Avicenna J Dent Res. 12(4):136-141.
doi: 10.34172/ajdr.2020.27
Original Article
Prevalence and Anatomic Characteristics of Accessory Mental Foramen Using ConeBeam Computed Tomography Views in an Iranian Population
Marouf Noruzi 1  , Maryam Mostafavi 1, Aysan Ghaznavi 1, Amir Ardalan Abdollahi 2, *
, Maryam Mostafavi 1, Aysan Ghaznavi 1, Amir Ardalan Abdollahi 2, * 
Author information:
1Assistant Professor, Department of Oral and Maxillofacial Radiology, School of Dentistry, Urmia University of Medical Sciences, Urmia, Iran.
2Assistant Professor, Department of Endodontics, School of Dentistry, Urmia University of Medical Sciences, Urmia, Iran.
*
Correspondence to Amir Ardalan Abdollahi Tel: +98-914 409 13 17, Fax: +98 413 334 69 77, Email:
ardalan_2000a@yahoo.com
Abstract
Background: Determining the incidence and anatomic features of accessory mental foramen (AMF) in the Iranian population is of vital importance. This study investigated the prevalence and anatomic characteristics of AMF using cone-beam computed tomography (CBCT) in a selected Iranian population.
Methods: A total of 853 CBCT images from 440 women and 413 men were examined in this cross-sectional retrospective study. The images were evaluated by two independent observers using reconstructed 3-dimensional, cross-sectional, and panoramic views. Several parameters were assessed, including the location of AMF relative to mental foramen (MF), size and the point of canal bifurcations, and the distance between the main and accessory canals. Finally, statistical differences in the AMF prevalence in terms of gender and direction and its location were evaluated by the Mann-Whitney U test (P<0.05).
Results: The prevalence of AMF was 10.55%, which was more frequently located in the posterior inferior area relative to the main MF, and its nerve was more frequently originated from the anterior loop (P=0.001). There were no statistically significant differences in gender (P=0.26) and direction (P=0.4). The mean distance of AMF was 7.62 mm. The mean height of MF and the AMF vertical height were 13.65 mm and 52.12 mm in those with AMF on one side, respectively, and this difference was statistically significant (P=0.001). The sizes of the MF and AMF were 3.2 mm (large diameter), 2.3 mm (small diameter), and 1.4 mm (large diameter), and 1.1 mm (small diameter), respectively.
Conclusions: Based on the findings of the present study, the prevalence of AMF according to hemi-mandibular was 5.80% in the selected Iranian population. Thus, AMF might branch from any section of the inferior alveolar nerve and the mandibular canal.
Keywords: Cone-beam computed tomography, Mental foramen, Prevalence
Copyright and License Information
© 2020 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Noruzi M, Mostafavi M, Ghaznavi A, Abdollahi AA. Prevalence and anatomic characteristics of accessory mental foramen using cone-beam computed tomography views in an iranian population. Avicenna J Dent Res. 2020;12(4):136- 141. doi: 10.34172/ajdr.2020.27.
Background
Highlights
-
Sensible prevalence of accessory mental foramen (AMF) was observed in a selected Iranian population.
-
Anatomic features of AMF should be considered before any mandibular surgical procedures.
-
AMF might branch from any section of the inferior alveolar nerve and mandibular canal.
The mental foramen (MF) is a two-sided anatomic landmark, located on the buccal surface of the mandibular body in the approximate region of premolar teeth, which is the outlet of the mental branch of the inferior alveolar nerve and artery (1). The position of MF in radiographic images varies from the mesial region of the first premolars to the mesial area of the first molars. In addition, it differs in various races (2). Moreover, a knowledge of the MF position could be useful in local anesthesia injections, periapical and orthognathic surgeries, and implant surgeries, as well as the treatment of mandibular fractures, and removal of cysts and pathologic lesions in the clinical practice (1,3).
Accessory mental foramen (AMF) could be defined as any additional foramen on the buccal surface of the mandible except for MF, which is related to the mandibular canal (4) Given that elements passing the AMF are the same as the main MF, knowing about the AMF position is as important as that of the main foramen in the dental practice with particular importance in local anesthesia and surgical procedures involving the region, including genioplasty, mandibular rehabilitation after the trauma, bone harvesting from the chin, and the root resection of mandibular premolars (5,6).
Conventional radiographs in the dental practice (e.g., periapical and panoramic) often fail to show MF anatomic variations since the long axis of AMF is <1.5 mm and the diagnosis of the presence and the position of this structure is extremely difficult using two-dimensional (2-D) radiographs (7). However, cone-beam computed tomography (CBCT) provides 3-D data with high details in dentofacial structures, which allows accurate presurgical assessments (8,9). Considering that AMF has been reported to have the ethnic variations of the incidence and anatomic features (10-12), this study was undertaken to evaluate the prevalence and anatomic characteristics of AMF using the CBCT technique in a sample of Iranian patients.
Methods
A cross-sectional retrospective study of CBCT images of 915 patients was carried out in the imaging centers of several specialists in Urmia, Iran. These mandibular CBCT images were taken during 2010-2017 and were matched based on the inclusion criteria (i.e., the lack of technical errors, visible lower jaw, and observable MF). On the other hand, the exclusion criteria consisted of the presence of pathological and developmental lesions in the apical region of premolars and MF, severe resorption and the fractures of the mandible, and supernumerary or impacted teeth in the MF region. According to inclusion and exclusion criteria, the final sample group included 853 patients (413 males and 440 females). The scans were provided using a CBCT machine (Planmeca, Helsinki, Finland). Radiographic parameters (Kvp, mA) were automatically determined from the scout views by the Planmeca. The exposure parameters were 90 Kvp and other parameters were selected according to the patient’s size, gender, and age. The thickness and interval of cross-sectional views were 1 mm and 2 mm, respectively. The data were saved using the Romexis 3.8.2 software.
The samples were visually evaluated by two independent oral and maxillofacial radiologists, and any disagreement between them was discussed until reaching a consensus. To determine reproducibility, the two observers re-examined 20% of the randomly selected CBCT scans 4 weeks after the first evaluation, and inter-intra observer reliability was confirmed by determining the inter-class coefficient. For the final analysis, each measurement was performed twice. Finally, the provided data by both investigators were averaged, and mean values were calculated accordingly. The CBCT scans were observed in a room with an optimal light without reflection using a 14-inch monitor (HP ProBook 4540s, Houston, USA). The scans were observed from different 3-D cross-sectional and axial views (Figure 1).
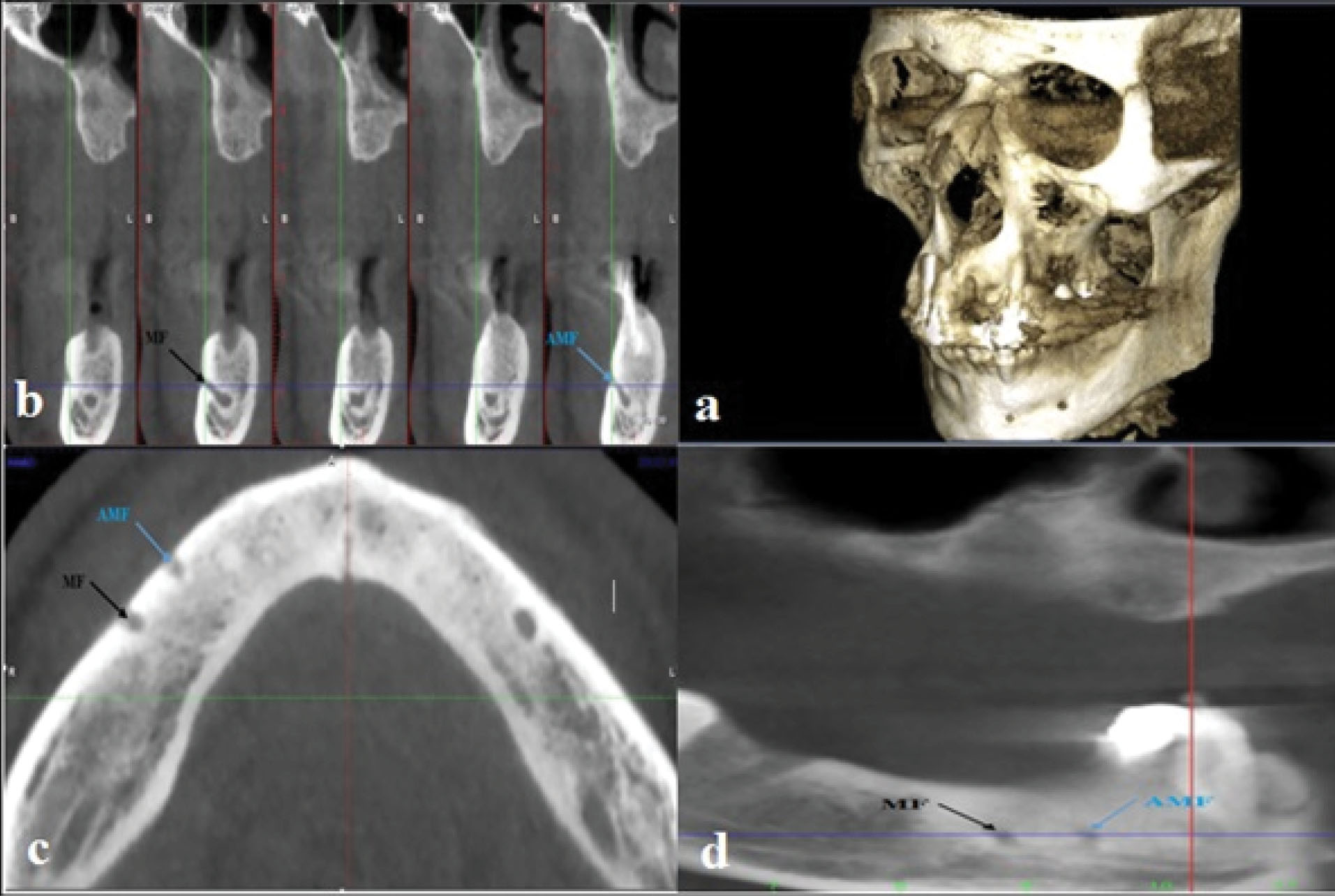
Figure 1.
Images From Different 3-D Cross-sectional and Axial Views. Note. (a) 3-D view, (b) Cross-sectional view, (c) Axial view, and (d) The reconstructed panoramic view showing the location of the separation and connection of both mental foramen and accessory mental foramen with the mandibular canal.
.
Images From Different 3-D Cross-sectional and Axial Views. Note. (a) 3-D view, (b) Cross-sectional view, (c) Axial view, and (d) The reconstructed panoramic view showing the location of the separation and connection of both mental foramen and accessory mental foramen with the mandibular canal.
The scans were evaluated for AMF, which was continuous with the mandibular canal. In scans with available AMF, several steps were taken after considering the patient’s gender. First, the number of AMFs (one, two, three, or more) and later, laterality (one- or two-sided) and the side with extra foramen (left, right, or both) were recorded as well (Figure 2). Then, to determine the position of AMF relative to MF, a hypothetical coordinate axis originating from the MF’s center and x-axis parallel to the occlusal plane was considered and the position of AMF according to the location on the hypothetical coordinate axis was recorded as upper, lower, anterior, posterior, upper posterior, lower posterior, upper anterior, and lower anterior. Next, the site of AMF connection with the mandibular canal was detected by assessing axial and coronal cross-sectional views and recorded as three groups of connection with the anterior branch of the mandibular canal, anterior loop connection, and connection with the mandibular canal. Further, for the measurement of MF and AMF dimensions, considering an approximate circle or elliptical shape, large and small diameters were determined on the axial and cross-sectional images, and the drawn lines were confirmed on the reconstructed panoramic radiograph. The canal with the larger area was considered as MF. The area of canals was calculated according to the following formula:
A= ((a/2*b/2))*pi (A = Area, a = Major diameter, and b = Minor diameter)
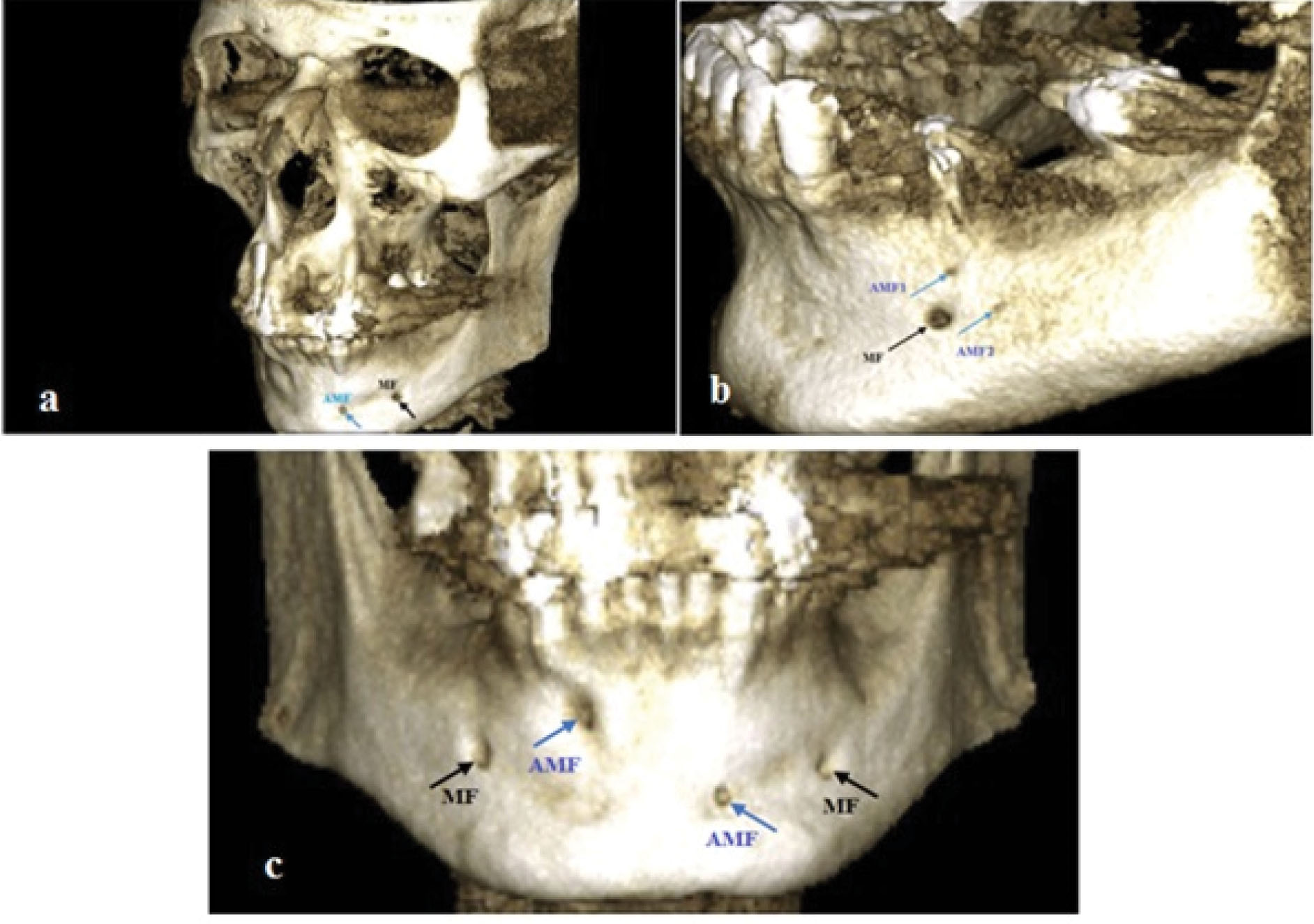
Figure 2.
Variations of the Number and Side of AMF. Note. AMF: Accessory mental foramen; (a) The existence of one one-sided AMF, (B) Two one-sided AMFs, and (c) One two-sided AMF.
.
Variations of the Number and Side of AMF. Note. AMF: Accessory mental foramen; (a) The existence of one one-sided AMF, (B) Two one-sided AMFs, and (c) One two-sided AMF.
Furthermore, the ratio of the AMF area to MF was taken into consideration. The distance between the MF and AMF was computed according to the formula suggested by Naitoh et al (13) (Distance = √(x2+y2)), in which x and y stand for vertical and horizontal distances (8) The vertical distance of MF relative to the inferior border of the mandible on the side with or without AMF was measured by specifying the distance between the inferior region of the osseous cortex of each foramen and the inferior border of the mandible. The prevalence of AMF was determined according to hemimandibular considering each quadrant as an independent unit.
Statistical Analysis
Data were analyzed with descriptive statistics (i.e., means and standard deviations) and Mann-Whitney U test for the prevalence of AMF in relation to gender or direction and its location using SPSS software, version 17 (SPSS version 17.0, SPSS, Chicago, IL, USA). Statistical significance was set at P < 0.05.
Results
In this study, inter-intra observer reliability was confirmed using the inter-class coefficient (0.8). A total of 90 (10.55%) patients (50 males and 40 females) exhibited the AMF on CBCT images. The prevalence of AMF according to hemi-mandibular was 99 (5.80%) of overall 1706 cases. The incidence of the existing AMF on the left and right sides was 48 (5.63%) and 51 (5.98%), respectively. Considering each half jaw as an independent unit, data analysis showed no significant difference in the prevalence of AMF between the left and right sides (P = 0.83).
Table 1 provides the frequencies of AMF. The highest frequency was found in cases with one AMF.
Table 1.
The Frequencies of AMF and its Laterality
|
Groups
|
Number
|
Laterality
|
|
One-Sided
|
Two-Sided
|
| One AMF |
73 |
73 |
0 |
| Two AMF |
16 |
8 |
8 |
| Three AMF |
1 |
0 |
1 |
| Total |
90 |
81 |
9 |
Note. AMF: Accessory mental foramen.
Of 865 patients, 81 cases had one or two AMF(s) on the right or left sides. AMF was found on the right and left sides in 42 and 39 cases, respectively. In addition, the AMF was found on both sides in 9 patients. According to the results, the prevalence of AMF in men was higher compared to women in both one-sided variants with one or two AMF(s) although the difference was not statistically significant (P = 0.26). Moreover, about the cases with AMFs on both sides, the prevalence in women was not statistically more compared to men (P = 0.26).
The Position of Accessory Mental Foramen
Overall, the most prevalent position of AMF was the inferior-posterior in relation to MF. In general, 73 out of 90 patients had one AMF on the right (39 cases) and left (34 cases) sides. In addition, the results of the evaluation of the AMF position in relation to MF in cases with one AMF showed that the most prevalent position of AMF was inferior-posterior, followed by anterior-inferior and upper positions.
Furthermore, of 9 cases exhibiting two or three AMFs, one case had two AMFs on the left side and one AMF on the right side, and 8 cases had one AMF on each side. Additionally, the results demonstrated that in cases with AMF on one of the sides exhibiting it in the anterior or posterior position of MF, the same position could be expected on the opposite side. Moreover, of 8 patients with two AMFs on one side, 3 cases represented it on the right side and 5 cases showed it on the left side. Further, it was observed that the anterior-posterior positions of the two foramina in relation to MF could be the same in cases with 2 AMFs on one side.
Table 2 presents the results regarding the location of the accessory mental nerve (AMN) branching from the inferior alveolar nerve. The results of statistical analyses revealed that AMN branching most commonly occurred in the anterior loop, and the relation of AMF with the anterior loop was significantly greater compared to other situations (P = 0.001). However, 6 cases of AMF originated directly from the mandibular canal.
Table 2.
Location of AMF Branching From the Inferior Alveolar Canal
|
Location of AMF Branching From the Inferior Alveolar Canal
|
Prevalence (N)
|
Prevalence (%)
|
| Anterior loop of the inferior alveolar canal |
76 |
70.37 |
| Anterior branch of the inferior alveolar canal |
26 |
24.07 |
| Inferior alveolar canal (behind the anterior loop) |
6 |
5.55 |
| Total |
108 |
100 |
Note. AMF: Accessory mental foramen; AMN: Accessory mental nerve.
The measurement results of the MF height are presented in Table 3. There was a statistically significant difference in the heights of MF and AMF in cases with one AMF on one side (P = 0.001) and MFs were closer to the alveolar bone in these cases in comparison to AMFs. However, no significant difference was found between the vertical heights of foramina from the inferior border of the mandible in other cases.
Table 3.
The Heights of MFs and AMFs (mm)
|
|
Number
|
Maximum
|
Minimum
|
Mean
|
SD
|
| Height of MF on the side without AMF |
81 |
18.89 |
5 |
13.64 |
2.51 |
| Height of MF in cases with one AMF (one-sided) |
73 |
22.72 |
8.65 |
13.66 |
2.43 |
| Height of AMF in cases with one AMF (one-sided) |
73 |
22.51 |
3.31 |
12.54 |
3.53 |
| Height of MF in cases with two AMFs (two-sided) |
8 |
15.85 |
7.48 |
13.04 |
2.54 |
| Height of AMF in cases with two AMFs (two-sided) |
8 |
20.74 |
6.65 |
13.21 |
4.82 |
| Height of MF on the side without AMF in cases with AMF (one-sided) |
8 |
16.41 |
9.23 |
13.29 |
2.19 |
| Height of MF on the side with AMF in cases with AMF (one-sided) |
8 |
16.6 |
9.52 |
13.65 |
2.24 |
| Height of large AMF on the side with AMF in cases with two AMFs (one-sided) |
8 |
18.3 |
9.22 |
12.33 |
2.77 |
| Height of small AMF on the side with AMF in cases with two AMFs (one-sided) |
8 |
19.4 |
6 |
12.29 |
4.61 |
Note. MF: Mental foramens; AMF: Accessory mental foramens; SD: Standard deviation.
Table 4 summarizes the results of the diameters and areas of MF and AMF in patients with only one one-sided AMF. The ratio of the AMF area to MF was 0.26±0.27. The statistical analysis showed significant differences between large and small diameters in both MF and AMF (P < 0.05), indicating that the shapes of MF and AMF tend to be more elliptical than circular. In addition, there was only a significant difference between small and large diameters in the small AMF (P = 0.03) in patients with two AMFs on one side. In these cases, the large and small AMFs were circular and elliptical, respectively.
Table 4.
Diameters and Areas of MF and AMF Canals in Cases With One-Sided AMF
|
|
MF
|
AMF
|
|
Large Diameter (mm)
|
Small diameter (mm)
|
A*
(mm
2
)
|
Large Diameter (mm)
|
Small Diameter (mm)
|
A*
(mm
2
)
|
| Maximum |
5.71 |
5.4 |
23.3 |
3.46 |
2.5 |
4.9 |
| Minimum |
1.64 |
0.88 |
1.4 |
0.2 |
0.2 |
0.03 |
| Mean |
3.20 |
2.58 |
7.08 |
1.39 |
1.07 |
1.29 |
| SD |
0.98 |
0.93 |
4.79 |
0.60 |
0.39 |
0.90 |
Note. MF: Mental foramens; AMF: Accessory mental foramens; SD: Standard deviation; A*= (a/2*b/2) *pi; A: Area; a: Large diameter; b: Small diameter.
The mean distance between MF and AMF according to the formula (√(x2+y2)) was 6.16±1.66 mm. The measurements of the distance between MF and AMF in patients with one AMF on each side represented no significant difference between the right and left sides (P = 0.4). Based on the results, changes in the position of AMF were more than that of MF. Further, there was no significant difference in the distance of MF from the small and large AMFs in cases with two AMFs on one side (P = 0.13).
Discussion
In this study, the prevalence and anatomic characteristics of AMF were evaluated using the CBCT technique in a selected Iranian population. AMF, as an anatomic and endemic variation, is of vital importance because of the exit of the accessory branches of nerves and arteries. The positions of the AMF must be considered when performing dental implant or periapical surgery in the posterior segment of the mandible. An AMN might be present, and AMF might be considered as a branch of the inferior alveolar nerve, which can cause anesthetic and surgical failures (14).
In the present study, the prevalence of AMF in 853 assessed CBCT images was 10.55%, which is consistent with the results of previous studies (1,15). Nonetheless, other studies using a wide variety of methods reported different prevalence rates in various ethnic groups and populations.(13,16-20) Based on the findings of Sawyer et al (11) the least prevalence rates were 1.4% and 1.5% among American whites and Asian Indians, respectively. Likewise, Riesenfeld (21) reported the prevalence rates of 3% and 3.6% for AMF among Hungarians and Egyptians, respectively. In addition, in a recent study by Paraskevas et al (22), the prevalence of AMF in a Greek population was 4.17%. Similarly, Khojastepour et al (23) reported a prevalence of 5.1% (8 cases) of AMF in a selected Iranian population, which was nearly half of our results. This contrast could be attributed to the significantly lower sample size of this study in comparison to that of our study. Furthermore, the method of assessment is important. Imada et al (24) evaluated 100 CBCT and panoramic images of patients for the presence of AMF and concluded that although CBCT evaluations showed a prevalence rate of 3%, no AMF was found on panoramic radiographs. Therefore, the evaluation of panoramic images may not be a reliable method for assessing the prevalence of AMF because of false-negative results and the inability to identify patients with AMF. CBCT can be highly helpful in the detection of MF variations such as the AMF, which could be missed using conventional radiographs (25,26)
The prevalence of double AMFs in this study was 0.9%. Additionally, Gershenson et al (17), Katakami et al (15), and Naitoh et al8 reported 0.7%, 0.6%, and 0.9% rates, respectively. In addition, Gershenson et al (17) found one case with three single-sided AMFs among 525 evaluated human dry mandibles. Similarly, one case with three two-sided AMFs (one on the right side and two on the left side) was detected in this study. Moreover, the findings of the present study showed no gender differences in the AMF distribution, which is in line with the results of previous studies (8,16,23,27). In contrast, Han et al (28) and Kieser et al (29) reported that AMF was more prevalent in males in comparison to females.
Regarding the position of AMF, the relationship between the topographic position of AMF and MF was evaluated in this study. Previous studies yielded controversial results similar to the relations of tooth roots. These discrepancies might be attributed to the fact that the position of AMF depends on the exact location of accessory nerve branching from the inferior alveolar nerve and its length (27) In this study, the posterior-inferior was the most prevalent position of AMF, followed by the anterior-inferior position, which corroborates with the results of the study by Naitoh et al8 carried out on a Japanese population. In another study, Kalender et al (27) reported the anterior-inferior position as the most common site of AMF. They further reported anterior, posterior, and anterior-superior positions with the least prevalence rate. Contrarily, these positions exhibited a moderate prevalence in this study. In one osteological study, AMF diameters ranged from 0.74 to 0.89 mm (14).
AMFs might be as small as 0.1 mm or reach a width exceeding 1.5 mm and often resemble the size of the MF (30). Kalender et al (27) reported the mean vertical and horizontal dimensions of 1.4 and 1.6 mm for the AMF, respectively. Based on our results, the mean size of the large and small diameters was 1.4 mm (ranging from 0.2 to 3.46 mm) and 1 mm (ranging from 0.2 to 2.5 mm), respectively.
In this study, as recommended by Kalender et al (27), the vertical positions of MF and AMF were evaluated in terms of the distance between the inferior margin of the foramen and the inferior border of the mandible since this region is not affected by bone resorption. Consistent with the findings of the previous studies (26,27,31), our results showed that MF was closer to the alveolar bone compared to AMF. In addition, the vertical heights of MF and AMF in males were more than those in females, which can be attributed to smaller sizes of female mandibles in comparison to males in this study population. Thus, this parameter could be used as a reference in order to prevent nerve damage during periapical surgeries (23). In this study, as shown by Kalender et al (27). there was a significant difference between the height of AMF and MF, and AMF had a lower vertical height. Thus, it had a lower vertical position compared to MF. Furthermore, the relationship between the vertical dimensions of MF and the presence of AMF was not significant, which is consistent with the findings of Zmysłowska-Polakowska et al (16).
Different studies reported amounts ranging from 0.67 to 6.3 mm for the distance between the AMF and the MF (8,24,27,32). In the present study, this distance was 7.62 mm, which was considerably higher than the mean values reported before. The results of different studies assessing the distance between AMF and MF differed due to the location of AMF, which is affected by the branching site and the length of the accessory branch. Longer branched nerves result in increased distances between the AMF and the MF (27).
Our findings about the location of AMF branching from the main canal are consistent with those of the previous studies (8,15,27), and the most common condition was branching from the anterior loop (70%). However, our results did not support the hypothesis of previous studies (15,27), indicating that the presence of AMF is because of a separating branch of the mental nerve before exit from the MF since 24% of cases of AMF were due to nerve branching from the anterior branch of the mandibular canal. Finally, 5% of the cases of the AMF nerve directly originated from the mandibular canal.
Conclusions
In general, the findings of the present study revealed that the prevalence of AMF according to hemi-mandibular was 5.80% in a selected Iranian population. Thus, AMF might branch from any section of the inferior alveolar nerve and the mandibular canal.
Authors’ Contribution
Noruzi M: Concepts, design, definition of intellectual content, data aquisition and manuscript review; Mostafavi M: Data acquitsition, data analysis and litreture search; Ghaznavi A: Concepts, design, data aqcusition, statistical analysis; Abdollahi AA: Litreture search, manuscript preparation, manuscript editing, manuscript review and corresponding author. All authors read and approved the manuscript.
Conflict of Interest Disclosures
The authors deny any conflict of interests.
Ethical Statement
This study was approved by the Ethics Committee of Urmia University of Medical Sciences, Iran
(No. 1396-09-35-3026).
Acknowledgement
The authors thank the Research Vice-chancellor of Urmia University of Medical Sciences.
References
- Al-Khateeb T, Al-Hadi Hamasha A, Ababneh KT. Position of the mental foramen in a northern regional Jordanian population. Surg Radiol Anat 2007; 29(3):231-7. doi: 10.1007/s00276-007-0199-z [Crossref] [ Google Scholar]
- Voljevica A, Talović E, Hasanović A. Morphological and morphometric analysis of the shape, position, number and size of mental foramen on human mandibles. Acta Med Acad 2015; 44(1):31-8. doi: 10.5644/ama2006-124.124 [Crossref] [ Google Scholar]
- Makris N, Stamatakis H, Syriopoulos K, Tsiklakis K, van der Stelt PF. Evaluation of the visibility and the course of the mandibular incisive canal and the lingual foramen using cone-beam computed tomography. Clin Oral Implants Res 2010; 21(7):766-71. doi: 10.1111/j.1600-0501.2009.01903.x [Crossref] [ Google Scholar]
- Balcioglu HA, Kocaelli H. Accessory mental foramen. N Am J Med Sci 2009; 1(6):314-5. [ Google Scholar]
- Jacobs R, Lambrichts I, Liang X, Martens W, Mraiwa N, Adriaensens P. Neurovascularization of the anterior jaw bones revisited using high-resolution magnetic resonance imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103(5):683-93. doi: 10.1016/j.tripleo.2006.11.014 [Crossref] [ Google Scholar]
- Pommer B, Tepper G, Gahleitner A, Zechner W, Watzek G. New safety margins for chin bone harvesting based on the course of the mandibular incisive canal in CT. Clin Oral Implants Res 2008; 19(12):1312-6. doi: 10.1111/j.1600-0501.2008.01590.x [Crossref] [ Google Scholar]
- Angelopoulos C, Thomas SL, Hechler S, Parissis N, Hlavacek M. Comparison between digital panoramic radiography and cone-beam computed tomography for the identification of the mandibular canal as part of presurgical dental implant assessment. J Oral Maxillofac Surg 2008; 66(10):2130-5. doi: 10.1016/j.joms.2008.06.021 [Crossref] [ Google Scholar]
- Naitoh M, Hiraiwa Y, Aimiya H, Gotoh K, Ariji E. Accessory mental foramen assessment using cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107(2):289-94. doi: 10.1016/j.tripleo.2008.09.010 [Crossref] [ Google Scholar]
- Ludlow JB, Laster WS, See M, Bailey LJ, Hershey HG. Accuracy of measurements of mandibular anatomy in cone beam computed tomography images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103(4):534-42. doi: 10.1016/j.tripleo.2006.04.008 [Crossref] [ Google Scholar]
- Liang X, Jacobs R, Corpas LS, Semal P, Lambrichts I. Chronologic and geographic variability of neurovascular structures in the human mandible. Forensic Sci Int 2009; 190(1-3):24-32. doi: 10.1016/j.forsciint.2009.05.006 [Crossref] [ Google Scholar]
- Sawyer DR, Kiely ML, Pyle MA. The frequency of accessory mental foramina in four ethnic groups. Arch Oral Biol 1998; 43(5):417-20. doi: 10.1016/s0003-9969(98)00012-0 [Crossref] [ Google Scholar]
- von Arx T, Friedli M, Sendi P, Lozanoff S, Bornstein MM. Location and dimensions of the mental foramen: a radiographic analysis by using cone-beam computed tomography. J Endod 2013; 39(12):1522-8. doi: 10.1016/j.joen.2013.07.033 [Crossref] [ Google Scholar]
- Naitoh M, Yoshida K, Nakahara K, Gotoh K, Ariji E. Demonstration of the accessory mental foramen using rotational panoramic radiography compared with cone-beam computed tomography. Clin Oral Implants Res 2011; 22(12):1415-9. doi: 10.1111/j.1600-0501.2010.02116.x [Crossref] [ Google Scholar]
- Toh H, Kodama J, Yanagisako M, Ohmori T. Anatomical study of the accessory mental foramen and the distribution of its nerve. Okajimas Folia Anat Jpn 1992; 69(2-3):85-8. doi: 10.2535/ofaj1936.69.2-3_85 [Crossref] [ Google Scholar]
- Katakami K, Mishima A, Shiozaki K, Shimoda S, Hamada Y, Kobayashi K. Characteristics of accessory mental foramina observed on limited cone-beam computed tomography images. J Endod 2008; 34(12):1441-5. doi: 10.1016/j.joen.2008.08.033 [Crossref] [ Google Scholar]
- Zmysłowska-Polakowska E, Radwański M, Łęski M, Ledzion S, Łukomska-Szymańska M, Polguj M. The assessment of accessory mental foramen in a selected polish population: a CBCT study. BMC Med Imaging 2017; 17(1):17. doi: 10.1186/s12880-017-0188-6 [Crossref] [ Google Scholar]
- Gershenson A, Nathan H, Luchansky E. Mental foramen and mental nerve: changes with age. Acta Anat (Basel) 1986; 126(1):21-8. doi: 10.1159/000146181 [Crossref] [ Google Scholar]
- Shankland WE 2nd. The position of the mental foramen in Asian Indians. J Oral Implantol 1994; 20(2):118-23. [ Google Scholar]
- Oliveira-Santos C, Souza PH, De Azambuja Berti-Couto S, Stinkens L, Moyaert K, Van Assche N. Characterisation of additional mental foramina through cone beam computed tomography. J Oral Rehabil 2011; 38(8):595-600. doi: 10.1111/j.1365-2842.2010.02186.x [Crossref] [ Google Scholar]
- Kqiku L, Weiglein A, Kamberi B, Hoxha V, Meqa K, Städtler P. Position of the mental foramen in Kosovarian population. Coll Antropol 2013; 37(2):545-9. [ Google Scholar]
- Riesenfeld A. Multiple infraorbital, ethmoidal, and mental foramina in the races of man. Am J Phys Anthropol 1956; 14(1):85-100. doi: 10.1002/ajpa.1330140122 [Crossref] [ Google Scholar]
- Paraskevas G, Mavrodi A, Natsis K. Accessory mental foramen: an anatomical study on dry mandibles and review of the literature. Oral Maxillofac Surg 2015; 19(2):177-81. doi: 10.1007/s10006-014-0474-1 [Crossref] [ Google Scholar]
- Khojastepour L, Mirbeigi S, Mirhadi S, Safaee A. Location of mental foramen in a selected Iranian population: a CBCT assessment. Iran Endod J 2015; 10(2):117-21. [ Google Scholar]
- Imada TS, Fernandes LM, Centurion BS, de Oliveira-Santos C, Honório HM, Rubira-Bullen IR. Accessory mental foramina: prevalence, position and diameter assessed by cone-beam computed tomography and digital panoramic radiographs. Clin Oral Implants Res 2014; 25(2):e94-9. doi: 10.1111/clr.12066 [Crossref] [ Google Scholar]
- Jacobs R, Mraiwa N, vanSteenberghe D, Gijbels F, Quirynen M. Appearance, location, course, and morphology of the mandibular incisive canal: an assessment on spiral CT scan. Dentomaxillofac Radiol 2002; 31(5):322-7. doi: 10.1038/sj.dmfr.4600719 [Crossref] [ Google Scholar]
- Apinhasmit W, Methathrathip D, Chompoopong S, Sangvichien S. Mental foramen in Thais: an anatomical variation related to gender and side. Surg Radiol Anat 2006; 28(5):529-33. doi: 10.1007/s00276-006-0119-7 [Crossref] [ Google Scholar]
- Kalender A, Orhan K, Aksoy U. Evaluation of the mental foramen and accessory mental foramen in Turkish patients using cone-beam computed tomography images reconstructed from a volumetric rendering program. Clin Anat 2012; 25(5):584-92. doi: 10.1002/ca.21277 [Crossref] [ Google Scholar]
- Han SS, Hwang JJ, Park CS. The anomalous canal between two accessory foramina on the mandibular ramus: the temporal crest canal. Dentomaxillofac Radiol 2014; 43(7):20140115. doi: 10.1259/dmfr.20140115 [Crossref] [ Google Scholar]
- Kieser J, Kuzmanovic D, Payne A, Dennison J, Herbison P. Patterns of emergence of the human mental nerve. Arch Oral Biol 2002; 47(10):743-7. doi: 10.1016/s0003-9969(02)00067-5 [Crossref] [ Google Scholar]
- Shiller WR, Wiswell OB. Lingual foramina of the mandible. Anat Rec 1954; 119(3):387-90. doi: 10.1002/ar.1091190308 [Crossref] [ Google Scholar]
- Chrcanovic BR, Abreu MH, Custódio AL. Morphological variation in dentate and edentulous human mandibles. Surg Radiol Anat 2011; 33(3):203-13. doi: 10.1007/s00276-010-0731-4 [Crossref] [ Google Scholar]
- Tanaka H, Tanabe N, Shoji M, Suzuki N, Katono T, Sato S. Nicotine and lipopolysaccharide stimulate the formation of osteoclast-like cells by increasing macrophage colony-stimulating factor and prostaglandin E2 production by osteoblasts. Life Sci 2006; 78(15):1733-40. doi: 10.1016/j.lfs.2005.08.017 [Crossref] [ Google Scholar]