Avicenna J Dent Res. 11(3):98-103.
doi: 10.34172/ajdr.2019.19
Original Article
Evaluation of Postoperative Electrolyte Imbalance in Maxillofacial Surgery Patients
Omid Soltaninia 1, *  , Zohre Mousavie 2, Maryam Seyed Tabib 3, Seyed Masih Moosavi Seresht 4
, Zohre Mousavie 2, Maryam Seyed Tabib 3, Seyed Masih Moosavi Seresht 4
Author information:
1Assistant Professor, Department of Oral and Maxillofacial Surgery, School of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran
2Dentist, Private Practitioner
3PhD Student, Department of Biostatics and Epidemiology, School of Public Health, Hamadan University of Medical Sciences, Hamadan, Iran
4Resident of Oral and Maxillofacial Surgery, School of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran
Abstract
Background: Electrolytes play a significant role in the regulation of various vital functions in the human body. Changes in electrolyte composition can be pre-operative, intra-operative, and post-operative. The aim of this study was to analyze the incidence of electrolyte imbalances after a maxillofacial surgery and find possible relationship between imbalances and kind of surgery.
Methods: In this descriptive cross-sectional study, 101 maxillofacial surgery patients admitted to Besat educational hospital were selected by convenience sampling method. Serum electrolytes (sodium, potassium, calcium, and magnesium) of each patient were measured a day before the operation and on the first and the third post-operative days. The demographic and medical information and also details of the surgery of each patient were documented in checklists, which were used when all the needed data were collected. Statistical analysis was performed using SPSS version 23.0.
Results: Our results showed that, among electrolyte imbalances, hypocalcemia was the most frequent with 26.3%, followed by hyponatremia with 18.7%, and hypermagnesemia with 16.6%, while potassium demonstrated the least changes (6.3%) after a maxillofacial surgery. There was a significant correlation between the body mass index (BMI) and magnesium (P=0.032) and calcium (P=0.021) imbalances (hypo or hyper). Statistical analyses showed that magnesium abnormalities are more common in patients with jaw trauma on the third post-operative day in comparison with first postoperative day (P=0.037).
Conclusions: Hypocalcemia, hyponatremia, and hypermagnesemia are relatively common after maxillofacial surgeries. The findings showed that some factors such as the BMI and etiology of maxillofacial surgeries could cause electrolyte abnormalities after maxillofacial surgery. Identifying these factors could be useful in planning strategies for prevention, diagnosis, and early treatment of possible complications, which, in turn, may result in an improvement in the quality of care.
Keywords: Electrolyte disorders, Sodium, Potassium, Magnesium, Electrolyte imbalance, Maxillofacial surgery
Copyright and License Information
© 2019 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Soltaninia O, Mousavie Z, Seyed Tabib M, Moosavi Seresht SM. Evaluation of Postoperative Electrolyte Imbalance in Maxillofacial Surgery Patients. Avicenna J Dent Res. 2019;11(3):98-103. doi: 10.34172/ajdr.2019.19.
Background
Highlights
Electrolytes including potassium, sodium, magnesium, calcium, and phosphate play significant roles in enzymatic and biochemical reactions, the regulation of cellular membrane potentials, energy transformation, neurotransmission, nerve signal conduction, hormone function, muscle contraction, cardiovascular role, bone composition, and fluid and acid–base regulation (1,2).
Acute and severe electrolyte imbalances can induce a wide variety of clinical disorders, such as severe arrhythmias and neuromuscular dysfunction and are associated with increased morbidity and mortality (3). The risk posed by these abnormalities increases significantly when more than one electrolyte is deficient, and the severity of the symptoms is commonly associated with the severity of the disorder and the rate at which the disorder progresses (2).
Changes in both fluid volume and electrolyte composition happen preoperatively, intraoperatively, and postoperatively (4). Postoperative surgery patients are prone to electrolyte changes probably because of the loss of blood and bodily fluids, the stress response to surgery, fasting before surgery, the inability of the patients to receive necessary nutrition after the operation of the jaws, anesthesia and surgical trauma, fluid replacement and/or use of diuretics, blood transfusion, and the underlying surgical disease (5,6).
Sodium plays a key role in maintaining fluid balance of the body and also influences the functioning of the bodily muscles and the central nervous system. This electrolyte is the most abundant in the blood plasma and plays a major role in maintaining water balance in the blood and tissues. Sodium disorders are associated with an increased risk of morbidity and mortality (7). Hyponatremia is one of the common electrolyte abnormalities defined as a serum sodium level of less than 135 mEq/L and hyponatremia is the most common postoperative electrolyte disorder caused by surgical stress (7,8).
Potassium disorders are common. Hypokalemia (serum potassium level less than 3.6 mEq/L) is reported up to 21% among hospitalized patients and 2 to 3% among outpatients. The most common disorder after hyponatremia is a hypokalemia, which causes problems such as arrhythmia and muscle weakness (9,10). Hyperkalemia (serum potassium level more than 5 mEq/L) occurs in up to 10% of hospitalized patients and approximately 1% of outpatients. Hyperkalemia occurs commonly in hospitalized patients and is of particular concern for those who have undergone surgery, with postoperative care provided by clinicians of many disciplines (10,11).
Magnesium is one of the most common co-factors and is crucial to more than 300 enzyme-driven biochemical reactions in the body. Normal magnesium levels are between 1.8–2.5 mg/dL, with levels less than 1.8 mg/dL defining hypomagnesemia (12,13). Hypomagnesemia is commonly found in current medical practice mainly in critically ill and postoperative patients. Clinical symptoms of hypomagnesemia include neuromuscular, neurologic, psychiatric, and cardiac disorders, which may significantly increase the morbidity of such patients (13).
Postoperative hypocalcemia has been reported in a population of healthy patients undergoing surgery. The patients who receive massive blood transfusion during an acute surgical crisis are at risk of developing hypocalcemia (14).
Considering the importance of electrolytes and the role of surgery in causing electrolyte imbalance in the body, the aim of this study was to evaluate electrolyte disturbances (potassium, sodium, magnesium, and calcium) among the patients undergoing maxillofacial surgery in which the oral intake of nutrition by the patient was directly or indirectly affected.
Objectives
The aim of the study was to evaluate electrolyte disturbances (potassium, sodium, magnesium, and calcium) among the patients who had undergone maxillofacial surgery from November 2016 to May 2017.
Materials and Methods
In this descriptive cross-sectional study, 101 patients, who had undergone maxillofacial surgery, were studied with a convenience sampling at Besat hospital, Hamadan, Iran.
The inclusion criteria were: 1) patients undergoing orthognathic surgery, open and closed mandibular fracture surgery, and open and closed maxillary fracture surgery, 2) patient hospitalized for ≥3 days, 3) oral nutrition of the patient directly or indirectly affected during the post-operation period.
Demographic information (e.g., age and gender), weight, height, body mass index (BMI), kinds of trauma, medication, comorbidity and clinical data were compiled for each patient.
Preoperative and postoperative sodium, potassium, calcium, and magnesium were measured. Preoperative laboratory analysis was performed a day before surgery and postoperative analysis was done on days 1 and 3. Sodium (135–145 mEq/L), calcium (9–10.2 mg/dL), potassium (3.5–5.2 mEq/L), and magnesium (1.8–2.5 mg/dL) were considered normal. The incidence of pre-operative and post-operative hypomagnesemia, hypermagnesemia, Hyponatremia, hypernatremia, hypokalemia, hyperkalemia, hypocalcemia, and hypercalcemia were measured. In the present study, whenever the laboratory test revealed an abnormal electrolyte results which could be harmful to the patient, the plasma electrolyte was corrected.
Statistical Analysis
Statistical analysis was performed using SPSS version 23.0 (SPSS, Chicago, IL, USA). Frequency distribution tables were used to study electrolyte disturbances, as well as the decrease and increase of them on different days. The relationship between quantitative variables such as the BMI and surgical duration and sequential variables was analyzed using Spearman’s correlation coefficient and the relationship between qualitative variables such as gender and surgical etiology with sequential variables was analyzed using the chi-square test.
Results
The age of the patients ranged from 19 to 54 years (mean age=42.31 ± 1.9); 68 patients (67.3%) were male and 33 (32.7%) were female.
Eleven different maxillofacial surgical procedures had been performed on 101 patients. Among the 11 maxillofacial surgeries, the predominant ones were open mandibular fractures and complex mandibular fractures (27 and 23%, respectively) (Figure 1).
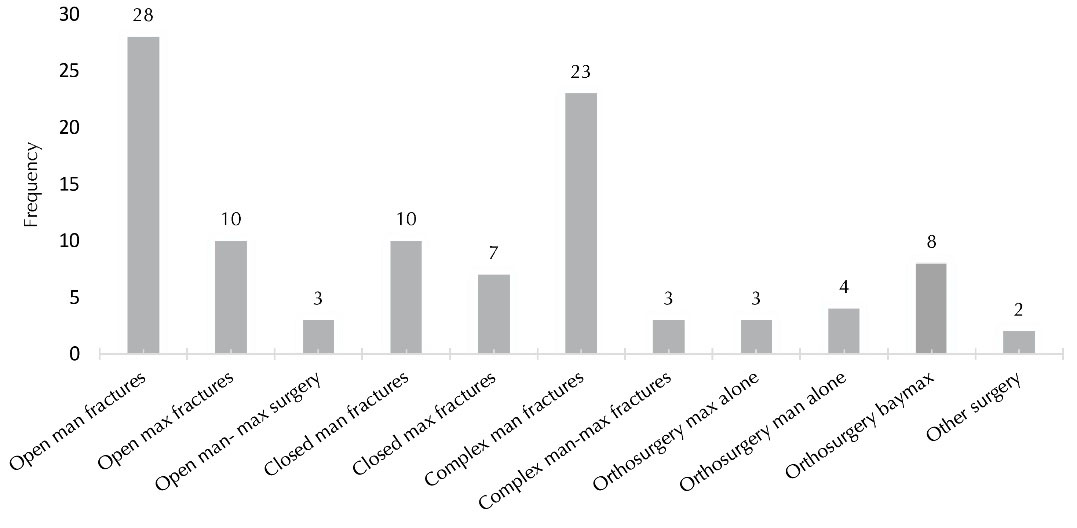
Figure 1.
Frequency Distribution of Different Maxillofacial Surgical Procedures Among 101 Patients. Abbreviations: Man, mandibular; Max, maxillary.
.
Frequency Distribution of Different Maxillofacial Surgical Procedures Among 101 Patients. Abbreviations: Man, mandibular; Max, maxillary.
Electrolyte imbalances were evaluated in 11 maxillofacial surgical procedures and the frequency of electrolyte imbalance was compared among the 11 maxillofacial surgical procedures, indicating no significant correlation between them (Table 1).
Table 1.
Frequency Distribution of Electrolyte Imbalances in Different Types of Maxillofacial Surgeries
|
Type of Maxillofacial Surgery
|
Sodium Imbalances
|
Potassium mbalances
|
Calcium Imbalances
|
Magnesium Imbalances
|
Total %
|
Day1
%
|
Day3
%
|
Day1
%
|
Day3
%
|
Day1
%
|
Day3
%
|
Day1
%
|
Day3
%
|
| Open man fractures |
2 |
5.9 |
1 |
2 |
6.9 |
8.9 |
5.9 |
8.9 |
41.5 |
| Open max fractures |
3 |
2 |
0 |
0 |
2 |
2 |
2 |
1 |
12 |
| Open man- max surgery |
0 |
0 |
0 |
0 |
0 |
1 |
0 |
0 |
1 |
| Closed man fractures |
3 |
1 |
2 |
2 |
3 |
3 |
1 |
1 |
16 |
| Closed max fractures |
1 |
1 |
0 |
0 |
4 |
1 |
1 |
1 |
9 |
| Complex man fractures |
1 |
4.9 |
1 |
0 |
3 |
6.9 |
3 |
1 |
20.8 |
| Complex man-max fractures |
1 |
2 |
0 |
0 |
0 |
0 |
2 |
1 |
6 |
| Orthosurgery max alone |
0 |
0 |
0 |
0 |
1 |
1 |
1 |
1 |
4 |
| Orthosurgery man alone |
2 |
1 |
0 |
0 |
0 |
1 |
0 |
1 |
5 |
| Orthosurgery bimax |
0 |
2 |
0 |
1 |
2 |
2 |
2 |
0 |
9 |
| Other surgery |
1 |
0 |
1 |
0 |
1 |
0 |
0 |
0 |
3 |
Man: mandibular, Max: maxillary
The frequency of electrolyte imbalance among preoperative and postoperative maxillofacial surgery patients are shown in Tables 2 and 3.
Table 2.
Frequency Distribution of Electrolyte Disturbances in Maxillofacial Surgery Patients (Pre-operative, Day 1, and Day 3)
|
Electrolyte imbalance
|
Pre-operative
|
Day 1
|
Day 3
|
|
No.
|
%
|
No.
|
%
|
No.
|
%
|
| Sodium |
Hyponatremia |
6 |
5.9 |
10 |
9.9 |
17 |
16.8 |
| Hypernatremia |
4 |
4.0 |
3 |
3.0 |
3 |
3.0 |
| Potassium |
Hypokalemia |
5 |
5.0 |
4 |
4.0 |
5 |
5.0 |
| Hyperkalemia |
1 |
1.0 |
1 |
1.0 |
0 |
0.0 |
| Calcium |
Hypocalcemia |
14 |
13.9 |
18 |
17.8 |
26 |
25.7 |
| Hypercalcemia |
7 |
6.9 |
5 |
5.0 |
1 |
1.0 |
| Magnesium |
Hypomagnesemia |
4 |
4.0 |
6 |
5.9 |
4 |
4.0 |
| Hypermagnesemia |
13 |
12.9 |
13 |
12.9 |
17 |
16.8 |
Table 3.
Frequency Distribution of Electrolyte Imbalances in Maxillofacial Surgery Patient
|
Electrolyte Imbalance
|
Increasing Imbalances
|
Decreasing Imbalances
|
Total
|
| % |
% |
% |
| Sodium |
18.7 |
3.3 |
22.0 |
| Potassium |
5.3 |
1 |
6.3 |
| Calcium |
26.3 |
1.2 |
27.5 |
| Magnesium |
6 |
16.6 |
22.6 |
Hypocalcemia, hyponatremia, and hypermagnesemia were more common in the maxillofacial surgery patients in preoperative and postoperative settings. To evaluate the effects of surgical procedures on the electrolyte panel, we excluded samples that had preoperative electrolyte abnormalities. Our results showed that, among electrolyte imbalances, hypocalcemia was the most frequent with 26.3%, followed by hyponatremia with 18.7%, and hypermagnesemia with 16.6%, while potassium demonstrated the least amount of change (6.3%) after maxillofacial surgery.
The correlation between electrolyte imbalances (hypo or hyper) and the BMI were evaluated using Spearman correlation coefficient test (Table 4). The results showed a significant correlation between magnesium imbalances and the BMI on the third postoperative day and calcium on the third preoperative day. The results also indicated that a low BMI is associated with magnesium and calcium imbalances on third post-operative day (P < 0.05) (Table 4). Another finding was that patients with hypernatremia and hypercalcemia on first post-operative day had greater BMI (Table 5).
Table 4.
Results ofCorrelation Between Electrolyte Imbalances and the BMIby Day
|
Electrolyte imbalances
|
Pre-operative
|
Day 1
|
Day 3
|
| Na |
r*= 0.060 |
r = -0.110 |
r = -0.027 |
|
P = 0.549 |
P = 0.275 |
P = 0.790 |
| K |
r = -0.021 |
r = 0.172 |
r = -0.056 |
|
P = 0.838 |
P = 0.085 |
P = 0.575 |
| Ca |
r = -0.119 |
r = -0.189 |
r = -0.229 |
|
P = 0.236 |
P = 0.059 |
P
**= 0.021 |
| Mg |
r = -0.040 |
r = -0.122 |
r = -0.214 |
|
P = 0.689 |
P = 0.225 |
P
**= 0.032 |
*Spearman's rho correlation coefficient
**Correlation is significant at the 0.05 level (2-tailed).
Table 5.
Results ofCorrelation Between Type of Electrolyte Imbalances and the BMIby Day
|
|
Pre-operative
|
Day 1
|
Day 3
|
| Na |
r*= -0.035 |
r = 0.251 |
r = 0.131 |
|
P = 0.727 |
P
**= 0.011 |
P = 0.192 |
| K |
r = 0.025 |
r = -0.039 |
r = 0.056 |
|
P = 0.805 |
P = 0.697 |
P = 0.575 |
| Ca |
r = 0.209 |
r = 0.242 |
r = 0.188 |
|
P
**= 0.036 |
P
**= 0.015 |
P = 0.060 |
| Mg |
r= 0.016 |
r = -0.124 |
r = -0.165 |
|
P = 0.874 |
P = 0.216 |
P = 0.100 |
*Spearman's rho correlation coefficient
**Correlation is significant at the 0.05 level (2-tailed).
Discussion
The inorganic electrolytes are important components of body fluid as they play a crucial role in cellular function and survival, excitability of tissues, regulating fluid balance, acid base equilibrium, and many mechanisms associated with life (15). Abnormalities of fluid and electrolyte are very common in patients undergoing surgical procedures. These abnormalities can range from mild, readily correctable deviations to life-threatening ones that demand immediate attention (16). The management of electrolyte imbalances is critical for a comprehensive care of surgical patients. The goal of the postoperative assessment was to confirm proper healing and eliminate complications (16).
Therefore, the aim of this study was to evaluate electrolyte disturbance (potassium, sodium, magnesium, and calcium) among the patients undergoing maxillofacial surgery in which the oral nutrition of the patient was directly or indirectly affected.
This study was performed on 101 patients at Beasat hospital in Hamadan, Iran, who had undergone maxillofacial surgery. The frequency of electrolyte imbalances of sodium, potassium, calcium, and magnesium one day preoperative and three days postoperative were evaluated. The relationship between electrolyte imbalances and BMI, gender, type of etiology, and type of surgery were also assessed.
Our results show that, among electrolyte imbalances, hypocalcemia had the highest frequency (26.3%), followed by hyponatremia (18.7%), and hypermagnesemia (16.6%), while potassium showed the least changes (6.3%) after maxillofacial surgery.
This result was contrary to the results obtained by El-Sherif and Turitto in 2011 (17) and Gennari in 2002 (18) in which hypokalemia was the most common electrolyte abnormality encountered in hospitalized patients.
In a study by Reza Masouleh et al in 2016 (9), electrolyte disorders were evaluated in patients undergoing coronary artery bypass grafting surgery. The results showed that hyponatremia was the most common electrolyte imbalance with 16.7%, followed by hypokalemia with 14.2%. These results are somewhat consistent with our findings regarding postoperative sodium abnormality, but the frequency of hypokalemia was greater compared to our study. This difference could be due to the type of surgery and age of the patients participated in this study.
In a study by Polderman and Girbes in 2004 (1), electrolyte disorders following cardiac surgery were investigated. The results of this study revealed that, after an open heart surgery, 88% of patients showed at least one type of electrolyte disorder. Hypomagnesaemia had the highest frequency, followed by hypocalcemia in the second place among disorders. The results of this study are consistent with our study in term of the occurrence of calcium and magnesium disturbance and the association of these two disorders with each other. However, in our study, the magnesium disturbance was more of an increasing type.
The effect of the BMI on postoperative complications has been assayed in several prior studies. Many studies have shown that there is no statistically significant association between obesity and post-operative complications (19-21). However, they found that obese patients undergoing a surgery were at significantly higher risk of complications (22,23). In the present study, there was a significant correlation between sodium imbalances as hypernatremia on the first day after the operation, and calcium imbalances as hypercalcemia preoperative and third day postoperative with the BMI.
Since the present study was performed within 1 year, we were not able to reach ideal sample size. Consequently, association between electrolyte imbalances and some variables like type of maxillofacial surgery was not accurately evaluated. Because there were discrepancies in the patients’ gender and etiology (trauma, dentofacial deformity and so on), we could not offer correct interpretation about correlation between electrolyte discrepancies and these two variables.
Conclusions
Hypocalcemia, hyponatremia, and hypermagnesemia are relatively common after maxillofacial surgeries. We found that imbalances of calcium and magnesium, two electrolytes that are not measured routinely in pre- and post-operative settings, are more common than the usual analyses of sodium and potassium. Moreover, the findings showed that some factors such as the BMI and kind of maxillofacial surgery could affect electrolyte abnormalities after maxillofacial surgery. BMI above normal limits and jaw trauma could be considered as risk factors and identifying these factors could be useful in planning for prevention, diagnosis, and early treatment of possible complications, which, in turn, may result in an improvement in the quality of care.
Conflict of Interest Disclosures
The authors declare that they have no conflict of interests.
Acknowledgments
This study has been supported by the Hamadan University of Medical Sciences as the thesis of Zohre Mousavie.
Ethical Statement
The present study was approved by Ethics Committee of the Hamadan University of Medical Sciences (IR.UMSHA.REC.13950244).
Authors’ Contributions
OS developed the concept of the study and contributed to the supervision of the project and revision of the paper. ZM contributed to literature search, data collection, and draft writing. MST did the statistical analysis. SMMS controlled hospital checklist and prepared the manuscript. All the authors have read and approved the final manuscript.
References
- Polderman KH, Girbes AR. Severe electrolyte disorders following cardiac surgery: a prospective controlled observational study. Crit Care 2004; 8(6):R459-66. doi: 10.1186/cc2973 [Crossref] [ Google Scholar]
- Kraft MD, Btaiche IF, Sacks GS, Kudsk KA. Treatment of electrolyte disorders in adult patients in the intensive care unit. Am J Health Syst Pharm 2005; 62(16):1663-82. doi: 10.2146/ajhp040300 [Crossref] [ Google Scholar]
- Ducceschi V, D’Andrea A, Liccardo B, Sarubbi B, Ferrara L, Romano GP. Ventricular tachyarrhythmias following coronary surgery: predisposing factors. Int J Cardiol 2000; 73(1):43-8. doi: 10.1016/s0167-5273(99)00224-7 [Crossref] [ Google Scholar]
- Singh RR, Shekhar S, Akhtar MJ, Shankar V. Serum electrolyte changes in major surgical trauma. Int J Res Med Sci 2017; 4(7):2893-6. doi: 10.18203/2320-6012.ijrms20161972 [Crossref] [ Google Scholar]
- Lobo DN, Macafee DA, Allison SP. How perioperative fluid balance influences postoperative outcomes. Best Pract Res Clin Anaesthesiol 2006; 20(3):439-55. doi: 10.1016/j.bpa.2006.03.004 [Crossref] [ Google Scholar]
- Pandey CK, Singh R. Fluid and electrolyte disorders. Indian J Anaesth 2013; 47(5):380-7. [ Google Scholar]
- Braun MM, Barstow CH, Pyzocha NJ. Diagnosis and management of sodium disorders: hyponatremia and hypernatremia. Am Fam Physician 2015; 91(5):299-307. [ Google Scholar]
- Leonard SD, Lee JF. Hyponatremia and Syndrome of Inappropriate Antidiuretic Hormone after Orthopedic Surgery. Proceedings of UCLA Healthcare; 2017. Vol 21.
- Reza Masouleh S, Ahmadi N, Monfared A, Rezasefat A, Kazemnezhad Leili E, Ziaei T. Electrolyte disorders after coronary artery bypass grafting surgery and its related factors. Journal of Holistic Nursing and Midwifery 2016; 25(78):81-90. [ Google Scholar]
- Viera AJ, Wouk N. Potassium disorders: hypokalemia and hyperkalemia. Am Fam Physician 2015; 92(6):487-95. [ Google Scholar]
- Ayach T, Nappo RW, Paugh-Miller JL, Ross EA. Postoperative hyperkalemia. Eur J Intern Med 2015; 26(2):106-11. doi: 10.1016/j.ejim.2015.01.010 [Crossref] [ Google Scholar]
- Bhardwaj B, Desai AD, Patel BM, Parekh CD, Patel SM. Prevalence of hypomagnesemia in patients undergoing gynecological oncology surgery in tertiary care cancer institute of India. Int J Reprod Contracept Obstet Gynecol 2017; 6(10):4355-62. doi: 10.18203/2320-1770.ijrcog20174404 [Crossref] [ Google Scholar]
- Deheinzelin D, Negri EM, Tucci MR, Salem MZ, da Cruz VM, Oliveira RM. Hypomagnesemia in critically ill cancer patients: a prospective study of predictive factors. Braz J Med Biol Res 2000; 33(12):1443-8. doi: 10.1590/s0100-879x2000001200007 [Crossref] [ Google Scholar]
- Brainard BM, Campbell VL, Drobatz KJ, Perkowski SZ. The effects of surgery and anesthesia on blood magnesium and calcium concentrations in canine and feline patients. Vet Anaesth Analg 2007; 34(2):89-98. doi: 10.1111/j.1467-2995.2006.00300.x [Crossref] [ Google Scholar]
- Walker MD. Fluid and electrolyte imbalances: interpretation and assessment. J Infus Nurs 2016; 39(6):382-6. doi: 10.1097/nan.0000000000000193 [Crossref] [ Google Scholar]
- Lowry SF. Fluid, Electrolyte, and Acid-Base Disorders in the Surgery Patient. In: Lowry SF, Ciocca RG, Rettie CS, Vodarsik M, eds. Learning Surgery. New York, NY: Springer; 2005. p. 62-81. 10.1007/0-387-28310-2_4.
- El-Sherif N, Turitto G. Electrolyte disorders and arrhythmogenesis. Cardiol J 2011; 18(3):233-45. [ Google Scholar]
- Gennari FJ. Disorders of potassium homeostasis Hypokalemia and hyperkalemia. Crit Care Clin 2002; 18(2):273-88, vi. doi: 10.1016/s0749-0704(01)00009-4 [Crossref] [ Google Scholar]
- Kamoun S, Alves A, Bretagnol F, Lefevre JH, Valleur P, Panis Y. Outcomes of laparoscopic colorectal surgery in obese and nonobese patients: a case-matched study of 180 patients. Am J Surg 2009; 198(3):450-5. doi: 10.1016/j.amjsurg.2008.09.022 [Crossref] [ Google Scholar]
- Kushnir L, Dunnican WJ, Benedetto B, Wang W, Dolce C, Lopez S. Is BMI greater than 60 kg/m(2) a predictor of higher morbidity after laparoscopic Roux-en-Y gastric bypass?. Surg Endosc 2010; 24(1):94-7. doi: 10.1007/s00464-009-0552-x [Crossref] [ Google Scholar]
- Thomas EJ, Goldman L, Mangione CM, Marcantonio ER, Cook EF, Ludwig L. Body mass index as a correlate of postoperative complications and resource utilization. Am J Med 1997; 102(3):277-83. doi: 10.1016/s0002-9343(96)00451-2 [Crossref] [ Google Scholar]
- Modlin CS, Flechner SM, Goormastic M, Goldfarb DA, Papajcik D, Mastroianni B. Should obese patients lose weight before receiving a kidney transplant?. Transplantation 1997; 64(4):599-604. doi: 10.1097/00007890-199708270-00009 [Crossref] [ Google Scholar]
- Yamamoto S, Hanley E, Hahn AB, Isenberg A, Singh TP, Cohen D. The impact of obesity in renal transplantation: an analysis of paired cadaver kidneys. Clin Transplant 2002; 16(4):252-6. doi: 10.1034/j.1399-0012.2002.01080.x [Crossref] [ Google Scholar]
- Švagždienė M, Širvinskas E. Changes in serum electrolyte levels and their influence on the incidence of atrial fibrillation after coronary artery bypass grafting surgery. Medicina (Kaunas) 2006; 42(3):208-14. [ Google Scholar]