Avicenna J Dent Res. 12(1):8-12.
doi: 10.34172/ajdr.2020.03
Original Article
Evaluation of Shear Bond Strength of Composite Restoration by Different Dentin Bonding Systems Under Different Cycling Conditions
Mohadese Shokripour 1, Bahareh Asgartooran 1, *  , Sharareh Ghasemi 1
, Sharareh Ghasemi 1  , Farnaz Sepehrnia 2
, Farnaz Sepehrnia 2
Author information:
1Assistant Professor, Department of Restorative Dentistry, Dental School, Hamadan University of Medical Sciences, Hamadan, Iran.
2Dentist, Hamadan University of Medical Sciences, Hamadan, Iran.
Abstract
Background: Adhesion of composite resins to dentin is crucial in restorative dentistry. The aim of this study was to evaluate shear bond strength of composite restorations to dentin under different cycling conditions.
Methods: Ninety extracted premolar teeth were randomly divided into 9 groups (n=10). The samples were mounted in resin and sectioned to prepare dentin samples. Then the samples were polished with 600-grit silicon carbide sanding sheet, and adhesive types of bonding (5th generation/Ambar, 6th generation/Clearfil SE bond, 8th generation/G-Premio) were applied on them. Afterward, composite resin was bonded to the surface, and cycling was exerted (control: no cycling; thermal cycling: 3000 cycles, 5°C to 55°C; thermal/erosive cycling: thermal cycling and storage in hydrochloric acid, pH = 2.1, 5 minutes, 6 times a day, for 8 days). Shear bond test was done for the specimens. Finally, statistical analysis was done using a two-way analysis of variance (ANOVA) and Tukey test (P<0.001).
Results: G-Premio displayed the most bond strength. No significant differences were observed between Clearfil liner bond and Ambar bond. While significant differences were observed in different cycling conditions. Measured bond strength was reduced by thermal/erosive cycling.
Conclusions: Thermal cycling and thermal/erosive cycling could affect the shear bond strength of composite to dentin. Universal bonding systems can also increase the shear bond strength of composite resin to dentin.
Keywords: Shear bond, Dentin bonding, Composite restoration
Copyright and License Information
© 2020 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Asgartooran B, Shokripour M, Ghasemi S, Sepehrnia F. Evaluation of Shear Bond Strength of Composite Restoration by Different Dentin Bonding Systems Under Different Cycling Conditions. Avicenna J Dent Res. 2020;12(1):8-12. doi: 10.34172/ajdr.2020.03.
Background
Highlights
Nowadays, the demand for cosmetic restorations such as composites has increased, even for posterior teeth (1). Today, composites are regarded as one of the most widely used materials in dentistry. The prognosis of such dental restorations depends on the seal, and marginal adaptation. Failure to achieve marginal integration leads to a poor bond and postoperative sensitivity, as well as secondary caries and other problems (2). Adhesive agents are used in combination with composite materials; this creates micromechanical retention, making a strong, long-lasting connection between tooth structure and restoration (3,4). Bonding system components include: (a) etchant agents: they are acidic molecules that change or remove the smear layer and demineralize enamel and dentin, (b) primer: it contains hydrophobic and hydrophilic molecules and prepares the surface of hydrophilic dentin to receive the hydrophobic bonding resin (So primers provide the penetration of the bonding resin), and (c) adhesives: molecules that penetrate into the teeth and then bond with the composite material (5).
Laboratory tests are widely used to compare the bonding performance of adhesive systems. Shear bond strength tests are one of them; they use relatively large bonding areas for testing (diameter 3-6 mm, 7-28 mm2). The nominal (average) bond strength is calculated by dividing the fracture force by the cross-sectional area of the sample. The high incidence of cohesive failure in the substrate observed with these tests has led to the development of micro-bond strength tests, using samples with much smaller bonding regions (1 mm2) (6). Other materials can also be used. Composites are another used materials in this study essentially consisting a polymer or resin matrix in which a mineral filler is dispersed. One of the most commonly used composites are hybrid composites. These materials generally contain 75% to 85% inorganic fillers. The average particle size in them is 0.4-1 µm. Recent types of hybrid composites also contain very small nanofillers, which lead to better properties. These newer types of hybrid composites are called nanohybrid composites (7). In this study, the shear bond strength of composite restorations using different bonding systems and in different cycling conditions was investigated.
Materials and Methods
In this study, 90 healthy human teeth (premolars) that were extracted for orthodontic or periodontal problems were used. Teeth with caries, defects, and cracks were excluded. The teeth were cleaned and then the samples were kept in 1% sodium hypochlorite for disinfection for one week. The samples were then placed in distilled water until the testing time to prevent dehydration. The occlusal surface of the teeth was removed with an orthodontic trimmer to obtain a flat dentin surface without any remaining enamel, and water cooling was used perpendicularly on the longitudinal axis of the tooth to remove the heat. The dentin surface was polished with 600-grit silicon carbide (3M, St. Paul, MN, USA) sanding sheet for 60 seconds to obtain a uniform smear layer. The ends of each sample were buried in acrylic resin up to 1 mm below cementoenamel junction (CEJ). Three types of bonding were used for every group. Two different types of cycling and one control group without cycling were used. Hence, 9 study groups were divided into 3 groups with 30 cases. Group 1 was the control group to which the shear bond strength test was done after 24 hours of storage in distilled water. For group A, Ambar (AMB, FGM Prod Odont; Joinville, SC, Brazil; etch-and-rinse bonding) was used according to the manufacturer’s instructions after preparing the samples. In this group, 37% phosphoric acid (DiaDent, Chungcheongbuk-do, Korea) was used on the exposed dentin for 15 seconds. After washing and drying, the bonding was placed according to the factory instructions and light cured for 20 seconds by a light cure device (Guilin Woodpecker Medical Instrument Co., Ltd., China). A clear plastic mold with a diameter of 3 mm and a height of 2 mm was placed on the surface of the composite and cured for 20 seconds. Then the plastic mold was removed. In group B, self-etching bonding was used (Clearfil liner bond F (Kuraray Co., Osaka, Japan)). First, the primer was applied for 20 seconds and thinned with air for 10 seconds. Afterward, the adhesive layer was applied and cured for 20 seconds, and then like group A, composite was placed on the surface. For group C, G-Premio (GC, Tokyo, Japan) universal bonding was used, cured for 20 seconds according to the factory instructions, and then the composite was placed like the previous groups. In groups 2 and 3, bonding agents were applied exactly the same as the control group, and after the application of bonding and composite for group 2, thermal cycling was done with 3000 thermal cycles, at 5-55°C and with dwell time of 25 seconds. The transfer time was 5 seconds. For group 3, as for group 2, thermal cycles were applied. Afterward, erosive cycle was performed, in which the samples were immersed in hydrochloric acid at pH 2.1 at room temperature for 5 minutes, 6 times a day. Immersion interval was considered to be 90 minutes. This process was repeated for eight days and lasted 4 hours throughout the erosive cycle (8).
Shear Bond Strength Test
This test was performed by a universal machine. The shear force was applied to the composite-dentin interface with the aid of a cast-iron device, parallel to the enamel or dentin at a rate of 1 mm/minute until the breaking process took place. The values shown were recorded by the device. Bond strength was measured in megapascal. Fracture patterns were observed with 25X magnification with an optical microscope and classified into 3 groups: 1) adhesive (if it occurs in the adhesive interface), 2) mixed less than 50% in the composite with less than 50% of the total area attached to the dental substrate, mixed more than 50% in the composite with more than 50% of the total area attached to the dental substrate, and 3) cohesive (cohesive - tooth and cohesive - composite) (3).
Results
The highest mean shear bond strength was observed in the G-Premio bonding in the control group (14.90 ± 3.63). While the lowest shear bond strength was observed in the Clearfil liner bond in erosive group (7.79 ± 1.67) (Table 1).
The results of the two-way analysis of variance (ANOVA) showed that there was a statistically significant difference in the average shear bond strength in different periodic conditions (P < 0.001). There was also a significant difference between different types of bonding (P < 0.001, Table 2).
Table 1.
Comparison of Shear Bond Strength of Composite Restorations With Different Dentin Bonding Agents Under Periodic Conditions
|
Group
|
Bonding
|
Mean ± SD
|
95% Confidence Interval
|
|
Lower Bond
|
Upper Bond
|
| Control |
Ambar |
12.16 ± 3.39 |
10.10 |
14.21 |
| G-Premio |
14.90 ± 3.63 |
12.84 |
16.95 |
| Clearfil |
14.41 ± 2.34 |
12.35 |
16.46 |
| Thermal |
Ambar |
10.33 ± 3.29 |
8.27 |
12.38 |
| G-Premio |
13.28 ± 3.64 |
11.22 |
15.33 |
| Clearfil |
11.64 ± 3.07 |
9.58 |
13.69 |
| Erosive |
Ambar |
7.60 ± 1.90 |
5.54 |
9.65 |
| G-Premio |
12.91 ± 1.85 |
10.58 |
14.96 |
| Clearfil |
7.79 ± 1.67 |
5.73 |
9.84 |
Table 2.
Results of Two-Way Analysis of Variance (ANOVA) for the Comparison of the Average Shear Bond Strength of Composite Restorations Under Different Bonding Systems
|
Source
|
Sum of Squares
|
df
|
F
|
P
value
|
| Group |
289.37 |
2 |
13.52 |
<0.001 |
| Bonding |
208.47 |
2 |
9.74 |
<0.001 |
| Group * bonding |
59.41 |
4 |
1.38 |
0.245 |
Tukey test results showed that there was a statistically significant difference in the mean shear bond strength of composite restorations between the control group, thermal, and thermal/erosive groups. The difference between thermal and thermal/erosive groups was also significant (Table 3; mean difference ± SE = 4.39 ± 0.84).
Table 3.
Results of Tukey Post Hoc Test for the Comparison of Shear Bond Strength of Composite Restorations Under Different Periodic Conditions
|
Group (I)
|
Group (J)
|
Mean Difference (I-J) ± SE
|
P
Value
|
| Control |
Thermal |
2.07 ± 0.84 |
0.042 |
| Erosive |
4.39 ± 0.84 |
<0.001 |
| Erosive |
Thermal |
2.31 ± 0.84 |
0.020 |
The results of the Tukey test showed that there was a statistically significant difference in the mean shear bond strength between Ambar and G-Premio groups. There was also a significant difference between Clearfil and G-Premio groups (P < 0.001). Nonetheless, there was no statistically significant difference between Ambar and Clearfil bonds (Table 4 and Figure 1).
Table 4.
Tukey Post Hoc Test Results for the Comparison of the Shear Bond Strength of Composite Restorations With Different Bonding Systems
|
Bonding (I)
|
Bonding (J)
|
Mean Difference (I-J) ± SE
|
P
Value
|
| Ambar |
G-Premio |
-3.66± 0.84 |
<0.001 |
| Ambar |
Clearfil |
-1.25 ± 0.84 |
0.306 |
| Clearfil |
G-Premio |
-2.41± 0.84 |
0.015 |
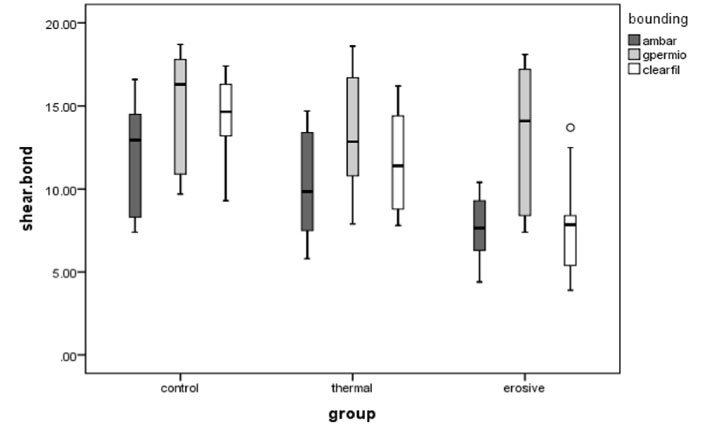
Figure 1.
Box Diagram for Comparing the Shear Bond Strength of Composite Restorations With Different Bonding Systems Under Periodic Conditions
.
Box Diagram for Comparing the Shear Bond Strength of Composite Restorations With Different Bonding Systems Under Periodic Conditions
Stereomicroscopic Analysis
In images from an optical microscope, the fracture patterns of the unbonded areas between the composite and the dentin were surveyed. The most common failure pattern in all three bonds studied was an adhesive failure. The lowest pattern of failure was related to the cohesive failure. Mixed failures (less than 50%) were more than mixed failures (more than 50%). In the control group, Clearfil, and G-Premio, the mixed failure (more than 50%) was observed. Cohesive failure was also observed only in the G-Premio bonding group (Table 5; Figures 2 and 3A-D).
Table 5.
Distribution of the Number of Different Fractures by Cycle Type and Bonding Group Used on Dentin
|
Bonding
|
Cycle
|
Bond Failure Pattern
|
|
Adhesive
|
Mixed <50%
|
Mixed >50%
|
Cohesive
|
| Ambar |
Control |
8 |
2 |
0 |
0 |
| Thermal |
9 |
1 |
0 |
0 |
| Thermal/erosive |
10 |
0 |
0 |
0 |
| Clearfil |
Control |
7 |
2 |
1 |
0 |
| Thermal |
8 |
2 |
0 |
0 |
| Thermal/erosive |
10 |
0 |
0 |
0 |
| G-Premio |
Control |
7 |
1 |
1 |
1 |
| Thermal |
8 |
1 |
0 |
1 |
| Thermal/erosive |
8 |
1 |
0 |
1 |
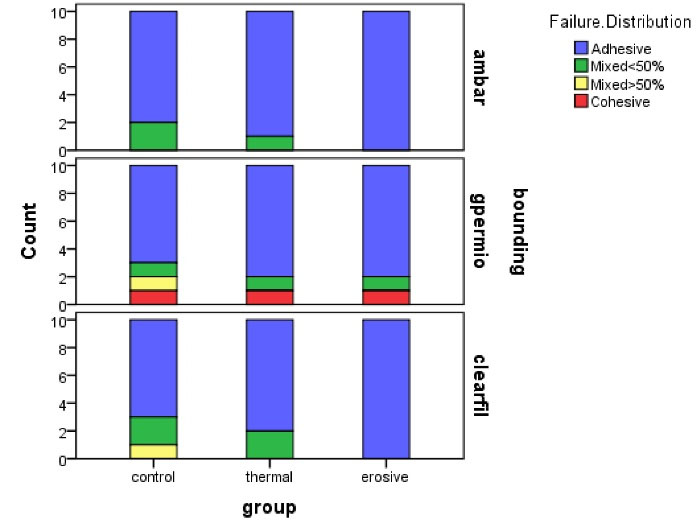
Figure 2.
Distribution of Failure Patterns on Dentin Substrate
.
Distribution of Failure Patterns on Dentin Substrate
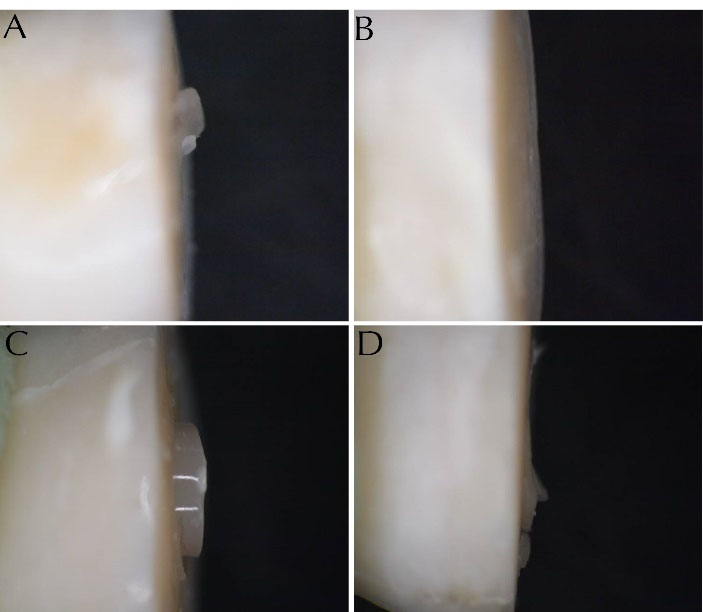
Figure 3.
25X Magnification Image of (A) a 50% Mixed, (B) the Adhesive, (C) the Cohesive, and (D) 50% Mixed Fracture Failure Sample Obtained From a Stereomicroscope.
.
25X Magnification Image of (A) a 50% Mixed, (B) the Adhesive, (C) the Cohesive, and (D) 50% Mixed Fracture Failure Sample Obtained From a Stereomicroscope.
Statistical Analysis
Data were analyzed using SPSS software version 21. In this study, to compare the shear bond strength of composite restorations with different dentin bonding systems under periodic conditions, a two-way analysis of variance was used. The normality of the data distribution was also assessed by the Kolmogorov-Smirnov test. The results showed that the normality assumption was established. Significance level was considered α = 0.05. Further, Tukey post hoc test was used to compare the two groups.
Discussion
Nowadays, the use of composite restorations has been expanded due to aesthetics. Mechanical attachment to dental tissue, conservative tooth extraction, and greater patient acceptance are the issues to be tackled (9). The strong and durable interface, bonded to enamel or dentin, significantly protects the restoration from the penetration of bacteria that may cause secondary decay. It also reduces the need for trapped areas in the incision that require the removal of a healthy dental structure. In some cases, bonding may help to strengthen the remaining tooth structure (6). The thermal cycle is a common thermal fatigue method for evaluating the durability of composite bonds (10,11). Therefore, failure of the adhesive-restorative material may occur after the thermal cycle, indicating that this method is effective for measuring the valuesb of bond strength (10). Ernest et al showed that thermal stresses between 5°C and 55°C are actually the same temperature that occurs inside the mouth (12). ISO standards state that the residence time for resin materials must be at least 20 seconds in every thermal bath (13). In our study, 3000 thermal cycles were applied with a temperature shock of 5-55°C for 25 seconds, which can be one of the positive points of the present study. An important issue about durability of resin restorative materials is erosive (acidic) cycles. This cycle is used to predict their behavior. This model has also been proven to evaluate cariogenic challenges that are clinically similar to in vitro studies (14). Hydrochloric acid is commonly used to simulate intraoral erosion. The total erosion time in the present study was 4 hours (8). It seems that the passage of liquid after the acid cycle causes hydrolysis effects. This is actually the main factor involved in the destruction of the matrix. Expansion of the matrix can cause cavities inside the restorative material. This causes organic materials to be released through it and shortens the lifespan of the restorative material (15,16). One of the results obtained in the present study was that the application of thermal and thermal/erosive cycles significantly reduced the bond strength in the three types of bonding used in our study. This result was in line with the study result of Zanatta et al who compared the bond strengths of 5th and 6th generations with thermal and thermal/erosive cycles. They observed that at the enamel edge, the bond strength in the control group was significantly lower than that in the thermal and thermal/erosive cycles. However, this decrease in bond strength was not significant in the dentin group (8). Considering the 3-mm diameter of the prepared composite samples in this study, the macro-shear bond strength test was used. In this test, the higher was the stress concentration in the applied area, the lower was the bond strength (6). Based on the results of this study, there was a statistically significant difference in the average shear bond strength between the G-Premio group and the Clearfil and Ambar bonding groups. These results were similar to those of Joseph et al. In their study, the highest average bond strength was related to the Futura bond DC bonding group (8th generation) which had significantly higher bond strength than Clearfil SE bond (6th generation) and Adper Easy One (7th generation). The 8th-generation bonding group has nano-sized cross-linking agents that increase its bonding potential to hydroxyapatite. It also has silica particles, as well as the benefits of being dual-cure (17). On the other hand, the presence of BTH (butylated hydroxyl toluene) in G-Premio can be a factor for its high bandwidth. The behavior of universal adhesives is highly dependent on the composition of the material. BTH acts as an inhibitor and prevents spontaneous polymerization and increases the durability of the resin, which may explain the high bond strength of this adhesive. G-Premio contains three functional monomers of MDP, 4META, and MDPT, which make them suitable for bonding to all types of substrates (18). In the present study, no statistically significant difference was observed between the 5th and 6th generations. But the Clearfil liner bond showed higher bond strength than Ambar bond. This may occur since this mildly pH-bonded 6th generation bond easily decalcifies the dentin, and the MDP reacts chemically with hydroxyapatite, increasing the bond relative to etch-and-rinse systems. Meharry et al investigated the shear bond strength of self-etching and total etching systems in dentin. They concluded that there was no statistically significant difference in shear bond strength of dentin bonding factors between self-etching and total etching systems, which is in line with the results of this study (8). Rao et al reported no statistically significant difference between self-etch and universal bonding factors. These results are inconsistent with the results of the present study and this may be due to insufficient drying time or bonding method. These factors are effective in the bond strength obtained from the universal bond. Other variables such as functional monomers, cross-linking monomers, solvents, inhibitors, and activators can vary in bonds, which in turn can affect the bond strength obtained. In fact, the amounts of monomer, diluent, and filler in bonding systems vary according to their different manufacturing technology, for them manufacturers do not give a detailed explanation of the exact composition of the bonding offered. These factors are involved in the bond strength obtained from different types of bonding. The type of test taken for bond strength can also be one of the factors involved in the results. The duration and storage conditions of the substrate also affect the results (19). Kamble et al studied 8th generation bonds and self-etch bonding systems. They found that the tensile bond strength of 8th generation bonding was higher than that of the 6th and 7th generation bonds, which was similar to this study. The reason for these observations can be the monomers in 8th generation bonding systems which cause strong cross-links into the bonding; so, they create stronger bands (2).
Conclusion
The results of the present study showed that the thermal cycle alone or thermal/erosive cycle reduced the shear bond strength of composite to dentin, and universal bonding systems in composite-dentin restorations had the highest bond strength compared to the 5th and 6th generation bonding systems.
Conflict of Interest Disclosures
The authors declare that they have no conflict of intrests.
Acknowledgements
We would like to thank the vice chancellor of research, Hamadan University of Medical Sciences, for supporting this study.
Ethical Statement
The study was approved by the ethical committee of Hamadan University of Medical Sciences. (Code: IR.UMSHA.REC.1397.691)
Authors’ Contribution
All authors have contributed to the concept and design of the study. FS contributed to the data collection.The statistical analyses and interpretation of data were carried out by FS, BA, MS and SG. BA, MS and SG drafted the manuscript. All the authors critically revised, read and approved the final manuscript.
Funding
None.
References
- Manhart J, Neuerer P, Scheibenbogen-Fuchsbrunner A, Hickel R. Three-year clinical evaluation of direct and indirect composite restorations in posterior teeth. J Prosthet Dent 2000; 84(3):289-96. doi: 10.1067/mpr.2000.108774 [Crossref] [ Google Scholar]
- Kamble SS, Kandasamy B, Thillaigovindan R, Goyal NK, Talukdar P, Seal M. In vitro comparative evaluation of tensile bond strength of 6th, 7th and 8th generation dentin bonding agents. J Int Oral Health 2015; 7(5):41-3. [ Google Scholar]
- Eick JD, Gwinnett AJ, Pashley DH, Robinson SJ. Current concepts on adhesion to dentin. Crit Rev Oral Biol Med 1997; 8(3):306-35. doi: 10.1177/10454411970080030501 [Crossref] [ Google Scholar]
- Nagpal R, Manuja N, Tyagi SP, Singh UP. In vitro bonding effectiveness of self-etch adhesives with different application techniques: a microleakage and scanning electron microscopic study. J Conserv Dent 2011; 14(3):258-63. doi: 10.4103/0972-0707.85805 [Crossref] [ Google Scholar]
- Medić V, Obradović-Djuricić K, Dodić S, Petrović R. In vitro evaluation of microleakage of various types of dental cements. Srp Arh Celok Lek 2010; 138(3-4):143-9. doi: 10.2298/sarh1004143m [Crossref] [ Google Scholar]
- Ronald Sakaguchi. Craig’s Restorative Dental Materials. 12th ed. Mosby; 2006.
- Strosberg E, Mayor F. Art and Science. UNESCO; 1999.
- Meharry MR, Moazzami SM, Li Y. Comparison of enamel and dentin shear bond strengths of current dental bonding adhesives from three bond generations. Oper Dent 2013; 38(6):E237-45. doi: 10.2341/12-521-l [Crossref] [ Google Scholar]
- Mackenzie L, Shortall AC, Burke FJ. Direct posterior composites: a practical guide. Dent Update 2009; 36(2):71-2, 4. doi: 10.12968/denu.2009.36.2.71 [Crossref] [ Google Scholar]
- Yang B, Adelung R, Ludwig K, Bössmann K, Pashley DH, Kern M. Effect of structural change of collagen fibrils on the durability of dentin bonding. Biomaterials 2005; 26(24):5021-31. doi: 10.1016/j.biomaterials.2005.01.024 [Crossref] [ Google Scholar]
- Dos Santos PA, Garcia PP, Palma-Dibb RG. Shear bond strength of adhesive systems to enamel and dentin Thermocycling influence. J Mater Sci Mater Med 2005; 16(8):727-32. doi: 10.1007/s10856-005-2609-2 [Crossref] [ Google Scholar]
- Ernst CP, Canbek K, Euler T, Willershausen B. In vivo validation of the historical in vitro thermocycling temperature range for dental materials testing. Clin Oral Investig 2004; 8(3):130-8. doi: 10.1007/s00784-004-0267-2 [Crossref] [ Google Scholar]
- International Organization for Standardization. Dental Materials - Guidance on Testing of Adhesion to Tooth Structure. Geneva, Switzerland: International Organization for Standardization; 1994.
- Zanatta RF, Lungova M, Borges AB, Torres C, Sydow HG, Wiegand A. Microleakage and shear bond strength of composite restorations under cycling conditions. Oper Dent 2017; 42(2):E71-E80. doi: 10.2341/16-132-l [Crossref] [ Google Scholar]
- Hashimoto M, Ohno H, Sano H, Kaga M, Oguchi H. In vitro degradation of resin-dentin bonds analyzed by microtensile bond test, scanning and transmission electron microscopy. Biomaterials 2003; 24(21):3795-803. doi: 10.1016/s0142-9612(03)00262-x [Crossref] [ Google Scholar]
- Sauro S, Watson TF, Tay FR, Chersoni S, Breschi L, Bernardi F. Water uptake of bonding systems applied on root dentin surfaces: a SEM and confocal microscopic study. Dent Mater 2006; 22(7):671-80. doi: 10.1016/j.dental.2005.08.006 [Crossref] [ Google Scholar]
- Joseph P, Yadav C, Satheesh K, Rahna R. Comparative evaluation of the bonding efficacy of sixth, seventh and eight generation bonding agents: an in vitro study. Int Res J Pharm 2013; 4(9):143-7. doi: 10.7897/2230-8407.04930 [Crossref] [ Google Scholar]
- Diniz AC, Bandeca MC, Pinheiro LM, Dos Santosh Almeida LJ Jr, Torres CR, Borges AH. Influence of different etching modes on bond strength to enamel using universal adhesive systems. J Contemp Dent Pract 2016; 17(10):820-5. doi: 10.5005/jp-journals-10024-1937 [Crossref] [ Google Scholar]
- Rao SA, Roopa D. Comparative evaluation of the bonding efficacy of seventh generation bonding agent and peak universal bond: an in-vitro study. J Interdiscipl Med Dent Sci 2015; 3(2):167. doi: 10.4172/2376-032X.1000167 [Crossref] [ Google Scholar]