Avicenna J Dent Res. 12(1):31-34.
doi: 10.34172/ajdr.2020.07
Case Report
Mandibular Thinning Due to Peripheral Hemangioma: A Case Report
Atie Safaee 1, 2  , Shahin Moeini 3, *
, Shahin Moeini 3, * 
Author information:
1Assistant Professor, Department of Oral and Maxillofacial Radiology, School of Dentistry, Mashhad University of Medical Sciences, Mashhad, Iran.
2Oral and Maxillofacial Diseases Research Center, Mashhad University of Medical Sciences, Mashhad, Iran.
3Postgraduate Student, Department of Oral and Maxillofacial Radiology, School of Dentistry, Mashhad University of Medical Sciences, Mashhad, Iran.
Abstract
Background: Peripheral hemangioma is a benign congenital lesion and when involving the tongue, it does not appear on panoramic radiography.
Case Presentation: This case report describes a 29-year-old male patient with peripheral hemangioma in his tongue and left side of the lower lip. In panoramic radiography, some calcifications are seen. In cone beam computed tomography (CBCT), more calcifications (phleboliths) and mandibular thinning are seen and if the lesion is not excised, it can result in mandibular fracture. As is known, biopsy or surgical excision of this lesion can result in severe hemorrhage, leading even to death. Therefore, accurate clinical and radiographic diagnosis is essential before starting any surgical intervention.
Conclusions: Exact evaluation of panoramic radiographs by dentists is important for the detection of silent lesions. With early detection of these lesions, many side effects can be prevented. On the other hand, sometimes peripheral lesions, such as peripheral hemangiomas, affect adjacent bone in a way that mimics a central lesion and are difficult to distinguish using only two-dimensional images such as panoramic radiographs. Therefore, using complementary imaging techniques such as CBCT scans can help us better understand the extent of the lesion and its effects on adjacent structures.
Keywords: Cone-beam computed tomography, Hemangioma, Mandible
Copyright and License Information
© 2020 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Safaee A, Moeini S. Mandibular Thinning Due to Peripheral Hemangioma: A Case Report. Avicenna J Dent Res. 2020;12(1):31-34. doi: 10.34172/ajdr.2020.07.
Background
Hemangiomas are the most common benign congenital lesions in humans and are characterized by the proliferation of blood vessels. They are often present at birth or appear soon after, and grow rapidly by endothelial proliferation. Today, discussion continues on whether they are in fact neoplasms or hamartomas. Hemangioma is histologically classified by Thoma as peripheral type (arising from periosteum) and central or intraosseous type (arising from central spongiosa) (1,2).
Phleboliths are calcified thrombi within a vein often in the presence of vascular malformations or hemangiomas. The etiology includes injury to the vessel wall and stagnation of the blood flow. Healing may involve formation of a protective thrombus which may be calcified. They may have either a radiopaque or radiolucent core. In the maxillofacial region, they are usually multiple and associated with hemangioma (34). Therefore, when phleboliths are seen on panoramic radiography, other radiographs such as CBCT should be checked to assess the extension of peripheral hemangioma and its effect on surrounding structures.
In this report, a patient with phleboliths and peripheral hemangiomas is described.
Case Presentation
Highlights
-
Exact evaluation of panoramic radiographs is important for the detection of silent lesions.
-
Sometimes peripheral lesions affect adjacent bone in a way that mimics a central lesion.
-
Advanced imaging techniques such as CBCT scans provide more accurate information to find the effects of lesion on the surrounding structures and to avoid side effects of late diagnosis.
A 29-year-old male patient with no medical problem referred to the Department of Oral and Maxillofacial Radiology of Mashhad School of Dentistry. His chief complaint was tooth pain. Intraoral examination revealed poor oral hygiene and multiple decayed teeth.
In an intraoral examination, bluish discoloration was seen in the tongue and left side of the lower lip (Figure 1A and 1B).
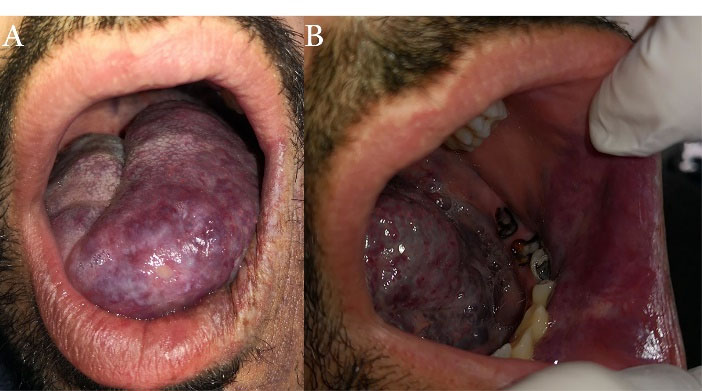
Figure 1.
Blue Discoloration Corresponding to Peripheral Hemangioma on the Left Side of (A) the Tongue and (B) the Lower Lip.
.
Blue Discoloration Corresponding to Peripheral Hemangioma on the Left Side of (A) the Tongue and (B) the Lower Lip.
A panoramic radiograph revealed multiple remained roots demonstrating the chief complaint of the patient. Some calcifications were seen in the posterior region of the mandibular body and upper parts of the ramus. In addition, a poorly-defined radiolucent lesion was seen on the left side of the mandibular body, extending from the left lateral incisor to the left second premolar. The lesion extended vertically from alveolar crest to the left inferior alveolar nerve canal. The periphery of the inferior alveolar nerve canal was not seen in the premolar region. The lamina dura of the canine and premolars was not observed. There was no evidence of root resorption (Figure 2).

Figure 2.
Panoramic Radiograph Indicating Poorly-Defined Radiolucency Extended From Lateral Incisor to the Second Premolar Region of the Left Side of the Mandible. Some calcified foci are seen in the posterior region of the mandibular body and upper parts of the ramus.
.
Panoramic Radiograph Indicating Poorly-Defined Radiolucency Extended From Lateral Incisor to the Second Premolar Region of the Left Side of the Mandible. Some calcified foci are seen in the posterior region of the mandibular body and upper parts of the ramus.
For the exact evaluation of this radiolucency and calcified foci, CBCT was taken. As seen in the axial view, there was severe mandibular thinning as a concavity in canine-premolar region. In addition, some calcifications were observed in cross-sectional images. They had a laminated appearance. There was no evidence of root resorption (Figures 3, 4, and 5). In the 3-D view, we found more calcified foci compared to the panoramic radiograph. According to clinical and radiographic findings, these calcifications were diagnosed as phleboliths (Figure 6). The blue-red lesions on the left side of the tongue and lower lip were diagnosed as congenital facial hemangiomas which were present from early childhood. Since these lesions had not caused discomfort or pain for the patient, no treatment, follow-up, or biopsy was done. Therefore, accurate clinical and radiographic examinations can help in early diagnosis and treatment and prevent complications such as mandibular fractures.
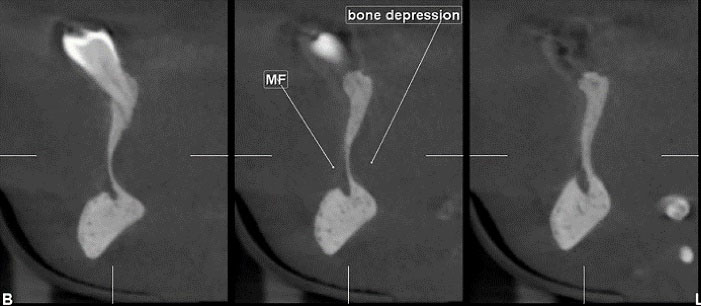
Figure 3.
Cross-sectional View of Cone-Beam CT Showing a Severe Concavity and 2 Calcified Foci With Laminated Appearance on Lingual Side of the Alveolar Ridge.
.
Cross-sectional View of Cone-Beam CT Showing a Severe Concavity and 2 Calcified Foci With Laminated Appearance on Lingual Side of the Alveolar Ridge.

Figure 4.
Panoramic-Like View of Cone-Beam CT Indicating Poorly-Defined Radiolucenat Area on the Left Side of the Mandibular Body
.
Panoramic-Like View of Cone-Beam CT Indicating Poorly-Defined Radiolucenat Area on the Left Side of the Mandibular Body
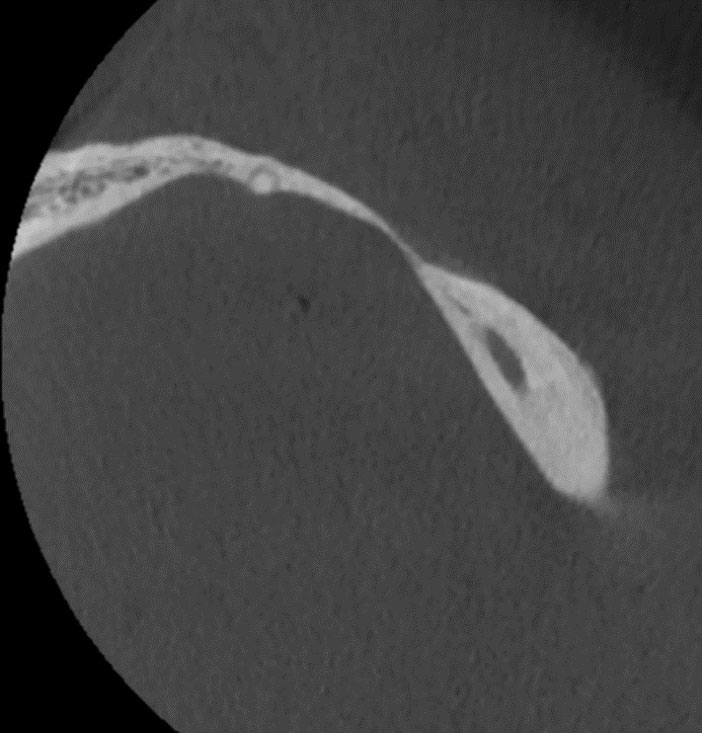
Figure 5.
Axial View of Cone-Beam CT Indicating Mandibular Thinning Due to the Effect of Peripheral Hemangioma.
.
Axial View of Cone-Beam CT Indicating Mandibular Thinning Due to the Effect of Peripheral Hemangioma.
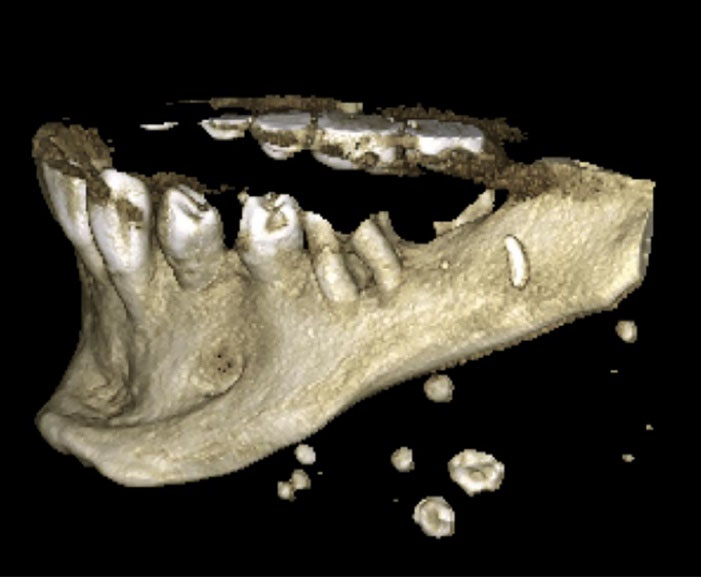
Figure 6.
3-D View of CBCT Indicating Multiple Phleboliths.
.
3-D View of CBCT Indicating Multiple Phleboliths.
Discussion
Hemangiomas are benign vascular lesions that cause symptoms such as mass, swelling, pain, and discoloration. They frequently occur on both skin and mucosal surfaces in the head and neck region but are rare in the oral cavity (5).
For this lesion, the female to male ratio is 2:1. They are mostly reported to occur between the second and fifth decades of life. The patient may be asymptomatic or may present with swelling, bleeding, bluish discoloration, mobile teeth, deranged arch, or early dental exfoliation. A very prominent feature is blood secretion from the sulcus (6,7).
Hemangiomas are usually seen as masses with well-defined phleboliths on tomography. Magnetic resonance imaging (MRI) can produce high signal intensity representing blood. In addition, focal heterogeneities represent areas of thrombosis, fibrosis, or calcifications. Hemangiomas show hyperintensity on T2-weighted images and isointensity on T1-weighted images. Phleboliths are seen as non-enhanced nodular structures in contrast-enhanced T1-weighted MRI scans and hypointense structures in T2-weighted MR scans (7,8).
Head or neck phleboliths must be differentiated from other calcifications, such as sialoliths, calcified lymph nodes, foreign bodies, tonsilloliths, atherosclerotic plaques in the carotid artery, healed acne lesions, cysticercosis, and miliary skin osteomas, which occur in the same area. Sialoliths appear on a single line when seen more than one, whereas phleboliths are randomly distributed. Phleboliths usually coexist with hemangiomas (9). Phlebolith is most frequently found in the pelvis area and head and neck region. In the latter area, they may be found in 15%-25% of intramuscular hemangiomas (3,10).
Ultrasonography is an inexpensive and noninvasive method and phleboliths are seen on it as multiple hyperechoic areas within the mass (9).
Dental treatments in Iran and many countries around the world are expensive and are not covered by insurance. Due to the unfavorable economic situation, the patient was not able to refer to the dentist for periodic dental examinations and his soft tissue lesion (peripheral hemangioma) was not diagnosed before. Prolonged pressure of the lesion on the adjacent bone resulted in severe concavity of the mandible. Mandibular thinning can lead to fractures even with minor to moderate trauma (such as tooth extraction). It is important to remember that the effect of peripheral lesions on adjacent bone may mimic the central lesions on two-dimensional images. In these cases, the use of advanced imaging techniques such as CBCT or CT can help us assess the origin and extent of the lesion.
One of the reasons that led us to report this case was that peripheral hemangioma was found as an incidental finding by careful examination of panoramic radiography. Panoramic radiography is the most common imaging method used in dentistry due to its relatively low radiation dose, wide field of view, patient comfort, and availability. Sometimes, a careful examination of this radiograph reveals things that may not have been noticed before. Such findings include metastatic lesions, atherosclerotic plaques, lesions with low expansion, and so on. Follow-up of these findings can lead to the prevention of adverse events or even save the patient’s life.
The treatment protocol for intramuscular hemangiomas is dependent on some clinical factors such as the age of the patient, size and location, rapidity of growth, and subjective symptoms. Some therapeutic approaches include intralesional injection of sclerosing agents (e.g., Bleomycin A5, sodium sulfate tetradecyl, sodium morrhuate, and ethanolamine oleate), cryotherapy, corticosteroids (either intralesional or systemic corticosteroids), embolization, laser therapy, and continued observation (4,8,11,12).
In some cases, surgical excision may be considered as the treatment of choice which can also eliminate the phleboliths. McHeik et al obtained good results with surgical excision of hemangiomas at early age (13).
Conclusions
Although our patient had been suffering from peripheral hemangioma for a long time, he had not been followed for dental examinations due to poor socio-economic conditions; therefore, severe mandibular thinning was not found before. As can be seen in this case, the long-term effect of this lesion on the surrounding bone can lead to severe mandibular thinning that can result in pathologic fractures with minor trauma or even without trauma. Panoramic radiography can show the presence of phleboliths and even mandibular thinning (as a radiolucent area), but this radiolucent area may be misdiagnosed as a central lesion in two-dimensional images. However, CBCT scan provides more accurate information to find the effects of lesions on the surrounding structures and to avoid side effects of late diagnosis.
On-going educational programs for dentists can create a good opportunity to emphasize the importance of a thorough examination of panoramic radiographs and referral of suspected cases for further evaluation.
Conflict of Interest Disclosures
The authors declare that they have no conflict of interests.
Authors’ Contribution
all authors contributed equally to this work.
Funding
None.
Informed consent
Informed consent was obtained from the patient for publication of this study.
References
- Edgerton MT. Steroid therapy of haemangioma. In: Williams HG, ed. Symposium on Vascular Malformation and Melanotic Lesions. St. Louis, MO: Mosby; 1983. p.74-83.
- Shafer WG, Hine MK, Levy BM. A Textbook of Oral Pathology. 4th ed. Philadelphia: W.B. Saunders Company; 1983. p. 154-7.
- Mandel L, Perrino MA. Phleboliths and the vascular maxillofacial lesion. J Oral Maxillofac Surg 2010; 68(8):1973-6. doi: 10.1016/j.joms.2010.04.002 [Crossref] [ Google Scholar]
- Yang WT, Ahuja A, Metreweli C. Sonographic features of head and neck hemangiomas and vascular malformations: review of 23 patients. J Ultrasound Med 1997; 16(1):39-44. doi: 10.7863/jum.1997.16.1.39 [Crossref] [ Google Scholar]
- Aynalı G, Unal F, Yarıktaş M, Yasan H, Ciriş M, Yılmaz O. Submandibular hemangioma with multiple phleboliths mimicking sialolithiasis: the first pediatric case. Kulak Burun Bogaz Ihtis Derg 2014; 24(3):168-71. doi: 10.5606/kbbihtisas.2014.24392 [Crossref] [ Google Scholar]
- Jain S, Singaraju S, Singaraju M. Central hemangioma: a case report and review of literature. J Indian Soc Pedod Prev Dent 2016; 34(1):87-91. doi: 10.4103/0970-4388.175525 [Crossref] [ Google Scholar]
- Zengin AZ, Celenk P, Sumer AP. Intramuscular hemangioma presenting with multiple phleboliths: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 115(1):e32-6. doi: 10.1016/j.oooo.2012.02.032 [Crossref] [ Google Scholar]
- Karslıoğlu Karslıoğlu, H H, Sümer AP. Hemangioma presenting with multiple phleboliths: case report with CBCT findings. Cumhuriyet Dental Journal 2018; 21(3):263-7. doi: 10.7126/cumudj.410482 [Crossref] [ Google Scholar]
- White SC, Pharoach MJ. Oral Radiology: Principles and Interpretation. 4th ed. Philadelphia: Mosby; 2000.
- Morris SJ, Adams H. Case report: paediatric intramuscular haemangiomata--don’t overlook the phlebolith!. Br J Radiol 1995; 68(806):208-11. doi: 10.1259/0007-1285-68-806-208 [Crossref] [ Google Scholar]
- Rossiter JL, Hendrix RA, Tom LW, Potsic WP. Intramuscular hemangioma of the head and neck. Otolaryngol Head Neck Surg 1993; 108(1):18-26. doi: 10.1177/019459989310800103 [Crossref] [ Google Scholar]
- Wolf GT, Daniel F, Krause CJ, Kaufman RS. Intramuscular hemangioma of the head and neck. Laryngoscope 1985; 95(2):210-3. doi: 10.1288/00005537-198502000-00018 [Crossref] [ Google Scholar]
- McHeik JN, Renauld V, Duport G, Vergnes P, Levard G. Surgical treatment of haemangioma in infants. Br J Plast Surg 2005; 58(8):1067-72. doi: 10.1016/j.bjps.2005.04.029 [Crossref] [ Google Scholar]