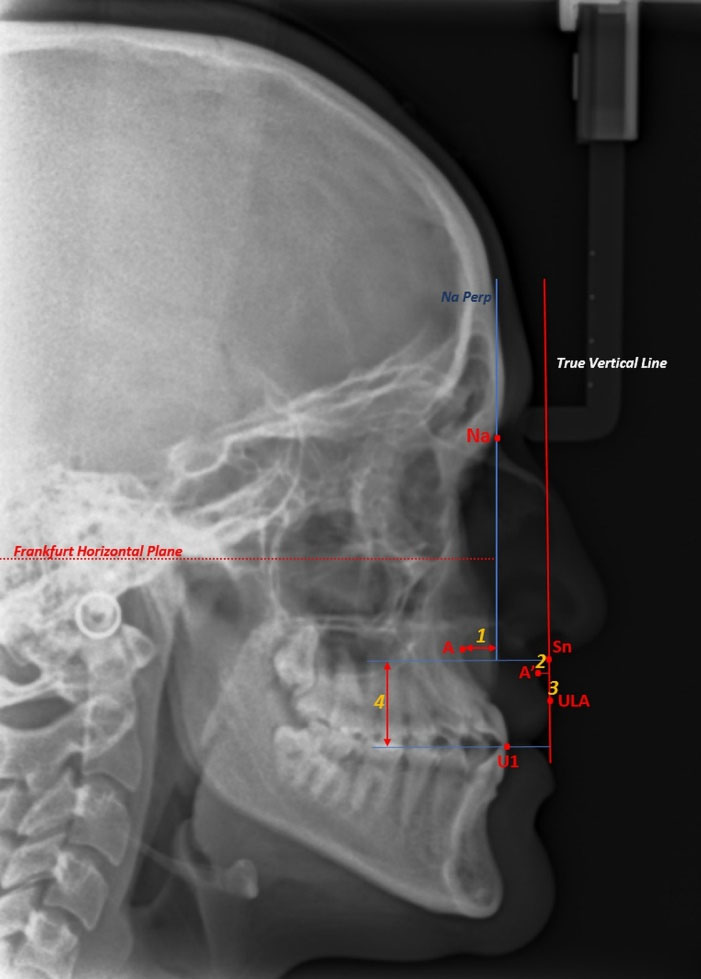
Figure 2.
Maxillary Skeletal and Soft Tissue Measurements. (1) N-Perp A, (2) A’ point distance to TVL, (3) Upper lip anterior distance to TVL, (4) Maxillary height.
.
Maxillary Skeletal and Soft Tissue Measurements. (1) N-Perp A, (2) A’ point distance to TVL, (3) Upper lip anterior distance to TVL, (4) Maxillary height.
All measurements were performed by an experienced orthodontist in cephalometric measurements (E.G.) using the software program (Facad trial version 3.8 software, Ilexis AB, Linkoping, Sweden). In addition, 20% of the photographs and cephalometric radiographs were re-measured by the same researcher after one month and intra-class correlations were performed.
All statistical analyses were performed with statistical software (SPSS for Windows version 20.0 software, IBM Corp., Armonk, NY, USA). The Kolmogorov-Smirnov test was used to evaluate the normal distribution of data to compare scleral and cephalometric measurements between the genders. Independent t test was applied to the normally distributed parameters and Mann-Whitney U test was applied to the non-normally distributed parameters. Moreover, Pearson correlation test was used to determine the relationship between scleral exposure rate and maxillary hard and soft tissue parameters. Moreover, P < 0.05 was considered as statistically significant.
Results
The intra-class correlation coefficients for the maxillary and scleral eye measurements were >0.878. This correlation shows a very high repeatability of the measurements.
The present study was performed on the lateral cephalometric radiographs and frontal facial photographs of 110 adolescent subjects. There was no statistically significant difference between chronological ages and vertical skeletal dimensions (P>0.05) (Table 1).
Comparisons of the genders in terms of inferior scleral exposure ratio and other maxillary cephalometric parameter values were presented in Table 2. There was no statistical difference between genders in the inferior scleral exposure ratio, NPerp_A, A’_TVL, and Upper Lip_TVL parameters (P>0.05). However, maxillary height was found to be greater in male subjects compared to females (P < 0.001) (Table 2).
The inferior scleral exposure ratio was found to be significantly correlated with NPerp_A distance in males (r=0.286; P < 0.05). However, there was no correlation between other maxillary parameters and inferior scleral exposure ratio in males (P>0.05) (Table 3). Moreover, correlations between other maxillary cephalometric parameters in males were presented in Table 3.
Table 3.
Pearson Correlations Between Inferior Scleral Exposure Ratio and Other Maxillary Cephalometric Parameters in Males
|
|
Inferior Scleral Exposure Ratio
|
NPerp_A
|
A’_TVL
|
Upper Lip_TVL
|
Maxillary Height
|
| Inferior scleral exposure ratio |
− |
0.286a |
0.130 |
0.106 |
0.021 |
| NPerp_A |
0.286a |
− |
0.335a |
0.393a |
0.175 |
| A’_TVL |
0.130 |
0.335a |
− |
0.906b |
0.292a |
| Upper Lip_TVL |
0.106 |
0.393a |
0.906b |
− |
0.342a |
| Maxillary height |
0.021 |
0.175 |
0.292a |
0.342a |
− |
The inferior scleral exposure ratio was found to be significantly correlated with maxillary height in females (r=-0.296; P< 0.05). However, there was no correlation between other maxillary parameters and inferior scleral exposure ratio in females (P>0.05) (Table 4). The correlations between other maxillary cephalometric parameters in females were presented in Table 4.
Table 4.
Pearson Correlations Between Inferior Scleral Exposure Ratio and Other Maxillary Cephalometric Parameters in Females
|
|
Inferior Scleral Exposure Ratio
|
NPerp_A
|
A’_TVL
|
Upper Lip_TVL
|
Maxillary Height
|
| Inferior scleral exposure ratio |
− |
0.109 |
-0.051 |
-0.055 |
-0.296a |
| NPerp_A |
0.109 |
− |
0.228 |
0.207 |
0.206 |
| A’_TVL |
-0.151 |
0.228 |
− |
0.852b |
0.287a |
| Upper Lip_TVL |
-0.055 |
0.207 |
0.852b |
− |
0.384b |
| Maxillary height |
-0.296a |
0.206 |
0.287a |
0.384b |
− |
Discussion
The position and symmetry of the eyes play an important role in the aesthetic perception of the face. The inferior sclera should not be visible in the natural and relaxed head position. The appearance of the inferior sclera may result from exophthalmos, senile lower lid laxity, trauma to the eye area, as well as the sagittal position of the maxilla. It is possible to correct the inferior scleral exposure with different treatment alternatives, as well as orthognathic surgery. Some studies reported that maxillary advancement surgical procedures can decrease the inferior scleral exposure (5,6,10-12). The purpose of present study was to determine the relationship between inferior scleral exposure and maxillary sagittal position.
The facial area should be evaluated in detail during orthognathic surgery planning. Clinical evaluation of the periorbital region is important at this stage as much as the maxilla and mandibular structures on the face. The periorbital region should be evaluated comprehensively by performing various measurements both clinically and through photographs in cases requiring orthognathic surgery with midface insufficiency. Clinicians need to inform their patients about changes in the face, and especially in the eye area with 3D virtual surgery planning.
Gulsen et al (13) evaluated the relationship between ocular protrusion and craniofacial structures on lateral cephalometric film, and reported that ocular protrusion did not change with gender, anteroposterior position of the maxilla, and mandibular plane angle, and correlated with several craniofacial parameters. In our study, the inferior scleral exposure ratio was found to be significantly correlated with NPerp_A distance in males. The inferior scleral exposure ratio was found to be significantly correlated with maxillary height in females.
Posnick and Sami (10) reported that Le Fort I maxillary advancement with impaction decreased inferior scleral appearance in 10 long face patients. Magraw et al (11) reported that scleral appearance decreased in patients with Le Fort III osteotomies who underwent maxillary advancement. Soydan et al (5)also reported that Le Fort I osteotomies maxillary advancement with or without impaction decreased the inferior scleral exposure in patients with midface insufficiency and retrognathia. Shafaee Fard et al (14) evaluated the lower eyelid position in patients undergoing Le Fort I osteotomy. All patients were found to have achieved an improved lower eyelid position as a result of maxillary advancement. In addition, all patients achieved a decrease of scleral show. While planning for midface insufficiency orthognathic surgery patients, the relationship between the inferior scleral exposure parameter and the maxilla should be considered for each gender.
Conclusions
While the inferior scleral exposure ratio was correlated with NPerp_A distance in male adolescents, the inferior scleral exposure ratio was correlated with maxillary height in female adolescents. The inferior sclera exposure and its relationship with the maxilla should be evaluated comprehensively in maxillary orthognathic surgery procedures.
Conflict of Interest Disclosures
The authors declare that they have no competing interests.
Ethical Statement
This study was approved by the Clinical Research Ethics Committee of Ordu University (No. 2020/21).
Authors’ Contributions
SKB: conceived the ideas and methodology, interpreted the data, led the writing and editing and final approval of manuscript. FA: conceived the ideas and methodology, interpreted the data and final approval of manuscript. EG: collected the data, conceived the ideas and methodology, led the writing and editing and final approval of manuscript. TI: collected the data, led the writing and editing and final approval of manuscript.
Funding/Support
None.
References
- Gill DS, Lloyd T, East C, Naini FB. The facial soft tissue effects of orthognathic surgery. Facial Plast Surg 2017; 33(5):519-25. doi: 10.1055/s-0037-1606334 [Crossref] [ Google Scholar]
- Mokos ZB, Ćurković D, Kostović K, Čeović R. Facial changes in the mature patient. Clin Dermatol 2018; 36(2):152-8. doi: 10.1016/j.clindermatol.2017.10.006 [Crossref] [ Google Scholar]
- Jelks GW, Jelks EB. The influence of orbital and eyelid anatomy on the palpebral aperture. Clin Plast Surg 1991; 18(1):183-95. [ Google Scholar]
- McCurdy JA Jr. Beautiful eyes: characteristics and application to aesthetic surgery. Facial Plast Surg 2006; 22(3):204-14. doi: 10.1055/s-2006-950179 [Crossref] [ Google Scholar]
- Soydan SS, Bayram B, Sar C, Uckan S. Change in inferior sclera exposure following Le Fort I osteotomy in patients with midfacial retrognathia. J Oral Maxillofac Surg 2014; 72(1):166.e1-5. doi: 10.1016/j.joms.2013.09.025 [Crossref] [ Google Scholar]
- Norouzi A, Chi G, Shafaee Fard S, Sezavar M, Sarkarat F, Rakhshan V. Scleral exposure alterations following Le Fort I osteotomy (with and without maxillary impaction) in skeletal class III patients: a before-and-after clinical trial. J Craniomaxillofac Surg 2018; 46(9):1480-3. doi: 10.1016/j.jcms.2018.06.006 [Crossref] [ Google Scholar]
- Flowers RS. The art of eyelid and orbital aesthetics: multiracial surgical considerations. Clin Plast Surg 1987; 14(4):703-21. [ Google Scholar]
- Hintschich C. Correction of entropion and ectropion. Dev Ophthalmol 2008; 41:85-102. doi: 10.1159/000131075 [Crossref] [ Google Scholar]
- Arnett GW, Jelic JS, Kim J, Cummings DR, Beress A, Worley CM Jr. Soft tissue cephalometric analysis: diagnosis and treatment planning of dentofacial deformity. Am J Orthod Dentofacial Orthop 1999; 116(3):239-53. doi: 10.1016/s0889-5406(99)70234-9 [Crossref] [ Google Scholar]
- Posnick JC, Sami A. Individuals with a long face growth pattern and excess inferior scleral exposure: is there improvement after maxillary (Le Fort I) advancement and vertical shortening?. J Oral Maxillofac Surg 2015; 73(9):1809-15. doi: 10.1016/j.joms.2015.02.016 [Crossref] [ Google Scholar]
- Magraw CB, Garaas R, Shaw A, Phillips C, Turvey TA. Changes in scleral exposure following modified Le Fort III osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol 2015; 120(2):119-24. doi: 10.1016/j.oooo.2015.04.005 [Crossref] [ Google Scholar]
- Tahmasbi S, Meshkini M, Rahimipour K, Namdari M, Mousavi R. Changes in scleral exposure following Le Fort І maxillary advancement or impaction. Oral Maxillofac Surg Cases 2019; 5(4):100108. doi: 10.1016/j.omsc.2019.100108 [Crossref] [ Google Scholar]
- Gulsen A, Uzuner FD, Sibar S. The relationship between ocular protrusion and craniofacial structures. J Craniofac Surg 2019; 30(4):1109-12. doi: 10.1097/scs.0000000000005438 [Crossref] [ Google Scholar]
- Shafaee Fard S, Sezavar M, Sarkarat F, Norouzi A, Yazdani M. Inferior scleral show changes following le Fort I osteotomy in CL III patients with maxillary retrusion. J Craniomaxillofacial Res 2017; 4(2):360-5. [ Google Scholar]