Avicenna J Dent Res. 11(4):131-134.
doi: 10.34172/ajdr.2019.26
Case Report
Management of Immature Permanent Teeth With Crown-Root Fracture: A Case Report With a 24-Month Follow-up
Arqavan Kamali Sabeti 1, Ali Aghajani 2, Arghavan Afshar 2, Zahra Pakseresht 3, Zahra Karimizade 1, * 
Author information:
1Assistant Professor, Department of Pediatric Dentistry, Dental School, Hamadan University of Medical Sciences, Hamadan, Iran.
2Resident, Department of Pediatric Dentistry, Dental School, Hamadan University of Medical Sciences, Hamadan, Iran.
3Assistant Professor, Department of Endodontics, Dental School, Gilan University of Medical Sciences, Rasht, Iran.
Abstract
Background: Crown root fractures are usually caused by severe horizontal trauma, involving enamel, dentine, and cementum, and continue down to the gingival margin. One of the most common areas affected by trauma in the mouth is maxillary central incisors.
Case Presentation: A10-year-old boy fractured his maxillary central incisors. The fracture line involved the pulp and extended subgingivally on the palatal aspect invading the biologic width. The procedure used to manage this case included endodontic treatment of residual teeth and surgical extrusion to move the fracture line above the alveolar bone. Finally, the teeth were restored with composite build-up.
Conclusion: During 24-month follow-up period, the teeth did not show any signs of root resorption. Therefore, surgical extrusion is recommended as a treatment option for crown/root fractures.
Keywords: Crown-root fracture, Immature tooth, Surgical extrusion
Copyright and License Information
© 2019 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Kamali Sabeti A, Aghajani A, Afshar A, Pakseresht Z, Karimizade Z. Avicenna J Dent Res. 2019;11(4):131-134. doi: 10.34172/ajdr.2019.26.
Background
Highlights
Although the oral region comprises only 1% of the total body area, oral injuries account for 5% of physical injuries of all ages. The most common etiologic factors are injuries from falls, bicycles, cars and collisions (1). In a study, Glendor demonstrated that one-third of all children have suffered a traumatic dental injury involving the primary dentition and one-fourth of all school children have suffered a trauma to the permanent dentition (2).
One of the most common areas affected by trauma in the mouth is maxillary central teeth due to their position and arch prominence in this region (3). The impact of dental trauma on a child’s confidence is of great importance as most dental traumas occur in the early years of life and adolescence, which are important periods of psychological development of a child (2). Anterior tooth trauma is a very bitter experience for young patients and has a psychological impact on the patient and his/her parents. If the injury results in the loss of extensive tooth structure, it changes the appearance of the child and makes the child be ridiculed by other children (4). Injuries to the tooth and its supporting structures may vary from enamel fractures to avulsion, with or without pulp involvement and bone fractures. Crown root fractures are usually caused by severe horizontal trauma, involving enamel, dentine, and cementum and continue down to the gingival margin. Depending on whether or not the pulp is involved, it is subdivided into complicated and uncomplicated. These injuries most often involve the maxilla central incisors before complete root formation. There are different treatment options depending on the location of the fracture including bonding of coronal fragment, gingivectomy, osteotomy, orthodontic extrusion, surgical extrusion and extraction of the tooth (5,6). The crown root fracture has exceeded the biologic width of the tooth; therefore, the goal of treatment is to expose the fracture line to the supragingival position. No matter which method is used, conditions should be provided to achieve optimum outcomes (7).
Case Presentation
A 10-year-old boy referred to the Department of Pediatric Dentistry of Hamadan University of Medical Sciences. The chief complaints of the patient were pain and fractures of anterior teeth (Figure 1). According to his parent’s report, he had a motorcycle accident two month ago. Medical history and extraoral examination were normal. A form of informed consent was signed by parents for performing treatment procedure and presenting case report in the future. In clinical and radiographic examinations, there were no maxillary and mandibular fractures. The patient had class II malocclusion with deep bite (Figure 2). Intraoral periapical radiography revealed partial loss of the crown and oblique crown root fracture of teeth 21 and 11. The development of root apex of teeth 21 and 11 was incomplete (Figure 3). Vitality pulp tests were performed and the teeth responded negatively to electrical and thermal tests. Due to the incomplete development of roots and the time elapsed since the injury, the prescribed treatment plan was the apexification of teeth with MTA plug (Figure 4). After pulp therapy, temporary restoration was applied to the teeth 21 and 11. After multidisciplinary consultation with Pediatric Orthodontics and Periodontology departments, it was decided that a surgical extrusion was the best way to expose the fracture line. Surgical extrusion was performed for definitive treatment and reconstruction of the coronal segment because the palatal portion of the fracture line continued down to the gingival margin and was approximately 1 mm below the alveolar crest. By a periosteal elevator and a sharp carver, the teeth were gently luxated. The teeth were extruded about 4 mm by forceps which took the mesiodistal of the tooth. Due to tooth mobility at this stage, fixation in the new position was performed by a wire-composite splint (wire diameter: 0.6 m) (Figure 5). Proper antibiotic therapy was prescribed for the patient for 10 days. The patient and his parents were informed about the importance of oral hygiene and soft diet during the healing period. After two weeks, the splint was removed and the tooth mobility significantly reduced (grade I). Then, temporary tooth restoration was removed and the fiber optic post was prepared and cemented with dual-cure resin. Finally, a composite build-up was performed for maximal aesthetic outcomes (Figure 6). During the follow-up period of 2 years, no trace of root resorption was observed (Figure 7). The patient referred to the Department of Orthodontics for orthodontic treatment.

Figure 1.
Intraoral View of Teeth 11 and 21 With Crown-Root Fractures.
.
Intraoral View of Teeth 11 and 21 With Crown-Root Fractures.

Figure 2.
Orthopantomographic View of the Patient.
.
Orthopantomographic View of the Patient.

Figure 3.
Pre-operative Periapical Radiography of Teeth 21 and 11.
.
Pre-operative Periapical Radiography of Teeth 21 and 11.
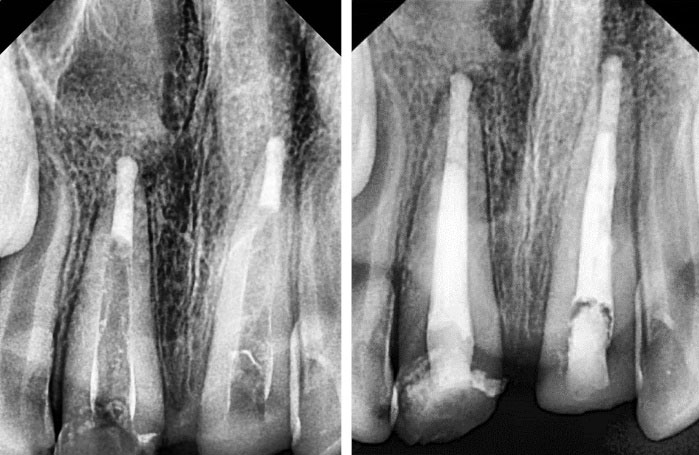
Figure 4.
Post-operative Periapical Radiography of Teeth 21 and 11 After Apexification.
.
Post-operative Periapical Radiography of Teeth 21 and 11 After Apexification.

Figure 5.
Surgical Extrusion and Wire-Composite Splint of Teeth 21 and 11.
.
Surgical Extrusion and Wire-Composite Splint of Teeth 21 and 11.

Figure 6.
Composite Build-up of the Teeth 21 and 11.
.
Composite Build-up of the Teeth 21 and 11.

Figure 7.
Periapical Radiography of Teeth 21 and 11 After 24-Month Follow-up.
.
Periapical Radiography of Teeth 21 and 11 After 24-Month Follow-up.
Discussion
In most studies, boys are more likely to have dental trauma than girls. Boys sustain dental trauma almost twice as much as girls since boys are more active in physical activity and contact sports. The peak of dental injuries occurs between the ages of 2 to 4 years in primary teeth and ages 8 to 10 in permanent teeth (8). In a prospective study by Andreasen on injuries from birth to the age 14 years, it was demonstrated that 30% of the children had trauma to the primary dentition and 22% to the permanent dentition. These injuries are most likely to affect the central maxillary incisors (9). In cases where the damaged tooth has an incomplete root development and requires complete pulp treatment, one of the treatment options is to close the apex of the roots by MTA plug (10). In most of the cases of crown/root fractures, the coronal segment displacement is minor, and the fracture line starts from a few millimetres above the gingiva on the fascial side and continues down to the gingival margin on the palatal side. In cases where conservative treatment is not possible due to the deep fracture below the gingival margin or the presence of pulpal pathology, preserving the apical segment is important to prevent alveolar bone resorption (6). In this case, surgical extrusion was preferable to other therapies because it offers a better crown/root ratio than gingivectomy and osteotomy (reducing root height and preserving crown length). Moreover, surgical extrusion was preferable to multi-session, long-term and costly orthodontic extrusion because the teeth were not vital.
Immobilization of tooth using a wire-composite splint, a semi-rigid splint, allows the tooth to move physiologically during the repair period. Functional splinting reduces replacement resorption. By reducing splint duration and rigidity, tooth prognosis improves (11). Extruded teeth should be examined for incomplete fractures as they are contraindication of repositioning (6). In a report of patients treated with 5-years follow up, root resorption was absent or very minor (12). In addition, in a 10-year follow-up study, all teeth treated with cervical extrusion survived, except for one case with cervical resorption (13).
Treatment and management of crown/root fracture require a multidisciplinary plan and the collaboration of several specialists to achieve optimal aesthetic outcomes. Factors to consider for choosing an ideal treatment plan include the depth and location of the fracture, root development, dental morphology, and aesthetic needs of each individual (14). Among the extrusion methods, orthodontic extrusion is suitable for immature vital teeth that preserve pulp vitality. In our case, surgical extrusion was chosen, which is a safe and rapid way to treat crown/root fractures. Additionally, in a systematic review study, it was stated that the surgical extrusion has advantages which include shorter chair-side time compared with other methods, good esthetics, and acceptance from the patient. The treatment failure rate in this method is very low (15). According to a systematic review by Elkhadem et al, ankylosis is not an adverse event to accompany surgical extrusion procedure. Surface resorption is a common finding following surgical extrusion, but it is self-limiting and should not be considered a harmful event. Slight mobility, progressive root resorption, marginal bone loss, and tooth loss are uncommon adverse events with a prevalence of less than 5% (16). In our case report, the patient was examined every 3 months during the follow-up period of 24 months. The teeth did not show any signs of root resorption during the treatment and follow-up periods. Therefore, surgical extrusion is recommended as a treatment option for crown/root fractures. Clinical and radiographic assessments during the follow-up period are very important as the highest rate of root resorption occurs in the first 2 to 3 years after the trauma.
Conclusions
During the 24-month follow-up period, the teeth did not show any signs of root resorption. Therefore, surgical extrusion was recommended as a treatment option for crown root fractures
Conflict of Interest Disclosures
The authors declare that they have no conflict of interests.
Ethical Statement
Informed consent was obtained from the parents’ patient for publication of this study.
Authors’ Contribution
The authors had same contribution in this study.
References
- Andreasen JO. Etiology and pathogenesis of traumatic dental injuries A clinical study of 1,298 cases. Scand J Dent Res 1970; 78(4):329-42. doi: 10.1111/j.1600-0722.1970.tb02080.x [Crossref] [ Google Scholar]
- Glendor U. Epidemiology of traumatic dental injuries--a 12 year review of the literature. Dent Traumatol 2008; 24(6):603-11. doi: 10.1111/j.1600-9657.2008.00696.x [Crossref] [ Google Scholar]
- Lee JH, Yoon SM. Surgical extrusion of multiple teeth with crown-root fractures: a case report with 18-months follow up. Dent Traumatol 2015; 31(2):150-5. doi: 10.1111/edt.12121 [Crossref] [ Google Scholar]
- Heda CB, Heda AA, Kulkarni SS. A multi-disciplinary approach in the management of a traumatized tooth with complicated crown-root fracture: a case report. J Indian Soc Pedod Prev Dent 2006; 24(4):197-200. doi: 10.4103/0970-4388.28077 [Crossref] [ Google Scholar]
- Calişkan MK, Türkün M, Gomel M. Surgical extrusion of crown-root-fractured teeth: a clinical review. Int Endod J 1999; 32(2):146-51. doi: 10.1046/j.1365-2591.1999.00199.x [Crossref] [ Google Scholar]
- Andreasen JO, Andreasen FM, Andersson L. Textbook and Color Atlas of Traumatic Injuries to the Teeth. John Wiley & Sons; 2018. p. 355-65.
- Olsburgh S, Jacoby T, Krejci I. Crown fractures in the permanent dentition: pulpal and restorative considerations. Dent Traumatol 2002; 18(3):103-15. doi: 10.1034/j.1600-9657.2002.00004.x [Crossref] [ Google Scholar]
- Lauridsen E, Hermann NV, Gerds TA, Kreiborg S, Andreasen JO. Pattern of traumatic dental injuries in the permanent dentition among children, adolescents, and adults. Dent Traumatol 2012; 28(5):358-63. doi: 10.1111/j.1600-9657.2012.01133.x [Crossref] [ Google Scholar]
- Andreasen JO, Ravn JJ. Epidemiology of traumatic dental injuries to primary and permanent teeth in a Danish population sample. Int J Oral Surg 1972; 1(5):235-9. doi: 10.1016/s0300-9785(72)80042-5 [Crossref] [ Google Scholar]
- Oliveira TM, Sakai VT, Silva TC, Santos CF, Abdo RC, Machado MA. Mineral trioxide aggregate as an alternative treatment for intruded permanent teeth with root resorption and incomplete apex formation. Dent Traumatol 2008; 24(5):565-8. doi: 10.1111/j.1600-9657.2008.00577.x [Crossref] [ Google Scholar]
- Kim CS, Choi SH, Chai JK, Kim CK, Cho KS. Surgical extrusion technique for clinical crown lengthening: report of three cases. Int J Periodontics Restorative Dent 2004; 24(5):412-21. doi: 10.11607/prd.00.0598 [Crossref] [ Google Scholar]
- Tegsjö U, Valerius-Olsson H, Frykholm A, Olgart K. Clinical evaluation of intra-alveolar transplantation of teeth with cervical root fractures. Swed Dent J 1987; 11(6):235-50. [ Google Scholar]
- Kim SH, Tramontina VA, Ramos CM, Prado AM, Passanezi E, Greghi SL. Experimental surgical and orthodontic extrusion of teeth in dogs. Int J Periodontics Restorative Dent 2009; 29(4):435-43. [ Google Scholar]
- Moura LF, Lima MD, Moura MS, Carvalho PV, Cravinhos JC, Carvalho CM. Treatment of a crown-root fracture with intentional replantation - case report with 16-year follow-up. Int Endod J 2012; 45(10):955-60. doi: 10.1111/j.1365-2591.2012.02078.x [Crossref] [ Google Scholar]
- Das B, Muthu MS. Surgical extrusion as a treatment option for crown-root fracture in permanent anterior teeth: a systematic review. Dent Traumatol 2013; 29(6):423-31. doi: 10.1111/edt.12054 [Crossref] [ Google Scholar]
- Elkhadem A, Mickan S, Richards D. Adverse events of surgical extrusion in treatment for crown-root and cervical root fractures: a systematic review of case series/reports. Dent Traumatol 2014; 30(1):1-14. doi: 10.1111/edt.12051 [Crossref] [ Google Scholar]