Avicenna J Dent Res. 11(2):53-60.
doi: 10.34172/ajdr.2019.10
Original Article
Evaluation of Dental Anxiety and the Role of Concomitant Factors in Their Anxiety Level in 9-12 years Old Children
Rezvan Rafatjou 1  , Mohammad Ahmadpanah 2
, Mohammad Ahmadpanah 2  , Bahar Ahmadi 3, *
, Bahar Ahmadi 3, *  , Marzieh Mahmoodi 4
, Marzieh Mahmoodi 4 
Author information:
1Assistant Professor, Department of Pediatric Dentistry, Dental School, Hamadan University of Medical Sciences, Hamadan, Iran.
2Associate Professor of Cognitive Science Department of Psychiatry, Hamadan University of Medical Sciences, Hamadan, Iran.
3Resident of Pediatric Dentistry, Dental School, Hamadan University of Medical Sciences, Hamadan, Iran.
4Department of Biostatistics, Bushehr University of Medical Sciences, Bushehr, Iran.
Abstract
Background: Child dental anxiety can be related to poor oral hygiene, along with more missing and decayed teeth. Information on the origin of dental fear and uncooperative behavior in pediatric dentistry is important for behavior management strategy. A limited number of studies have investigated the effects of environmental factors comparatively. Accordingly, the present study aimed to evaluate dental anxiety in children who referred to Hamadan Dental School with respect to such environmental factors during 2018-2019.
Methods: In this cross-sectional study, the level of child dental anxiety was evaluated by the Modified Child Dental Anxiety Scale (MCDAS) and Venham picture test (VPT). The study was conducted on 121 children aged 9-12 years old and the obtained data were statistically analyzed with SPSS 20. In addition, analytical methods such as t test, Freedman test, and independent t test (α=0.05), as well as one-way ANOVA, Kruskal-Wallis, and Mann-Whitney were utilized for analyzing the data. Finally, the correlation between the two questionnaires was measured using the Pearson test.
Results: Tooth extraction and injection in the gum were operated with the highest level of anxiety. The relationship between MCDAS and VPT scores was significant. According to the MCDAS score, having a dental experience was the only factor that was significantly related to child dental anxiety. Based on the VPT score, gender, dental experience, clinic type, and mother’s education level were the variables with a significant relationship with the child dental score.
Conclusions: In general, aggressive dental treatment such as tooth extraction and restoration should be avoided in the first visit of children. The level of dental anxiety among female children was higher compared to male children, therefore, female children need more attention in this regard. Eventually, mothers’ awareness of dental and oral hygiene also plays an important role in reducing the dental anxiety of their children.
Keywords: Dental anxiety, Child, Concomitant factors
Copyright and License Information
© 2019 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Rafatjou R, Ahmadpanah M, Ahmadi B, Mahmoodi M. Evaluation of Rental Anxiety and the Role of Concomitant Factors in Their Anxiety Level in 9-12 years Old Children. Avicenna J Dent Res. 2019;11(2):53-60. doi: 10.15171/ ajdr.2019.10.
Background
Highlights
-
In this study tooth extraction and injection in the gum were operated with the highest level of anxiety
-
In this study the relationship between MCDAS and VPT scores was significant
-
The level of dental anxiety among female children was higher compared to male children
Child dental anxiety is considered as one of the main obstacles against proper dental treatment (1). Although a low level of fear and anxiety is not problematic, an abnormally high level of fear and anxiety can disturb daily functions. Children with extremely high levels of fear and anxiety toward dental treatment commonly have poor oral and dental hygiene because they often refuse to visit dental clinics (2). In addition, evidence has stressed the relationship between dental anxiety and oral hygiene (3). Previous research demonstrated that nine-year-old children have at least one decayed permanent tooth in their mouth and this number increases to 2 for 12-year-old children (4). Further, child dental anxiety can be a reason for the high prevalence of dental caries among children. In this regard, it was concluded that dental fear and anxiety (DFA) are related to more decayed and missing teeth (5).
On the other hand, previous studies have not so far focused on the etiology of child dental anxiety comprehensively. However, Essau and Petermann (6) identified three groups of causes for explaining such phenomenon, including personal factors (e.g., age and mental characteristics), external factors (e.g., the socioeconomic status of the family, racial factors, education, and the like), and dental factors (e.g., dentistry team and pain). Therefore, dentists and society to obtain knowledge about factors that are supposed to affect child dental anxiety. Considering previous controversial results, more studies are needed in this regard. Accordingly, the present study sought to investigate the relationship between child dental anxiety and some social, economic, personal, and family-related factors.
Material and Methods
Data Collection Tools
Several tools were developed to assess participants’ dental anxiety, including Children’s Fear Survey Schedule-Dental Subscale (7), Corah’s Dental Anxiety Scale (8), and Wong-Bakar pain scale (9). The present study utilized the Modified Child Dental Anxiety Scale (MCDAS) (10) and Venham Picture Test (VPT) which is illustrated in Figure 1. Javadinejad et al (11) translated MCDAS into Persian. The scale consists of 8 questions on a 5-point Likert-type scale evaluating the anxiety level of children from different points of view. It must be noted that the last question of this scale was excluded because the nitrous oxide gas is not used for relaxation in dentistry centers supervised by Hamadan University of Medical Sciences. Similarly, Buchanan et al (12) confirmed the validity of VPT. It contains 8 pairs of images representing a child with different emotional states. To conduct this test, the children are asked to mark the most relevant pictures demonstrating their emotions when visiting a dentistry clinic. The higher score indicates that the child is more anxious.
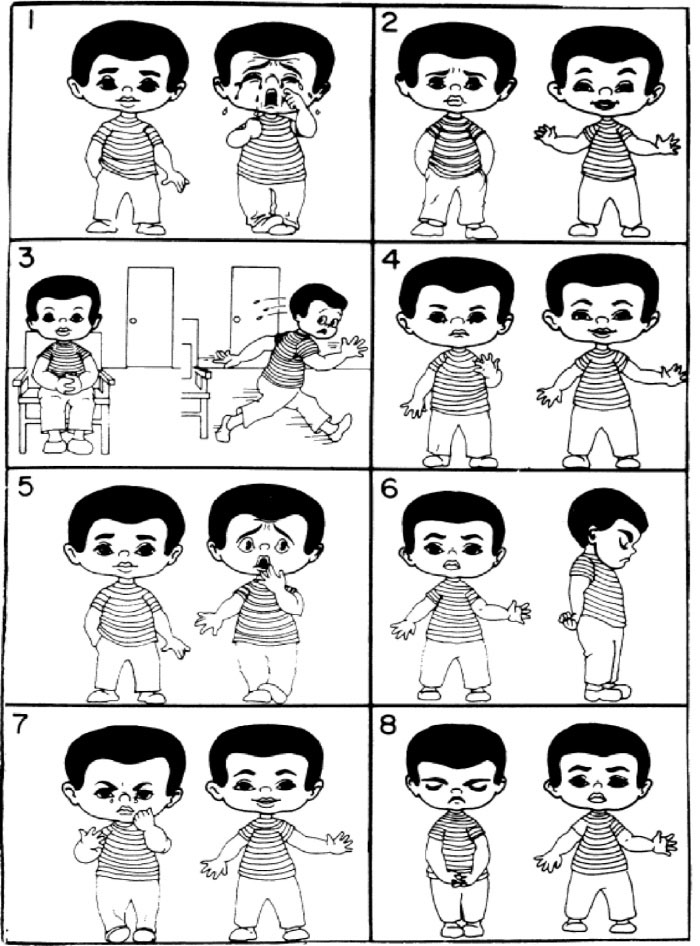
Figure 1.
Venham Picture Test.
.
Venham Picture Test.
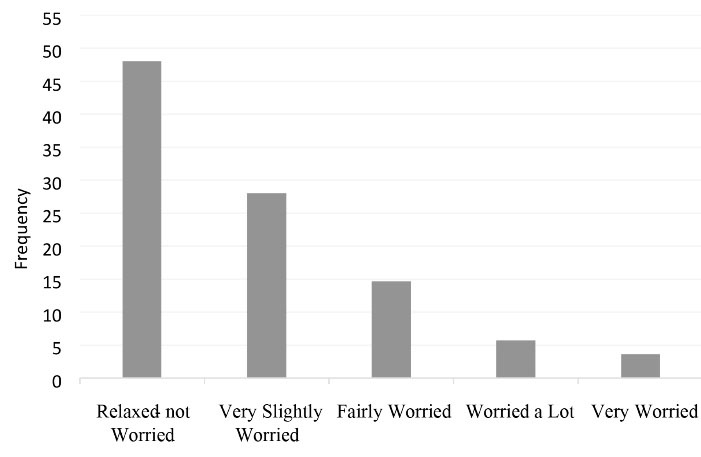
Figure 2.
The Overall Results of Modified Child Dental Anxiety Scale.
.
The Overall Results of Modified Child Dental Anxiety Scale.
Participants
The present cross-sectional study was conducted among children who referred to the Dental Clinic of the Dentistry Faculty of Hamadan University of Medical Sciences during 2015-2016. In general, 121 children within the age range of 9-12 years old were randomly selected to participate in the present study. The inclusion criteria were children who were mentally and physically healthy, had the experience of visiting a dentist, and those cases that their parents filled the contest form. Moreover, it was necessary for the participants to have a knowledge of reading and writing in order to read and answer the questionnaires. The demographic information of children was extracted from their medical records.
Study Variables
As already mentioned, the present study aimed to explore the relationship between child dental anxiety and some personal, economic, and family-related factors such as age, gender, parent’s occupation, parent’s education level, the type of clinic (private or public), the type of dental specialist, medical experience, dental experience, as well as the social-economic level of the family and birth order.
Statistical Analyses
The lowest required sample size for questionnaire-based studies is five to ten samples for each question. However, the lowest number of required samples should not be lower than one hundred when the number of questions is lower than 15 (13). Accordingly, the sample size was determined to be 121 in the present study. The data were analyzed using SPSS software, version 20 at the 0.05 level of significance.
Likewise, various statistical tests were utilized based on the nature of variables. The relationship between age and the anxiety level was examined using the Pearson correlation coefficient. Furthermore, the Spearman correlation coefficient was applied to assess the relationship between VPT score and age. Other examinations were performed using independent pairwise t test and ANOVA. It is worth mentioning that the normality of data and the equality of variances were evaluated using the Kolmogorov-Smirnov and the Levene tests, respectively. Finally, the Mann-Whitney and Kruskal-Wallis tests were employed for those cases the data of which failed to follow a normal curve.
Results
Table 1 presents demographic information of children who participated in the present study. As shown, 45.5% of them were males and the remaining participants were females. Furthermore, most participants were nine years old and the first child of their families. The information about the other study variables such as parent’s occupation, parent’s education level, and the socioeconomic status of children’s families are summarized as well.
Table 1.
Demographic Information of Study Participants
|
Variable
|
State
|
No. (%)
|
| Gender |
Male |
55 (45.5) |
| Female |
66 (54.4) |
| Age |
9 |
62 (51.7) |
| 10 |
31 (25.8) |
| 11 |
14 (11.7) |
| 12 |
13 (10.8) |
| Birth order |
First |
72 (59.5) |
| Second |
38 (31.4) |
| Third or older |
11 (9.1) |
| Father’s occupation |
Worker |
5 (4.2) |
| Self-employed |
66 (55.5) |
| Civil servant |
48 (40.3) |
| Mother’s occupation |
Housewife |
92 (76) |
| Self-employed |
2 (1.7) |
| Civil servant |
27 (22.3) |
| Father’s education level |
Primary and lower |
14 (12.2) |
| Secondary and diploma |
51 (44.3) |
| Academic (bachelor) |
31 (27) |
| Mater or higher |
19 (16.5) |
| Mother’s education level |
Primary and lower |
16 (13.6) |
| Secondary and diploma |
66 (55.9) |
| Academic (bachelor) |
23 (19.5) |
| Mater or higher |
13 (11) |
| Socio-economic status of family |
Poor |
19 (16.8) |
| Moderate |
57 (50.4) |
| Rather high |
24 (21.2) |
| High |
13 (11.5) |
The results of assessing child dental anxiety based on MCDAS are provided in Table 2. Based on the data, tooth extraction was the most fear-inducing operation during which 15.7% of participants were very worried, followed by the injection in the gum. In contrast, looking at teeth and “being put to sleep for treatment” were among the operations with the least perceived fear.
Table 2.
Participants’ Responses to MCDAS
|
Items
|
Responses
|
|
Relaxed-not Worried
|
Very Slightly Worried
|
Fairly Worried
|
Worried a lot
|
Very Worried
|
| “Going to the dentist” |
56 (46.7%) |
39 (32.5%) |
20 (16.7%) |
4 (3.3%) |
1 (0.8%) |
| “Having your teeth looked at” |
81 (67.5%) |
29 (24.2%) |
8 (6.7%) |
1 (0.8%) |
1 (0.8%) |
| “Having your teeth scraped and polished” |
78 (65.5%) |
25 (21%) |
11 (9.2%) |
4 (3.4%) |
1 (0.8%) |
| “Having an injection in the gum” |
37 (30.6%) |
43 (35.5%) |
27 (22.3%) |
7 (5.8%) |
7 (5.8%) |
| “Having a filling” |
48 (41%) |
33 (28.2%) |
27 (23.1%) |
8 (8.6%) |
1 (0.9%) |
| Having a tooth taken out” |
30 (57.9%) |
31 (27.3%) |
18 (9.1%) |
18 (15.7%) |
18 (15.7%) |
| “Being put to sleep to have treatment” |
70 (62.5%) |
33 (26.8%) |
11 (8.9%) |
6 (5%) |
1 (%0.8) |
Note. MCDAS: Modified child dental anxiety scale.
The overall results of MCDAS are demonstrated in Figure 1. As shown, more than 45% of participants had no fear of facing a dentistry clinic while lower than 5% experienced the highest level of fear in this regard.
Table 3 also represents the results of the VPT test. Based on the data, picture 2 received the highest score of sadness, followed by picture 4.
Table 3.
Participants’ Responses to VPT
|
Item
|
Response
|
|
Happy
|
Sad
|
| Picture 1 |
111 (92.5%) |
9 (7.5%) |
| Picture 2 |
91 (76.5%) |
28 (23.5%) |
| Picture 3 |
116 (97.5%) |
3 (2.5%) |
| Picture 4 |
96 (80%) |
24 (20%) |
| Picture 5 |
98 (81.7%) |
22 (18.3%) |
| Picture 6 |
115 (95.8%) |
5 (4.2%) |
| Picture 7 |
105 (88.2%) |
14 (11.8%) |
| Picture 8 |
109 (90.8%) |
11 (9.2%) |
Note. VPT, Venham picture test.
Spearman correlation test was utilized to assess the association of the obtained anxiety scores by MCDAS and VPT. The results revealed that there was a significant correlation between the scores of the two questionnaires (P= 0.0001).
Moreover, Table 4 demonstrates the association between MCDAS score and other variables of the study. As explained earlier, various statistical tests were utilized based on the nature of variables. The types of these tests are presented as well. Based on the results, having an experience of dental treatment was the only variable with a significant association with the MCDAS score.
Table 4.
Correlation Between MCDAS Score and Other Variables
|
|
Variables
|
Statistical Test
|
P value
|
| MCDAS score |
Age |
Pearson correlation |
0.251 |
| Treatment |
Pearson correlation |
0.921 |
| Gender |
Pairwise t-test |
0.125 |
| Medical experience |
Pairwise t-test |
0.728 |
| Dental experience |
Pairwise t-test |
0.043 |
| Clinic type |
Pairwise t-test |
0.423 |
| Type of dental specialist |
Pairwise t-test |
0.723 |
| Birth order |
Spearman correlation |
0.731 |
| Father’s occupation |
ANOVA |
0.833 |
| Mother’s occupation |
ANOVA |
0.736 |
| Father’s education level |
ANOVA |
0.428 |
| Mother’s education level |
ANOVA |
0.703 |
| Socio-economic status of the family |
ANOVA |
0.360 |
Note. MCDAS: Modified child dental anxiety scale; ANOVA: Analysis of variance.
Likewise, the association between child dental anxiety based on the VPT score and the other variables is presented in Table 5. Accordingly, gender, dental experience, type of clinic, and mother’s education level were the variables with a significant relationship with child dental anxiety based on the VPT score.
Table 5.
Correlation Between VPT Score and Other Variables
|
|
Variables
|
Statistical Test
|
P Value
|
| VPT score |
Age |
Spearman correlation |
0.953 |
| Treatment |
Spearman correlation |
0.222 |
| Gender |
Mann-Whitney |
0.011 |
| Medical experience |
Mann-Whitney |
0.162 |
| Dental experience |
Mann-Whitney |
0.035 |
| Clinic type |
Mann-Whitney |
0.029 |
| Type of dental specialist |
Mann-Whitney |
0.561 |
| Birth order |
Spearman correlation |
0.109 |
| Father’s occupation |
Kruskal-Wallis |
0.995 |
| Mother’s occupation |
Kruskal-Wallis |
0.184 |
| Father’s education level |
Kruskal-Wallis |
0.386 |
| Mother’s education level |
Kruskal-Wallis |
0.028 |
| Socio-economic status of family |
Kruskal-Wallis |
0.365 |
Note. VPT: Venham picture test.
Discussion
The present study was conducted to assess the level of dental anxiety among children who attended the Dentistry Clinic of Hamadan University of Medical Sciences during 2015-2016.
The level of dental anxiety was measured using two instruments (i.e., VPT and MCDAS), which were proven to be valid and reliable tools in this regard (11,12).
As previously explained, a total number of 121 children aged between 9 and 12 years old were randomly selected for investigation.
According to the results of the present study, tooth extraction and injection in the gum were the most anxious-inducing operations, which is in line with the results of some previous studies such as Nilchiyan & Mohammadi (14) and Paryab & Hosseinbor (15), as well as Lee et al (16), and Alsarheed (17). Such operations are normally accompanied by pain and have an aggressive nature.
Moreover, most children received no fear when visiting dental clinics or undergoing dental operations. The findings are in conformity with the results of Nilchiyan and Mohammadi (14).
However, the results contradict the results of Salem et al (18) whose participants were of lower ages. Children at lower ages have no distinct perception of fear and rarely have a dental experience. It is believed that dental anxiety decreases as the children grow older.
Based on the results, no significant relationship was observed between age and perceived anxiety in the present study. This finding corroborates with the result of Saatchi et al (19). All the above-mentioned studies were conducted on children aged near ten or higher who learned to adjust themselves to stressful situations. Younger children tend to admit their fears more freely than older ones. It is part of the normal growth process in preschool children to be afraid of unknown situations and people. New abilities develop as the child’s age increases, and the child feels more confident, has more self-control, and gets ready to face social environments (20).
Miron and Colosi (21) explained that child dental anxiety has a root in physiological issues rather than psychological matters, therefore, children’s age cannot play a great role in this regard. Contrarily, some studies concluded that children’s age has a prominent effect on dental anxiety (18,22). To evaluate the relationship between age and child dental anxiety, the study sample should be taken from a wider range of age. Studies conducted on a wide range of ages commonly reported a significant relationship between these two parameters. For example, Suprabha et al. (22) conducted a study on children aged between 7 and 14 years old and found a significantly higher level of dental anxiety among children aged 7-10 years old compared to those who were within the age range of 11-14 years old. As previously mentioned, children at lower ages have no distinct perception toward fear and rarely have a dental experience while during older ages, they learn to adjust themselves to various unpleasant conditions and normally have a dental experience. In this regard, it was reported that people aged 20-29 years old have the least dental anxiety (23).
In the present study, a significant relationship was observed between gender and dental anxiety. This finding is in line with the results of several studies (4,14,18,23). However, some other studies reported no relationship between these 2 variables (16,24,25). On the other hand, the results of a study performed in Africa showed no significant difference between the level of dental anxiety among girls and boys (26). It seems that cultural and social issues play a role in this regard (27). Socialization process and the establishment of cultural rules and patterns in older children led the boys to be more restricted to report subjective feelings like dental pain or dental fear while the social pressure for girls is in the other direction (20). Biological differences between female and male children can also be another reason why they perceived different levels of dental anxiety (25).
In addition, physiological emotions such as stress, depression, fear, and social phobia are more prevalent in women than men and dental anxiety may be related to such emotions (28). Moreover, females are more open to declare their emotions than males (29). In agreement with most, but not all studies, DFA decrease by an increase in age (30).
Another finding of the present study was the significant relationship between mother’s education level and dental anxiety based on the VPT score. This finding is in line with the results of Blackwell (31). In other words, educated mothers are more able to inform their children about dental treatments and to calm them down when facing such situations. Additionally, these mothers may be more careful about the oral and dental hygiene of their children so that their children visit dentists periodically and such experiences would gradually reduce the child dental anxiety (32).
Contrarily, no significant relationship was observed between the socioeconomic status of family and child dental anxiety, which is consistent with the findings of some previous studies (18,33). However, the results of one study demonstrated that child dental anxiety is more prevalent among immigrants and families with sub-standard socioeconomic status (34). The socioeconomic position is evidenced as a strong marker for health indicators and those with more deprivation exhibit worse general and oral health conditions. Similarly, children from poorer families have less access to dental care and thus experience higher loads of dental diseases, contributing probably to higher loads of dental fear (20).
Having a negative dental experience was significantly related to the child dental anxiety measured by both VPT and MCDAS instruments, which is in agreement with the findings of Suprabha et al (22) and Saatchi et al (19). In addition, a negative experience or an inadequate first dental visit during childhood can lead a grown person to present high levels of dental fear (20). The motivation for the first dental attendance can be decisive for the development of fear. If this first visit happens for preventive procedures, the prevalence of dental fear seems to be lower compared to when the dental visit is for emergency or curative procedures (20). If children have a painful dental experience, they would be anxious in the following visits. Therefore, considering the inhibition theory is very useful in this regard. According to this theory, children should have a neutral dental experience (e.g., examination) before undergoing any aggressive treatment such as tooth extraction or restoration (35).
These aspects reinforce the importance of early dental attention, preventing dental caries and, consequently, dental fear and the avoidance of dental appointments (20).
Further, dental fear decreases by increasing the number of dental visits. This finding should not be attributed to children’s age, The relation between dental fear and previous dental experience is still controversial (36). Although some studies found no difference in terms of DFA in children with or without previous dental experience, at least, the results of one study demonstrated that children with previous dental experience have significantly lower DFA (30).
It is important to maintain a balance between the duration of the procedure and efficient behavior management with respect to child patients. Shorter appointments are suggested as a cooperation-enhancing approach for pediatric dental patients. Furthermore, children usually interpret longer treatment sessions as a sign of major problems that might cause significant anxiety leading to the development of behavioral management problems (7,37,38).
According to the VPT results, the relationship between the type of dental clinic and dental anxiety was also significant so that the level of dental anxiety was higher in private clinics than public clinics. Well-trained and experienced pediatric dentists may be more efficient in providing treatment in a shorter course and with the least traumatic approaches which significantly contribute to children’s behaviors during and after treatment (36).
Public dental clinics normally have more visitors thus children can play with each other before the treatment leading to a reduction in their stress and anxiety. In the present study, no significant correlation was observed between the child dental anxiety and the other variables such as birth order, the type of dental specialist, and the medical experience of children, which is in line with the results of some previous studies (15,22).
Conclusions
In general, aggressive dental treatment such as tooth extraction and tooth restoration should be avoided in the first visit of children. Based on the results, the level of dental anxiety among female children was higher than male children, therefore, female children need more attention in this regard. Mothers’ awareness of dental and oral hygiene also plays an important role in reducing the dental anxiety of their children.
Conflict of Interest Disclosures
The authors declare that there is no conflict of interest.
Authors’ Contribution
All authors have contributed to the conception and design of the study. RR and MA supervised the conduct of the experiment. BA contributed to the data collection. The statistical analyses and interpretation of data were carried out by BA and MM.BA and RR drafted the manuscript. All the authors critically revised the manuscript for intellectual content and finally and approved the final version of the manuscript.
Ethical Statement
All steps of the study were approved by the Ethics Committee of Hamadan University of Medical Sciences. The parents of children filled out the consent form for their children participation in the study..
References
- Farokhgisour E, Hashemipour M, Ajdari H. The influence of music on pain sensation and fear in children during dental treatments. J Dent (Shiraz) 2008; 9(1):93-100. [ Google Scholar]
- Hakeberg M, Berggren U, Gröndahl HG. A radiographic study of dental health in adult patients with dental anxiety. Community Dent Oral Epidemiol 1993; 21(1):27-30. doi: 10.1111/j.1600-0528.1993.tb00714.x [Crossref] [ Google Scholar]
- Eitner S, Wichmann M, Paulsen A, Holst S. Dental anxiety--an epidemiological study on its clinical correlation and effects on oral health. J Oral Rehabil 2006; 33(8):588-93. doi: 10.1111/j.1365-2842.2005.01589.x [Crossref] [ Google Scholar]
- Rezaei-Soufi L, Kasraei S, Jazaeri M, Khamverdi Z. Dental caries experience in 13‒19-year-old Iranian students expressed by DMFT and significant caries index. Avicenna J Dent Res 2011; 3(2):45-52. [ Google Scholar]
- Armfield JM, Slade GD, Spencer AJ. Dental fear and adult oral health in Australia. Community Dent Oral Epidemiol 2009; 37(3):220-30. doi: 10.1111/j.1600-0528.2009.00468.x [Crossref] [ Google Scholar]
- Essau CA, Petermann F. Anxiety disorders in children and adolescents: epidemiology, risk factors and treatment. Routledge; 2013.
- Nakai Y, Hirakawa T, Milgrom P, Coolidge T, Heima M, Mori Y. The children’s fear survey schedule-dental subscale in Japan. Community Dent Oral Epidemiol 2005; 33(3):196-204. doi: 10.1111/j.1600-0528.2005.00211.x [Crossref] [ Google Scholar]
- Jain M, Tandon S, Sharma A, Jain V, Rani Yadav N. Cross-Cultural adaption, validity and reliability of a Hindi version of the Corah’s Dental Anxiety Scale. Health Promot Perspect 2018; 8(2):120-6. doi: 10.15171/hpp.2018.15 [Crossref] [ Google Scholar]
- Wong DL, Hockenberry-Eaton M, Wilson D, Winkelstein M, Schwartz P. Wong-Baker faces pain rating scale. Home Health Focus 1996; 2(8):62. [ Google Scholar]
- Howard KE, Freeman R. Reliability and validity of a faces version of the Modified Child Dental Anxiety Scale. Int J Paediatr Dent 2007; 17(4):281-8. doi: 10.1111/j.1365-263X.2007.00830.x [Crossref] [ Google Scholar]
- Javadinejad S, Farajzadegan Z, Sherkat S, Shokri Mozhdehi M. Reliability and Validity of the modified retranslated persian version of child dental anxiety scale in comparison with corah’s dental anxiety scale and Venham picture test. Journal of Research in Dental Sciences 2014; 11(2):112-5. [ Google Scholar]
- Buchanan H, Niven N. Validation of a Facial Image Scale to assess child dental anxiety. Int J Paediatr Dent 2002; 12(1):47-52. [ Google Scholar]
- de Vet HC, Adèr HJ, Terwee CB, Pouwer F. Are factor analytical techniques used appropriately in the validation of health status questionnaires? a systematic review on the quality of factor analysis of the SF-36. Qual Life Res 2005; 14(5):1203-18. doi: 10.1007/s11136-004-5742-3 [Crossref] [ Google Scholar]
- Nilchiyan F, Mohammadi A. Assessment of the level of dental anxiety in 10-12 year-old students in Shahr-e-kord city in 2012. Journal of Isfahan Dental School 2013; 9(5):451-8. [ Google Scholar]
- Paryab M, Hosseinbor M. Dental anxiety and behavioral problems: a study of prevalence and related factors among a group of Iranian children aged 6-12. J Indian Soc Pedod Prev Dent 2013; 31(2):82-6. doi: 10.4103/0970-4388.115699 [Crossref] [ Google Scholar]
- Lee CY, Chang YY, Huang ST. The clinically related predictors of dental fear in Taiwanese children. Int J Paediatr Dent 2008; 18(6):415-22. doi: 10.1111/j.1365-263X.2008.00924.x [Crossref] [ Google Scholar]
- Alsarheed M. Children’s perception of their dentists. Eur J Dent 2011; 5(2):186-90. [ Google Scholar]
- Salem K, Kousha M, Anissian A, Shahabi A. Dental fear and concomitant factors in 3-6 year-old children. J Dent Res Dent Clin Dent Prospects 2012; 6(2):70-4. doi: 10.5681/joddd.2012.015 [Crossref] [ Google Scholar]
- Saatchi M, Abtahi M, Mohammadi G, Mirdamadi M, Binandeh ES. The prevalence of dental anxiety and fear in patients referred to Isfahan Dental School, Iran. Dent Res J (Isfahan) 2015; 12(3):248-53. [ Google Scholar]
- Silveira ERD, Goettems ML, Demarco FF, Azevedo MS. Clinical and Individual Variables in Children’s Dental Fear: A School-Based Investigation. Braz Dent J 2017; 28(3):398-404. doi: 10.1590/0103-6440201601265 [Crossref] [ Google Scholar]
- Miron C, Colosi HA. Work stress, health behaviours and coping strategies of dentists from Cluj-Napoca, Romania. Int Dent J 2018; 68(3):152-61. doi: 10.1111/idj.12361 [Crossref] [ Google Scholar]
- Suprabha BS, Rao A, Choudhary S, Shenoy R. Child dental fear and behavior: the role of environmental factors in a hospital cohort. J Indian Soc Pedod Prev Dent 2011; 29(2):95-101. doi: 10.4103/0970-4388.84679 [Crossref] [ Google Scholar]
- Oktay EA, Koçak MM, Şahinkesen G, Topçu FT. The role of age, gender, education and experiences on dental anxiety. Gülhane Tıp Derg 2009; 51:145-8. [ Google Scholar]
- Jones LM, Buchanan H. Assessing children’s dental anxiety in New Zealand. N Z Dent J 2010; 106(4):132-6. [ Google Scholar]
- Kyritsi MA, Dimou G, Lygidakis NA. Parental attitudes and perceptions affecting children’s dental behaviour in Greek population A clinical study. Eur Arch Paediatr Dent 2009; 10(1):29-32. [ Google Scholar]
- Folayan MO, Idehen EE, Ufomata D. The effect of sociodemographic factors on dental anxiety in children seen in a suburban Nigerian hospital. Int J Paediatr Dent 2003; 13(1):20-6. doi: 10.1046/j.1365-263x.2003.00411.x [Crossref] [ Google Scholar]
- Folayan MO, Idehen EE, Ojo OO. The modulating effect of culture on the expression of dental anxiety in children: a literature review. Int J Paediatr Dent 2004; 14(4):241-5. doi: 10.1111/j.1365-263X.2004.00563.x [Crossref] [ Google Scholar]
- Ritsner M, Ponizovsky A, Nechamkin Y, Modai I. Gender differences in psychosocial risk factors for psychological distress among immigrants. Compr Psychiatry 2001; 42(2):151-60. doi: 10.1053/comp.2001.19750 [Crossref] [ Google Scholar]
- Dohrenwend BP, Dohrenwend BS. Social and cultural influences on psychopathology. Annu Rev Psychol 1974; 25:417-52. doi: 10.1146/annurev.ps.25.020174.002221 [Crossref] [ Google Scholar]
- Paglia L, Gallus S, de Giorgio S, Cianetti S, Lupatelli E, Lombardo G. Reliability and validity of the Italian versions of the Children’s Fear Survey Schedule - Dental Subscale and the Modified Child Dental Anxiety Scale. Eur J Paediatr Dent 2017; 18(4):305-12. doi: 10.23804/ejpd.2017.18.04.08 [Crossref] [ Google Scholar]
- Blackwell DL. Family structure and children’s health in the United States: findings from the National Health Interview Survey, 2001-2007. Vital Health Stat 10. 2010(246):1-166.
- Goyal J, Menon I, Singh RP, Sharma A, Passi D, Bhagia P. Association between maternal dental anxiety and its effect on the oral health status of their child: An institutional cross sectional study. J Family Med Prim Care 2019; 8(2):535-8. doi: 10.4103/jfmpc.jfmpc_415_18 [Crossref] [ Google Scholar]
- Ramos-Jorge J, Marques LS, Homem MA, Paiva SM, Ferreira MC, Oliveira Ferreira F. Degree of dental anxiety in children with and without toothache: prospective assessment. Int J Paediatr Dent 2013; 23(2):125-30. doi: 10.1111/j.1365-263X.2012.01234.x [Crossref] [ Google Scholar]
- Arnrup K, Broberg AG, Berggren U, Bodin L. Temperamental reactivity and negative emotionality in uncooperative children referred to specialized paediatric dentistry compared to children in ordinary dental care. Int J Paediatr Dent 2007; 17(6):419-29. doi: 10.1111/j.1365-263X.2007.00868.x [Crossref] [ Google Scholar]
- Pai R, Mandroli P, Benni D, Pujar P. Prospective analysis of factors associated with dental behavior management problems, in children aged 7-11 years. J Indian Soc Pedod Prev Dent 2015; 33(4):312-8. doi: 10.4103/0970-4388.165684 [Crossref] [ Google Scholar]
- Jamali Z, Najafpour E, Ebrahim Adhami Z, Sighari Deljavan A, Aminabadi NA, Shirazi S. Does the length of dental procedure influence children’s behavior during and after treatment? a systematic review and critical appraisal. J Dent Res Dent Clin Dent Prospects 2018; 12(1):68-76. doi: 10.15171/joddd.2018.011 [Crossref] [ Google Scholar]
- Bastos JL, Peres MA, Peres KG, Araujo CL, Menezes AM. Toothache prevalence and associated factors: a life course study from birth to age 12 yr. Eur J Oral Sci 2008; 116(5):458-66. doi: 10.1111/j.1600-0722.2008.00566.x [Crossref] [ Google Scholar]
- Goettems ML, Correa MB, Vargas-Ferreira F, Torriani DD, Marques M, Domingues MR. Methods and logistics of a multidisciplinary survey of schoolchildren from Pelotas, in the Southern Region of Brazil. Cad Saude Publica 2013; 29(5):867-78. doi: 10.1590/S0102-311X2013000500005 [Crossref] [ Google Scholar]