Avicenna J Dent Res. 12(3):93-96.
doi: 10.34172/ajdr.2020.19
Original Article
Evaluation of the Prevalence of Concha Bullosa in Cone-Beam Computed Tomography Images
Nasim Shams 1  , Bahareh Shams 2
, Bahareh Shams 2  , Zahra Sajadi 1, *
, Zahra Sajadi 1, * 
Author information:
1Assistant Professor, Department of Oral and Maxillofacial Radiology, Faculty of Dentistry, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
2Assistant Professor, Department of Periodontics, Faculty of Dentistry, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Abstract
Background: The ostiomeatal complex (OMC) is not a separate anatomical structure although it is a functional unit of structures, including the middle meatus, uncinate process, infundibulum, maxillary sinus ostium, ethmoidal bulla, anterior ethmoid sinus ostium, and frontal recess. Concha bullosa is the pneumatization of the concha, which is one of the most common anatomical variations in the middle turbinate.
Methods: This study was conducted using the cone-beam computed tomography (CBCT) images of 172 patients in the archives of the Department of Oral and Maxillofacial Radiology, Dentistry School, Ahvaz Jundishapur. Patient information including age and gender, presence or absence of concha bullosa, the involved side (left or right), and its type (i.e., extensive, lamellar, and bulbous) were collected in the information form. Finally, the chi-square test (with SPSS, version 22) was used to analyze the data, and P value less than 0.05 was considered statistically significant.
Results: Patients with and without concha bullosa were 39.1 and 41.7 years, respectively, but it was no significant difference in terms of age (P=0.321). Out of 52 patients with concha bullosa, 19 (36.5%) cases were males and 33 (63.5%) of them were females. The prevalence of concha bullosa was higher for the bilateral side (20 patients, 38.5%, P=0.000). The prevalence of bulbuls- and lamellar-shape was nearly the same (32.7% and 30.8%, respectively). Eventually, the extensive shape with 36.5% was more frequent for the shape of concha bullosa (P=0.000).
Conclusions: The prevalence of concha bullosa was high. There was no significant difference in terms of age (P=0.321) and gender (P=0.058) of patients with concha bullosa. The extensive type and the bilateral appearance of concha bullosa were more significant (P=0.000).
Keywords: Cone-beam computed tomography, Concha bullosa, Prevalence
Copyright and License Information
© 2020 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Shams N, Shams B, Sajadi Z. Evaluation of the prevalence of concha bullosa in cone-eeam computed tomography images. Avicenna J Dent Res. 2020;12(3):93-96. doi: 10.34172/ajdr.2020.19.
Background
Highlights
-
The prevalence of concha bullosa was high.
-
There was no significant difference in terms of age and gender of patients awith concha bullosa.
-
The extensive type and the bilateral appearance of concha bullosa were more significant.
The ostiomeatal complex (OMC) or ostiomeatal unit is not a separate anatomical structure although it is a functional unit of structures, including the middle meatus, uncinate process, infundibulum, maxillary sinus ostium, ethmoidal bulla, anterior ethmoid sinus ostium, and frontal recess (1).
Concha bullosa is the pneumatization of the concha, which is one of the most prevalent anatomical variations in the form of pneumatization in the bone of one of the turbinates (Concha) which often manifests itself as the middle turbinate. This anatomical condition can be unilateral or bilateral (2).
Conventional radiographic techniques have a limited value in showing OMC. Computed tomography (CT) is a method of choice for assessing the morphology of the OMC (3). With the recent introduction of cone-beam computed tomography (CBCT), dentists and ear, nose, and throat (ENT) specialists have been better able to diagnose anatomical abnormalities and pathological conditions in the structure of the nasal cavity and the surrounding paranasal sinuses (4). CBCT images provide a high-precision dimension and have a lower dose of radiation and metal artifacts compared to multi-detector computed tomography (MDCT) images. CBCT images have a good quality for viewing and examining paranasal sinuses even at the lowest radiation dose.
The presence of septal deviation and concha bullosa plays a role in the development and spread of chronic sinusitis and prevent mucosal outflow (5). This finding is also associated with frontal and temporal headaches (6). The frequency of concha bullosa has been reported from about 20% to more than 95% in some studies (7,8). The fluctuating frequency of concha bullosa in different studies can be due to racial differences and the size of the study population. CBCT is an appropriate assessment method for studying the anatomical variations of the OMC and has led to early diagnosis and appropriate treatment following early diagnosis (9). Accordingly, the present study examined the prevalence of concha bullosa in CBCT images in people who referred to Ahvaz Jundishapur University of Medical Sciences.
Materials and Methods
In this descriptive cross-sectional study, the study population was selected by the convenience sampling method, including people referring to the Dental Radiology Department of Ahvaz Jundishapur University of Medical Sciences between August 2018 and August 2019. The study sample consisted of 172 patients in the age range of 10-70 years (2), collected from the archive. CBCT images were produced by NewTom VGI (Verona, Italy) under 110 kVp, 0.65-3.29 mA, and with an exposure time of 3.6-5.4 seconds. All images were evaluated by NNT Viewer software (NewTom, Verona, Italy), version 3.00. The images were independently evaluated by two maxillofacial radiologists although consensus was reached in different cases.
All patients within the age range 10-70 years and having a proper quality image were considered in this study. The patients with a previous history of rhinoplasty, and/or malignant and benign diseases (polyposis masses) in the sinus nasal area were extruded from the study (3).
All CT images on the monitor (Philips 202EL2SB, 20 inches) in the axial section were examined for the presence and type of the pneumatization of the middle concha (concha bullosa) by oral and maxillofacial radiologists. Concha bullosa types were divided into three groups of bulbous (The pneumatization of the onion-shaped part of the middle concha, Figure 1A), lamellar (The pneumatization of the lamellar (base) part of the middle concha, Figure 1B), and extensive (The pneumatization of both the lamellar and bulbous parts of the middle conical, Figure 1C) according to (3). Descriptive statistics such as the mean, standard deviation, and the frequency and the percentage table were used to present the data. In addition, the Chi-square test and independent t-test were performed by SPSS (version 22) and a P value less than 0.05 was considered statistically significant.
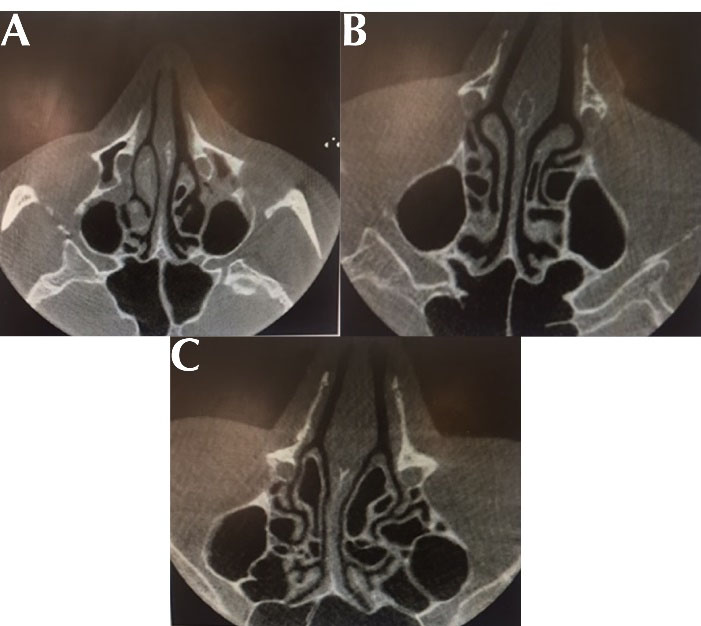
Figure 1.
(A) Bulbous-Type, (B) Lamellar-Type and (C) Extensive-Type Concha Bullosa in CBCT Axial Section. Note. CBCT: Cone-beam computed tomography.
.
(A) Bulbous-Type, (B) Lamellar-Type and (C) Extensive-Type Concha Bullosa in CBCT Axial Section. Note. CBCT: Cone-beam computed tomography.
Results
The collected data were analyzed statistically from all 172 patients, 52 (30.2%) cases had concha bullosa while 120 (69.8%) of them did not have concha bullosa; Therefore, the prevalence of concha bullosa in these patients was 30.2%. According to the data in Table 1, the mean age in patients with and without concha bullosa was 39.1 and 41.7 years, respectively. Patients with concha bullosa were younger compared to those without concha bullosa, but it was no significant difference (P = 0.321) between the two groups regarding age (Table 1).
Table 1.
Prevalence of Concha Bullosa in Age-Based Cone-Beam Computed Tomography Radiographs
|
|
With Concha Bullosa
|
Without Concha Bullosa
|
Total
|
P
Value
|
|
Mean
|
Standard Deviation
|
Mean
|
Standard Deviation
|
Mean
|
Standard Deviation
|
| Age |
39.1 |
15.3 |
41.7 |
15.9 |
40.9 |
15.7 |
0.321 |
As shown in Table 2, out of 172 studied patients, 75 (56.4%) cases were males and 97 (43.6%) of them were females. Out of 52 patients with concha bullosa, 19 (36.5%) and 33 (63.5%) cases were males and females, respectively, indicating a higher prevalence of concha bullosa in women. Of the 120 patients with no concha bullosa, 56 (46.7%) and 64 (53.3%) of them were males and females, respectively. Chi-square test results showed no significant difference in terms of gender between patients with and without concha bullosa (P>0.05).
Table 2.
Frequency for the Gender of Different Types of Concha Bullosa
|
|
With Concha Bullosa
|
Total
|
P
Value
|
|
Bulbous-Shape
|
Lamellar-Shape
|
Extensive-Shape
|
| Gender |
Female |
Number |
15 |
9 |
9 |
33 |
0.058 |
| Percent |
28.9 |
17.3 |
17.3 |
63.5 |
| Male |
Number |
2 |
7 |
10 |
19 |
| Percent |
3.8 |
13.5 |
19.2 |
36.5 |
The data on the frequency of the side of different types of concha bullosa are provided in Table 3. The prevalence of concha bullosa was higher for the bilateral side (20 patients, 38.5%, P = 0.000). Based on the results, the prevalence of bulbuls- and lamellar-shape was approximately the same (32.7% and 30.8%, respectively). Finally, the extensive shape with 36.5% was more frequent for the shape of concha bullosa (P = 0.000).
Table 3.
Frequency for the Side of Different Types of Concha Bullosa
|
|
The Side of Concha Bullosa
|
Total
|
P
Value
|
|
Bulbous-Shape |
Lamellar-Shape
|
Extensive-Shape
|
| Right |
Number |
7 |
5 |
4 |
16 |
0.000 |
| Percent |
13.5 |
9.6 |
7.7 |
30.8 |
| Left |
Number |
6 |
4 |
6 |
16 |
| Percent |
11.5 |
7.7 |
11.5 |
30.7 |
| Left & Right |
Number |
4 |
7 |
9 |
20 |
| Percent |
7.7 |
13.5 |
17.3 |
38.5 |
Discussion and Conclusion
Concha bullosa, which is one of the most common anatomical variations, often manifests itself as pneumatization inside the bone of one of the turbines (Concha), often the middle turbinate. This anatomical condition can be of unilateral or bilateral type (2).
Conventional radiographic techniques have limited values in examining this site. CT is a method of choice for assessing the morphology of the OMC (3). The recent introduction of CBCT has facilitated the diagnosis of anatomical abnormalities and pathological conditions in the structure of the nasal cavity and the surrounding paranasal sinuses for dentists and ENT specialists (4). CBCT images provide a high-detail, high-precision view and have lower radiation doses and metal artifacts compared to MDCT images. CBCT images are of good quality for viewing and assessing paranasal sinuses even at the lowest radiation dose. This descriptive cross-sectional study was performed retrospectively using the CBCT images of 172 patients, including 75 males and 97 females. After examining the images, concha bullosa was observed in 30.2% of patients, which was more in women than men, but there was no significant difference in this regard. The age of people with concha bullosa was lower compared to those without concha bullosa although there was no significant difference in this respect. Concha bullosa cells were more bilateral and extensive and there was a significant difference in this regard.
Abesi et al (8) in their study in Iran concluded that concha bullosa was one of the most common variations of paranasal sinuses mostly reported bilaterally in images, which is consistent with the bilateral prevalence in the present study.
In addition, Hatipoğlu et al (3) reported a prevalence of 70.58% for concha bullosa while the prevalence of concha bullosa in the present study was 30.2%. In the above-mentioned study, 76 patients with the symptoms of sinusitis and headache were included, while the presence of clinical symptoms was not considered in this study and the difference in prevalence is probably due to differences in the type of samples.
Smith et al (10) found a concha bullosa prevalence of 67.5%, which is higher than that of the present study. This difference can be attributed to the higher sample size and the racial differences of the studied populations.
Based on the results of Kucybała et al (11), the prevalence of concha bullosa was 42.1%, which is almost consistent with the result of the present study (30.2%), which can be due to the almost identical sample size and the applied sampling method.
In their study, Budu et al (2) reported a higher prevalence of concha bullosa in women than men, which corroborates with the finding of the present study. They also concluded that concha bullosa was the most common finding (63.67%) among patients with the pathological findings of OMC. The samples of the present study were evaluated from the archive without considering the pathological symptoms, which could indicate a difference in the prevalence percentage obtained in the above-mentioned study.
Hatipoğlu et al (3) showed the prevalence of concha bullosa frequently on the right while in the present study, it was frequently of bilateral type. They reported the most common type of concha bullosa, which is in line with the result of the present study.
Based on the report by Kalabalık et al (12), the prevalence of concha bullosa in Turkey in 2018 was 52.8% and it was frequently of bilateral type. Among unilateral cases, the most common form of concha bullosa was the lamellar type. In the present study, subjects with concha bullosa were frequently of bilateral and extensive type.
In some studies (3,10,11), CT scan images were used for examinations. In a recent study, CBCT images were used, which in addition to providing images with the same quality as CT, imposes a lower dose on the patient, which is one of the strengths of the research.
Our analyses revealed that the prevalence of concha bullosa was significantly high and there was no significant difference among the patients in terms of gender. Concha bullosa cells were frequently of extensive-shaped, bilateral type. According to our analysis, there was a significant relationship between concha bullosa and the site of involvement and the appearance of concha bullosa. People with concha bullosa were younger than those without concha bullosa, but there was no significant difference in this regard.
Conflict of Interest Disclosures
The authors declare that they have no conflict of interests.
Acknowledgments
This study was part of an MD thesis submitted by Zahra Sajadi. This research was financially supported by the Vice-chancellor for the Research Affairs of Ahvaz Jundishapur University of Medical Sciences (grant No. U-98134).
Ethical Statement
This study was approved by the Research Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (Code: IR.AJUMS.REC.1398.480).
Authors’ Contribution
Design of the work: NS, BS. Data collection: NS, ZS. Data analysis and interpretation: NS, BS. Drafting the article: NS, BS, and ZS. Critical revision of the article: NS and BS.
Funding
The costs of this project were supported by Ahvaz Jundishapur of University of Medical Sciences.
References
- Som PM, Curtin HD. Head and Neck Imaging. 15th ed. Elsevier; 2011.
- Budu V, Schnider A, Tache MS, Bulescu I. Evaluation of ostiomeatal complex pathology related to endoscopic sinus surgery–a retrospective analysis. Romanian J Rhinol 2015; 5(18):95-100. doi: 10.1515/rjr-2015-0011 [Crossref] [ Google Scholar]
- Hatipoğlu HG, Cetin MA, Yüksel E. Concha bullosa types: their relationship with sinusitis, ostiomeatal and frontal recess disease. Diagn Interv Radiol 2005; 11(3):145-9. [ Google Scholar]
- Bolger WE, Butzin CA, Parsons DS. Paranasal sinus bony anatomic variations and mucosal abnormalities: CT analysis for endoscopic sinus surgery. Laryngoscope 1991; 101(1 Pt 1):56-64. doi: 10.1288/00005537-199101000-00010 [Crossref] [ Google Scholar]
- White SC, Pharoah MJ. Oral Radiology: Principles and Interpretation. 7th ed. St. Louis: Mosby/Elsevier; 2014.
- Aktas D, Kalcioglu MT, Kutlu R, Ozturan O, Oncel S. The relationship between the concha bullosa, nasal septal deviation and sinusitis. Rhinology 2003; 41(2):103-6. [ Google Scholar]
- Aramani A, Karadi RN, Kumar S. A study of anatomical variations of osteomeatal complex in chronic rhinosinusitis patients-CT findings. J Clin Diagn Res 2014; 8(10):KC01-4. doi: 10.7860/jcdr/2014/9323.4923 [Crossref] [ Google Scholar]
- Abesi F, Haghanifar S, Khafri S, Montazeri A. The evaluation of the anatomical variations of osteomeatal complex in cone beam computed tomography images. J Babol Univ Med Sci 2018; 20(4):30-4. doi: 10.18869/acadpub.jbums.20.4.30 [Crossref] [ Google Scholar]
- Friedrich RE, Fraederich M, Schoen G. Frequency and volumetry of infraorbital ethmoid cells (Haller cells) on cone-beam computed tomograms (CBCT) of the mid-face. GMS Interdiscip Plast Reconstr Surg DGPW 2017; 6:Doc07. doi: 10.3205/iprs000109 [Crossref] [ Google Scholar]
- Smith KD, Edwards PC, Saini TS, Norton NS. The prevalence of concha bullosa and nasal septal deviation and their relationship to maxillary sinusitis by volumetric tomography. Int J Dent 2010;2010. 10.1155/2010/404982.
- Kucybała I, Janik KA, Ciuk S, Storman D, Urbanik A. Nasal septal deviation and concha bullosa-do they have an impact on maxillary sinus volumes and prevalence of maxillary sinusitis?. Pol J Radiol 2017; 82:126-33. doi: 10.12659/pjr.900634 [Crossref] [ Google Scholar]
- Kalabalık F, Tarım Ertaş E. Investigation of maxillary sinus volume relationships with nasal septal deviation, concha bullosa, and impacted or missing teeth using cone-beam computed tomography. Oral Radiol 2019; 35(3):287-95. doi: 10.1007/s11282-018-0360-x [Crossref] [ Google Scholar]