Avicenna J Dent Res. 11(3):104-107.
doi: 10.34172/ajdr.2019.20
Case Report
A Rare Gingivobuccal Complex Cancer in a Pediatric patient: A Case Report
Shishir Mohan Devki 1  , Venkatesh Balaji Hange 2, *
, Venkatesh Balaji Hange 2, * 
Author information:
1Head of Department, Department of Oral and Maxillofacial Surgery, K.D. Dental College and Hospital, Mathura, Uttar Pradesh, India
2Postgraduate Student, Department of Oral and Maxillofacial Surgery, K.D. Dental College and Hospital, Mathura, Uttar Pradesh, India
Abstract
Squamous cell carcinoma (SCC) of the oral cavity ranks as the 12th most common cancer in the world and the 8th most frequent cancer in males. Oral cavity SCC (OCSCC) is extremely unusual in the pediatric population. Researchers believe that the pathology of SCC in pediatric patients is a separate entity different from SCC in the adult population. SCC is a malignant and clinically variable epithelial neoplasm. When located in the gingiva, this neoplasm may mimic common inflammatory lesions. This neoplasm is generally more frequent in males than in females, but this is not observed in cases of SCC located in the gingiva. Usual risk factors such as tobacco and alcohol exposure are typically absent.
Keywords: Pediatric cancer, Gingivobuccal complex, Gingival neoplasms, Carcinoma, Oral
Copyright and License Information
© 2019 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Devki SM, Hange VB. A Rare Gingivobuccal Complex Cancer in a Pediatric patient: A Case Report. Avicenna J Dent Res. 2019;11(3):104-107. doi: 10.34172/ajdr.2019.20
Background
Highlights
Oral cavity squamous cell carcinoma (OCSCC) is rare in pediatric patients (defined by the American Academy of Pediatrics as patients under the age of 21), affecting approximately 1 in 1000 cases. OCSCC in pediatric patients is believed to be etiologically distinct from OCSCC in adults (1-4). Squamous cell carcinoma (SCC) of the oral cavity ranks as the 12th most common cancer in the world and the 8th most frequent cancer in males (1). There are no universally accepted treatment guidelines due to the rarity of pediatric head and neck cancers.
Approximately 10% of the malignant oral tumors exist in the gingiva, and tumors are more common in edentulous regions, even if they may appear in regions with teeth. Bhanu Prasad et al revealed a favorable survival for patients treated with surgery alone or surgery followed by adjuvant radiation. The patterns of care delivered in their study also reflected those of adult patients with head and neck SCC (5).
SCC is a malignant neoplasm with varying clinical manifestations. When located in the gingiva, this neoplasm may mimic common inflammatory lesions. This neoplasm is generally more frequent in male than in female, but this is not observed in cases of SCC located in the gingiva (3).
The clinical presentation of SCC in the gingiva can be quite variable, appearing as a region of ulceration or as an exophytic, granular or verruciform development. It may not clinically resemble a malignant tumor at all and may present as an endoperiodontal lesion, gingival erythema, or as a painless, asymptomatic, and elevated lesion (6). SCC of the gingiva is normally painless and it is located in the keratinized portion. In advanced stages, it is aggressive and has easy access to infratemporal fossa (3,7).
Malnutrition may be the causative factor in the development of OSCC when factors such as hepatic and pulmonary diseases are ruled out.
Case Report
A 14–year-old female patient referred to the Department of Oral and Maxillofacial Surgery K.D., Dental College and Hospital, Mathura. The chief complaints included painless swelling and bleeding in gingiva for 6 months which gradually increased to the present size. The patient gave a history of pain for 10 days for which the patient had sought treatment. The pain was mild to moderate, continuous in nature.
On the examination, the lesion (Figure 1) was round circular gingival swelling which was soft in consistency, slow-growing neoplasm seen in the upper right quadrant of the mouth. Facial asymmetry and bulge were seen on the right side of the face, causing elevation of the upper lip on the right side. The patient was aware of this swelling for 6 months. The swelling was roughly 1.5 × 4 cm in size with ill-defined margins and border, ulcerated surface along with tiny bleeding points. The patient revealed that bleeding became more frequent upon brushing in the region of lesion 10 days before the examination. The patient did not give any history of any kind of deleterious oral habit. Her family history was unremarkable. Clinically, the lesion appeared to be a benign soft tissue tumor with a provisional diagnosis of peripheral giant cell granuloma. Pre-surgical investigations that were carried out were found to be within the normal range. A full hemogram was requested, the blood investigation report was within the normal range except for the sedimentation level of erythrocytes, which was slightly elevated. To rule out metastasis in the lung, a chest X-ray was advised and was found to be clear. Intra-oral periapical radiograph (Figure 2) and orthopantomograph (Figure 3) did not reveal any significant bone loss in relation to the maxillary right anterior teeth or bone. As there was a possibility of a neoplasmic lesion, an excisional biopsy was planned (Figure 4). Intra-operatively involved teeth and bone were also removed along with the gingival neoplasm (Figure 5) for histopathological examination under general anaesthesia. Healing was found to be unsatisfactory. After confirmation of SCC of the gingiva by histopathological examination, the patient referred to a nearby cancer institute for definitive treatment. Given that gingival cancer is rare in maxillary gingiva and common in mandibular gingiva, the appearance of this neoplasm in population below 15 years of age in maxillary region is rare and was reported in very few studies till now.

Figure 1.
Gingivobuccal Complex Cancer Resembling Benign Inflammatory Lesion.
.
Gingivobuccal Complex Cancer Resembling Benign Inflammatory Lesion.

Figure 2.
The IOPA Radiograph Iindicating no Significant Bone Loss in the Region of Gingivobuccal Complex Cancer.
.
The IOPA Radiograph Iindicating no Significant Bone Loss in the Region of Gingivobuccal Complex Cancer.

Figure 3.
Orthopantomograph Showing no Significant Bone Loss in the Region of Gingivobuccal Complex Cancer.
.
Orthopantomograph Showing no Significant Bone Loss in the Region of Gingivobuccal Complex Cancer.

Figure 4.
Excisional Biopsy Performed to Remove Neoplasm and the Involved Bone and Teeth.
.
Excisional Biopsy Performed to Remove Neoplasm and the Involved Bone and Teeth.
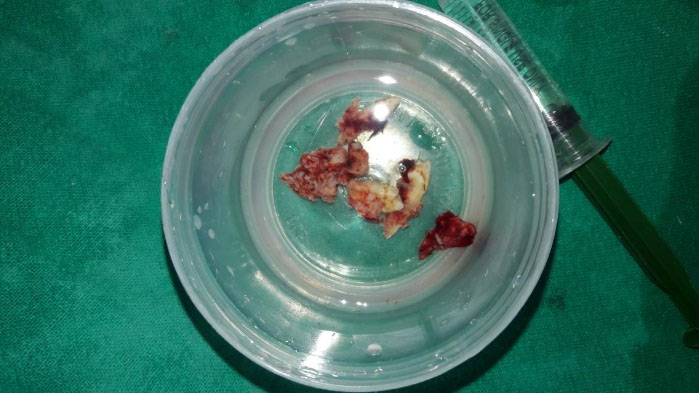
Figure 5.
Excised Specimen of Gingivobuccal Complex Cancer Including Neoplasm and the Involved Bone and Teeth.
.
Excised Specimen of Gingivobuccal Complex Cancer Including Neoplasm and the Involved Bone and Teeth.
Discussion
SCC is the most common malignant neoplasm of the mouth, accounting for 96% of all malignant tumors in this area. SCC influences Caucasian males over 40 years of age in particular and is highly uncommon in young patients (3). If lip vermilion carcinoma is excluded, the lateral/ventral tongue and mouth floor are the most prevalent sites of intraoral SCC. Gingiva, however, is the next most prevalent location for intraoral SCC, representing between 14% and 22% of all cases (6-8). Many clinicians believe that young patients suffer from this illness in particular and are associated with poorer survival than adults (4).
Generally, malignant mucosal lesions are not frequent in pediatric population. Due to the rarity of oral cavity malignancies in pediatric patients, the differential diagnosis of SCC is often not regarded. SCC accounts for less than 2% of all malignancies of the head and neck in the pediatric population. The pediatric SCC is even rarer, with very few cases of pediatric oral SCC reported in the medical literature, especially in people with <15 years of age (2,7-8).
In some cases of pediatric SCC, a contributing risk factor could be a genetic disorder such as Fanconi anemia, xeroderma pigmentosum, keratosis-ichthyosis-deafness (KID) syndrome, or an unknown genetic risk factor. A secondary malignancy following chemotherapy or radiotherapy would be less prevalent (4,9).
Other factors in the pediatric population are reported to be associated with an enhanced risk of oral cavity SCC; however, there is conflicting proof to support these factors. These factors include polyvinyl chloride (found in plastics), Epstein-Barr virus, and human papillomavirus (7,10). It is also common for gingiva carcinoma to metastasize to mandibular gingiva carcinoma than maxillary gingival tumors (6,11).
Histopathological examination revealed hyperkeratinized stratified squamous epithelium that shows hyperplasia, areas of papillary projections and dysplastic changes overlying connective tissue stroma. The epithelium shows invasion with islands, sheets and cords of atypical squamous cells extending deep into the underlying connective tissue stroma.
The squamous cells show atypical changes like cellular and nuclear pleomorphism, hyperchromatism, altered nuclear/cytoplasmic ratio, atypical mitosis, dyskeratotic cells, and keratin pearls. In addition, koilocytes with perinuclear clear spaces with small dark nuclei were seen. The supporting stroma consists of collagenous tissue interspersed with islands, sheets of atypical squamous epithelial cells, keratin pearls and epithelial pearls, blood vessels, extravasated red blood cells, and dense and diffuse inflammatory cell infiltrate suggestive of well-differentiated SCC of the gingiva. It is suggested that orthopantomogram and bone scintigraphy should be combined for early invasion. Magnetic resonance imaging (MRI) is more susceptible than computerized tomography (CT) for bony invasion. CT scanning provides extra data on the extent of participation, malignant infiltration, and cervical nodal disease. Ultrasound guided fine needle aspiration cytology has the greatest precision in the clinical diagnosis of cervical nodal metastasis relative to ultrasonography, CT scan, and MRI (1,12).
Positron emission tomography (PET)/CT does not play a part in the primary diagnosis of the regional extension of a confirmed oral cavity cancer. Previously undetected primary tumors or remote metastases may also be identified with PET-CT more accurately than with CT or MRI (13,14)
Nevertheless, it was found that fluorodeoxyglucose-PET is more accurate than CT and/or MRI, with 100% sensitivity and 61% to 71% specificity (14,15). Pre-operative ultrasound for tumor thickness is a reliable and cost-effective tool to measure the TT (tumor thickness) preoperatively, which will be of help in deciding the management. A TT of 4 mm and above is a predictor of occult cervical lymph node metastasis (16-18).
The therapy of pediatric oral SCC is a wide-ranging local resection while trying to prevent the important effect of radiotherapy on the pediatric population, including sequela, such as secondary malignancy (2,13). The treatment of gingival SCC is mainly surgical. Radical neck dissection, or its modification, is the standard treatment for the metastatic lymph nodes.
Partial maxillectomy using modified Weber-Ferguson approach was done. Supraomohyoid neck dissection was done to excise level IA (submental lymph node), IB (submandibular lymph node), II (upper deep jugular lymph node), III (middle deep jugular lymph node) lymph nodes and submitted for histopathological investigations.
Usually, radiation therapy is not the preferred therapy method for early gingivobuccal complex cancer. It is either used postoperatively or as a definitive therapy for advanced cancer with or without chemotherapy. Chemotherapy was used as a neoadjuvant, adjuvant or palliative therapy. The combination of cisplatin and 5-fluorouracil has been used as a standard induction therapy. Docetaxel has significant single-agent activity in SCC and has demonstrated improved survival and overall response (19). Given that some of the more serious lesions can imitate prevalent periodontal diseases, clinicians should be conscious that lesions that do not usually react to routine treatment should be biopsied (3,14).
Conflict of Interest Disclosures
The authors declared that they have no conflict of interests.
Acknowledgements
This study was supported by grants from K.D. Dental College and Hospital.
Ethical Statement
The protocol of the present study was approved by the Ethics Committee of the university.
Authors’ Contribution
Shishirmohan Devki,Venkatesh Hange worked during excisional biopsy. Venkatesh Hange worked on manuscript preparation, collection of relevant material, organizing case data & results.
References
- Misra S, Chaturvedi A, Misra NC. Management of gingivobuccal complex cancer. Ann R Coll Surg Engl 2008; 90(7):546-53. doi: 10.1308/003588408x301136 [Crossref] [ Google Scholar]
- Sidell D, Nabili V, Lai C, Cheung G, Kirsch C, Abemayor E. Pediatric squamous cell carcinoma: case report and literature review. Laryngoscope 2009; 119(8):1538-41. doi: 10.1002/lary.20531 [Crossref] [ Google Scholar]
- Cabral LA, de Carvalho LF, Salgado JA, Brandão AA, Almeida JD. Gingival squamous cell carcinoma: a case report. J Oral Maxillofac Res 2010; 1(3):e6. doi: 10.5037/jomr.2010.1306 [Crossref] [ Google Scholar]
- Morris LG, Ganly I. Outcomes of oral cavity squamous cell carcinoma in pediatric patients. Oral Oncol 2010; 46(4):292-6. doi: 10.1016/j.oraloncology.2010.01.015 [Crossref] [ Google Scholar]
- Modh A, Gayar OH, Elshaikh MA, Paulino AC, Siddiqui F. Pediatric head and neck squamous cell carcinoma: patient demographics, treatment trends and outcomes. Int J Pediatr Otorhinolaryngol 2018; 106:21-5. doi: 10.1016/j.ijporl.2017.12.032 [Crossref] [ Google Scholar]
- Wallace ML, Neville BW. Squamous cell carcinoma of the gingiva with an atypical appearance. J Periodontol 1996; 67(11):1245-8. doi: 10.1902/jop.1996.67.11.1245 [Crossref] [ Google Scholar]
- Binahmed A, Charles M, Campisi P, Forte V, Carmichael RP, Sándor GK. Primary squamous cell carcinoma of the maxillary alveolus in a 10-year-old girl. J Can Dent Assoc 2007; 73(8):715-8. [ Google Scholar]
- Stolk-Liefferink SA, Dumans AG, van der Meij EH, Knegt PP, van der Wal KG. Oral squamous cell carcinoma in children; review of an unusual entity. Int J Pediatr Otorhinolaryngol 2008; 72(1):127-31. doi: 10.1016/j.ijporl.2007.09.006 [Crossref] [ Google Scholar]
- Amichetti M. Squamous cell carcinoma of the oral tongue in patients less than fifteen years of age Report of a case and review of the literature. J Craniomaxillofac Surg 1989; 17(2):75-7. doi: 10.1016/s1010-5182(89)80049-6 [Crossref] [ Google Scholar]
- Bhanu Prasad V, Mallick S, Upadhyay AD, Rath GK. Systematic review and individual patient data analysis of pediatric head and neck squamous cell carcinoma: An analysis of 217 cases. Int J Pediatr Otorhinolaryngol 2017; 92:75-81. doi: 10.1016/j.ijporl.2016.11.005 [Crossref] [ Google Scholar]
- Shafer WG, Hiñe MK, Levy BM. A Textbook of Oral Pathology. 4th ed. Philadelphia: WB Saunders; 1983. p. 124-6.
- Heller AN, Klein A, Barocas A. Squamous cell carcinoma of the gingiva presenting as an endoperiodontic lesion. J Periodontol 1991; 62(9):573-5. doi: 10.1902/jop.1991.62.9.573 [Crossref] [ Google Scholar]
- Craig RM Jr, Vickers VA, Correll RW. Erythroplastic lesion on the mandibular marginal gingiva. J Am Dent Assoc 1989; 119(4):543-4. doi: 10.1016/s0002-8177(89)94013-0 [Crossref] [ Google Scholar]
- Kirkham DB, Hoge HW, Sadeghi EM. Gingival squamous cell carcinoma appearing as a benign lesion: report of case. J Am Dent Assoc 1985; 111(5):767-9. doi: 10.14219/jada.archive.1985.0197 [Crossref] [ Google Scholar]
- Wolff KD, Follmann M, Nast A. The diagnosis and treatment of oral cavity cancer. Dtsch Arztebl Int 2012; 109(48):829-35. doi: 10.3238/arztebl.2012.0829 [Crossref] [ Google Scholar]
- Keshava A, Gugwad S, Baad R, Patel R. Gingival squamous cell carcinoma mimicking as a desquamative lesion. J Indian Soc Periodontol 2016; 20(1):75-8. doi: 10.4103/0972-124x.164765 [Crossref] [ Google Scholar]
- Lonneux M, Lawson G, Ide C, Bausart R, Remacle M, Pauwels S. Positron emission tomography with fluorodeoxyglucose for suspected head and neck tumor recurrence in the symptomatic patient. Laryngoscope 2000; 110(9):1493-7. doi: 10.1097/00005537-200009000-00016 [Crossref] [ Google Scholar]
- Nair AV, Meera M, Rajamma BM, Anirudh S, Nazer PK, Ramachandran PV. Preoperative ultrasonography for tumor thickness evaluation in guiding management in patients with early oral tongue squamous cell carcinoma. Indian J Radiol Imaging 2018; 28(2):140-5. doi: 10.4103/ijri.IJRI_151_17 [Crossref] [ Google Scholar]
- Posner MR, Lefebvre JL. Docetaxel induction therapy in locally advanced squamous cell carcinoma of the head and neck. Br J Cancer 2003; 88(1):11-7. doi: 10.1038/sj.bjc.6600685 [Crossref] [ Google Scholar]