Avicenna J Dent Res. 16(4):238-241.
doi: 10.34172/ajdr.1860
Case Report
Management of an Idiopathic Gingival Fibromatosis (Elephantiasis): A Case Report With a Two-Year Follow-up
Lina Zarifpour 1, *  , Ali Modaberi 2
, Ali Modaberi 2 
Author information:
1Periodontics Department, School of dentistry, Kermanshah University of Medical Sciences, Kermanshah, Iran
2Endodontics Department, School of Dentistry, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Abstract
Background: Generalized gingival enlargement can arise from various causes. It may be hereditary, as observed in hereditary gingival fibromatosis, which occurs in association with syndromic conditions or results from the side effects of certain systemic medications such as phenytoin, cyclosporin, and nifedipine. This report discusses the condition of a 13-year-old girl who exhibited severe gingival overgrowth affecting both maxillary and mandibular arches, leading to substantial coverage of nearly all her teeth. The differential diagnosis included drug-induced enlargement and idiopathic gingival fibromatosis.
Methods: A conventional flap surgery alongside osteoplasty was performed to address the excess gingival tissue. Due to the generalized nature of the enlargement, the surgery was conducted quadrant by quadrant.
Results: The postoperative recovery was smooth, and the patient showed significant improvements in appearance. Follow-up evaluations over two years post-surgery indicated that the gingival condition remained stable.
Conclusion: Idiopathic gingival fibromatosis, although rare, is marked by significant gingival overgrowth. Surgical resection enhances aesthetics and improves functionality. While the recurrence of the condition is common, it may be managed or delayed through careful monitoring and scheduled follow-up appointments.
Keywords: Gingival diseases, Osseous surgery, Periodontal diseases
Copyright and License Information
© 2024 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Zarifpour L, Modaberi A. Management of an idiopathic gingival fibromatosis (elephantiasis): a case report with a two-year follow-up. Avicenna J Dent Res. 2024; 16(4):238-241. doi: 10.34172/ajdr.1860
Background
Gingival fibromatosis, also referred to as gingival fibromatosis, diffuse fibroma (1), familial elephantiasis, hereditary gingival hyperplasia, and hypertrophic gingiva, is characterized by the progressive fibrous enlargement of the gingiva in both the upper and lower jaws (2).
The overgrowth of the gingiva can lead to delayed eruption of teeth, as well as aesthetic, functional, psychological, and masticatory complications within the oral cavity (3).
Factors contributing to gingival overgrowth include plaque buildup, which may result from poor oral hygiene, nutritional deficiencies, or systemic hormonal influences (4).
Additional causes of gingival hyperplasia can include leukemia, certain medications, and genetic factors (5). The most prevalent types of gingival overgrowth are often associated with systemic medications, including the anti-epileptic drug phenytoin, the immunosuppressant cyclosporin, and the calcium channel blocker nifedipine, which is used for hypertension management (6).
Gingival overgrowth can appear as a standalone condition or may occur alongside various syndromes such as Zimmermann-Laband syndrome, Ramon syndrome, Ruther syndrome, Cross syndrome, and Jones syndrome (7,8).
Typically, gingival overgrowth begins with the eruption of permanent teeth, although it can also develop during the emergence of primary teeth and is rarely observed at birth (9,10). Clinically, the affected gingiva usually presents a normal pink hue, with a firm fibrotic texture. (3,11).
Histologically, the condition is marked by densely packed bundles of the fibrous connective tissue, a high level of differentiation with newly formed fibroblasts, and a limited number of blood vessels (10,11) accompanied by a well-organized epithelium with elongated and thin papillae embedded in the fibrous connective tissue (12).
Case Presentation
In June 2019, a 13-year-old female patient was referred to the Periodontics Department at the School of Dentistry of Shahid Sadoughi University of Medical Sciences, primarily due to swollen gums, which caused difficulties in chewing and resulted in aesthetic concerns.
Extraoral examination revealed a convex facial profile, a prominent premaxilla, and potentially incompetent lips (Figures 1A and 1B).
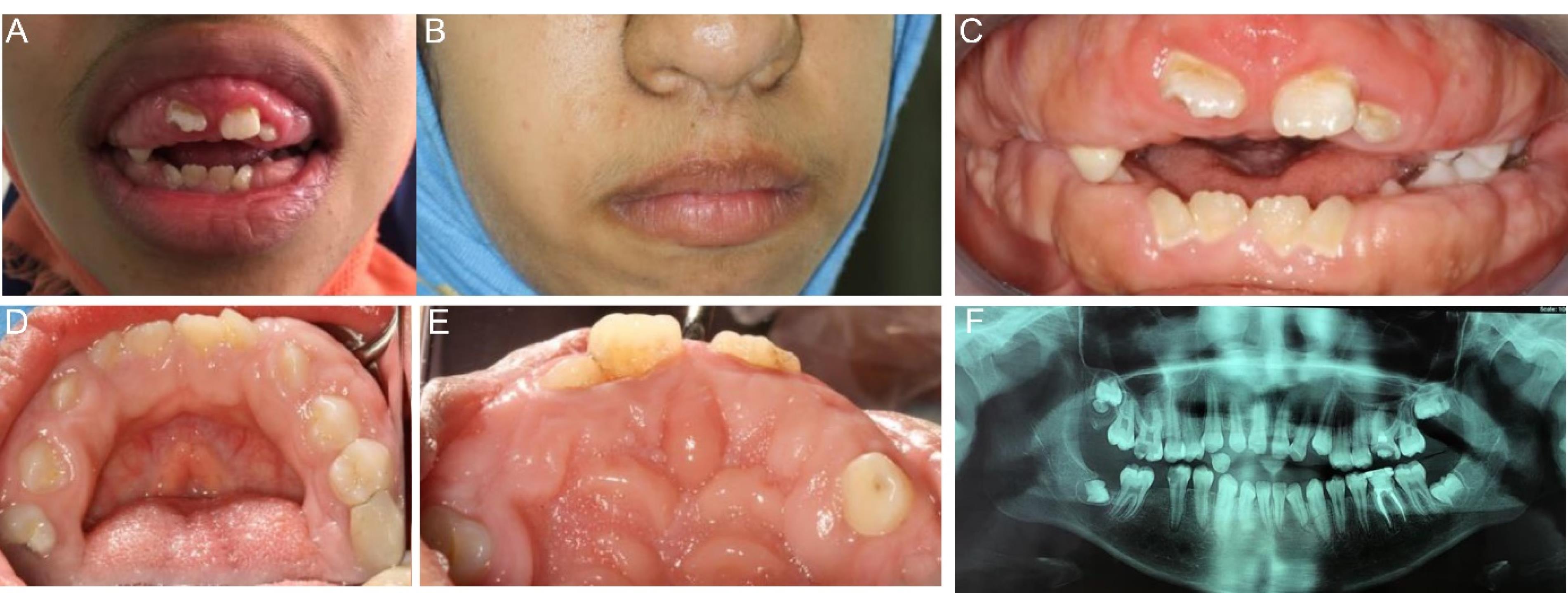
Figure 1.
(A-B) Extra-oral Examination: Profile View, (C) Intraoral Examination: Frontal View, (D) Palatal View, (E) Lingual View, and (F) Panoramic View
.
(A-B) Extra-oral Examination: Profile View, (C) Intraoral Examination: Frontal View, (D) Palatal View, (E) Lingual View, and (F) Panoramic View
Intraoral examination indicated a generalized fibrotic enlargement of the gingiva in both the upper and lower arches, with no reports of pain or bleeding. Numerous pseudo-pockets were detected, with probing depths exceeding 10 mm in certain areas (Figures 1C, 1D, and 1E).
The patient’s family history was unremarkable, with no paternal or maternal history of similar issues. A panoramic radiograph showed normal dental development, confirming the presence of all permanent teeth, which were at their appropriate developmental stages. Notably, a primary tooth crown was partially submerged in the upper right quadrant (Figure 1F).
Routine hematological tests, coagulation assessments, and thyroid hormone evaluations were all within normal limits. The patient had a history of gastric varices and underwent a hepatectomy four years ago, which precluded her from taking any medications, thereby ruling out the possibility of medication-related gingival overgrowth.
Following the initial diagnosis, an incisional biopsy was performed, and the specimen was examined under a light microscope. The analysis revealed a parakeratinized stratified squamous epithelium covering a connective tissue stroma. The connective tissue appeared densely collagenized and contained a mix of plump and spindle-shaped fibroblasts. A small number of chronic inflammatory cells, predominantly lymphocytes, were dispersed throughout the section, and areas with small- to medium-sized endothelial-lined blood vessels were also observed (Figure 2).
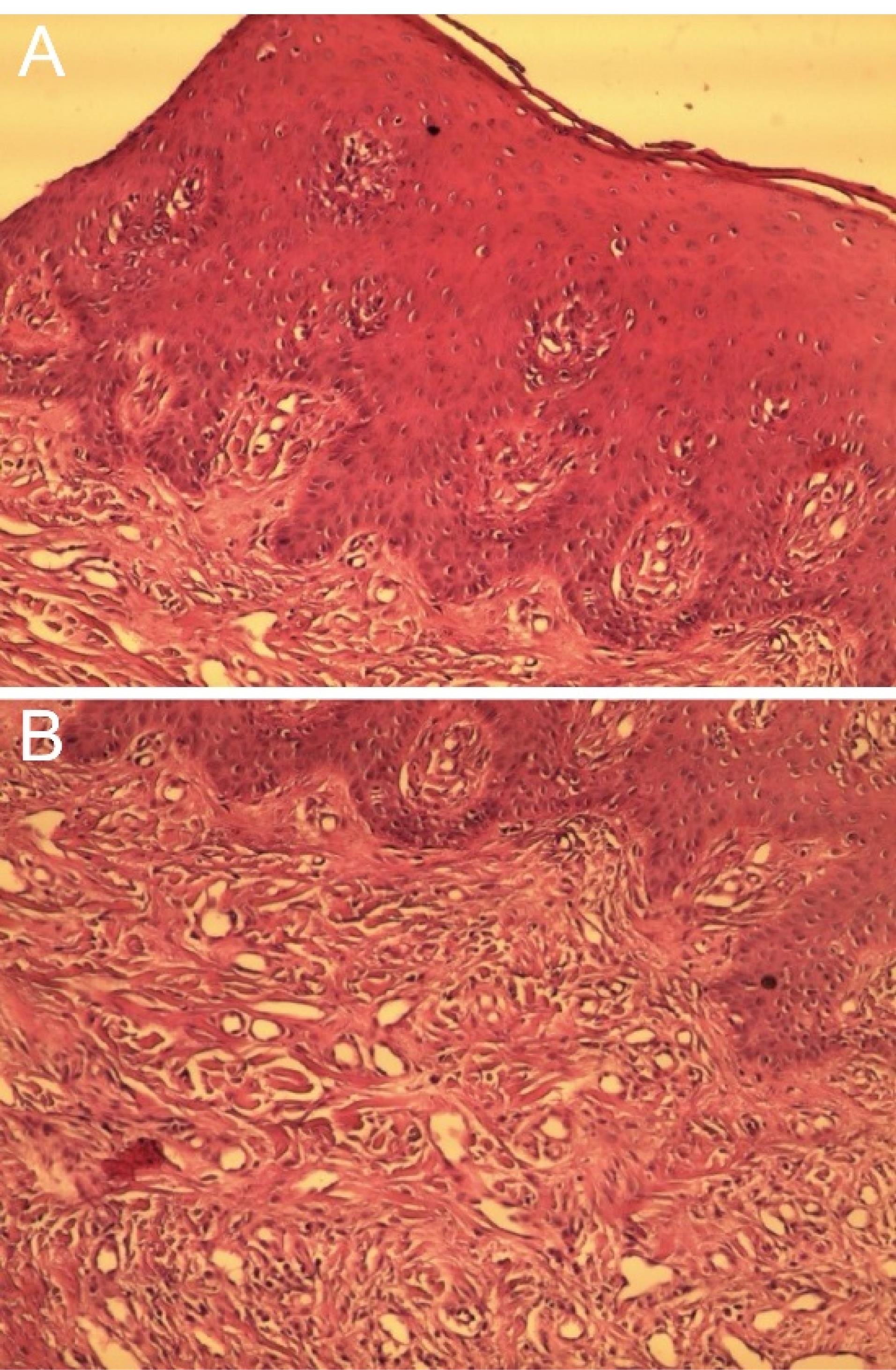
Figure 2.
(A-B) Microscopic Appearance
.
(A-B) Microscopic Appearance
Methods
Case Management
Considering the severity of the gingival enlargements classified as Class 3, a full mucoperiosteal flap surgery was performed on a quadrant-by-quadrant basis, accompanied by osteoplasty. A gap of 2-3 weeks between the treatment of each quadrant was planned to help the patient recover from the surgical interventions.
Postoperative analgesia included acetaminophen 325 mg tablets, taken every 6 hours for three days. Additionally, amoxicillin (250 mg capsules) was prescribed three times a day for seven days, based on the recommendations of her medical doctor.
The patient was instructed to use a 0.12% chlorhexidine mouthwash twice daily for one week and was advised to maintain a relatively soft diet following each surgery. As healing progressed, she could gradually return to her normal diet. Detailed oral hygiene instructions were provided in this regard.
Results
Postoperative healing was satisfactory, with complete resolution of the patient’s aesthetic and masticatory issues, resulting in adequate functional ability. The surgical excision of the enlarged gingival tissue led to significant improvements in gingival aesthetics. The patient was placed on a follow-up schedule with visits at 1, 3, and 6 months, then annually for two years (Figures 3A, 3B, and 3C). After two years of follow-up, oral examination confirmed good oral hygiene, minimal plaque accumulation, normal probing depths, and no signs of lesion recurrence (Figures 3D and 3E).
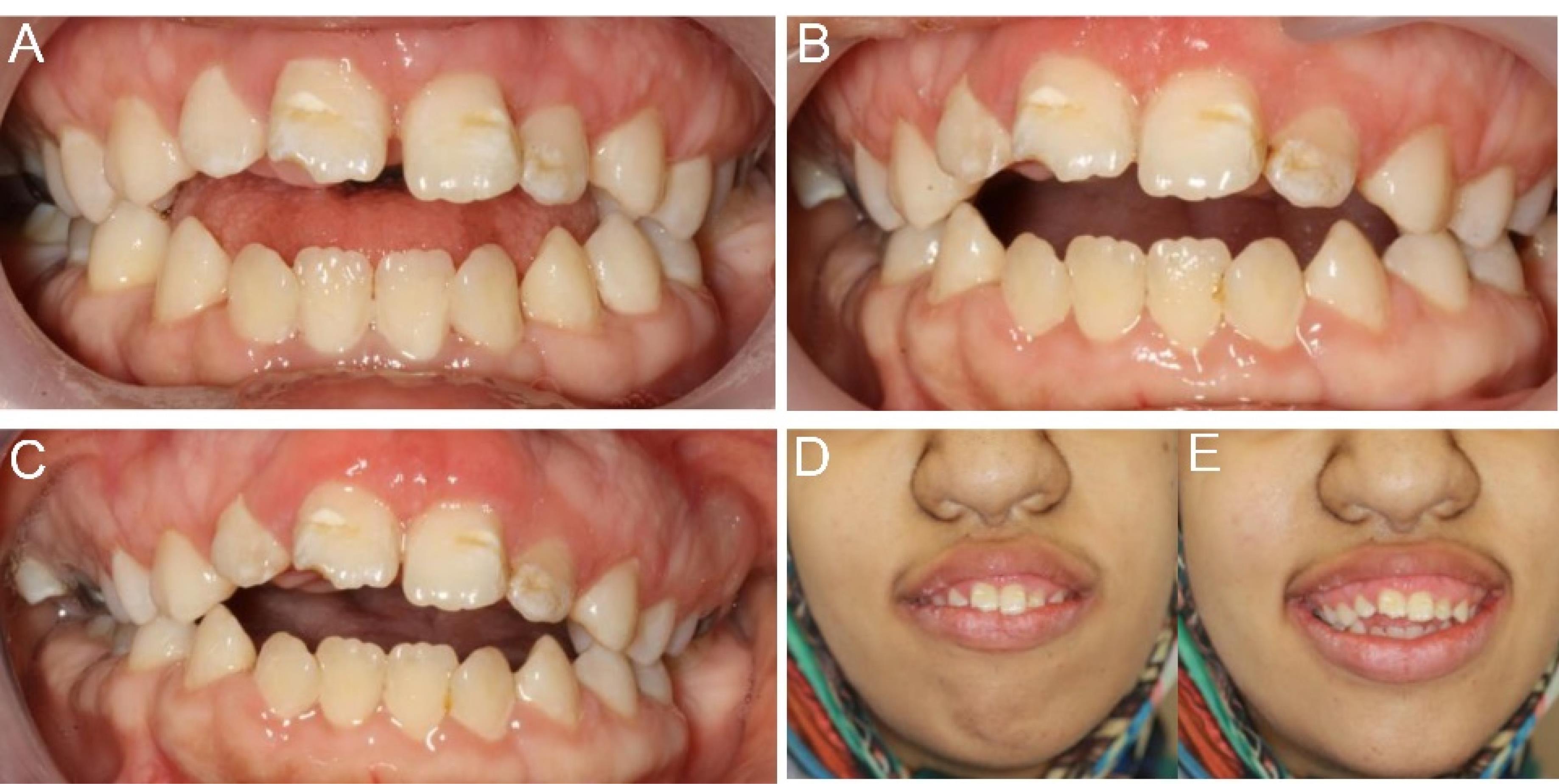
Figure 3.
(A) Three Months Postoperative Follow-up, (B) One Year Postoperative Follow-up, (C) Two Years Postoperative Follow-up, and (D-E) Extra Oral Photograph (Two Years Postoperative)
.
(A) Three Months Postoperative Follow-up, (B) One Year Postoperative Follow-up, (C) Two Years Postoperative Follow-up, and (D-E) Extra Oral Photograph (Two Years Postoperative)
Discussion
Gingival overgrowth is a significant pathological condition in periodontal medicine, and accurate diagnosis necessitates a thorough review of the patient’s medical history. The classification for the degree of gingival enlargement is as follows:
-
Grade 0: No signs of gingival enlargement
-
Grade I: Enlargement confined to the interdental papilla
-
Grade II: Enlargement involving both the papilla and marginal gingiva
-
Grade III: Enlargement covering three-fourths or more of the crown (13).
This report presents a case of severe gingival enlargement affecting both arches. Clinical and histological evaluations, along with systemic examinations, ruled out neoplastic enlargement.
Treatment requirements vary with the degree of severity; in cases of minimal enlargement, thorough scaling and proper home dental care may suffice to maintain oral health. However, a significant increase in gingival mass typically necessitates surgical intervention. Various techniques have been employed for the excision of enlarged gingival tissues, including external or internal bevel gingivectomy combined with gingivoplasty, apically positioned flaps, electrocautery, and CO2 laser treatments. Nonetheless, the conventional external bevel gingivectomy remains the most commonly used method for removing large amounts of tissue (14). Recurrence is a typical concern over varying timeframes; however, reports indicate that some cases have shown no recurrence over follow-up periods ranging from two to fourteen years (15).
This case highlights a rare instance of genuine gingival enlargement, with diagnosis primarily based on clinical, radiographic, and histopathological evaluations. While aesthetic and functional issues often necessitate surgical intervention, the potential for recurrence remains unpredictable. Nevertheless, the psychological benefits stemming from cosmetic improvements significantly outweigh the risks associated with recurrence (Figure 4).
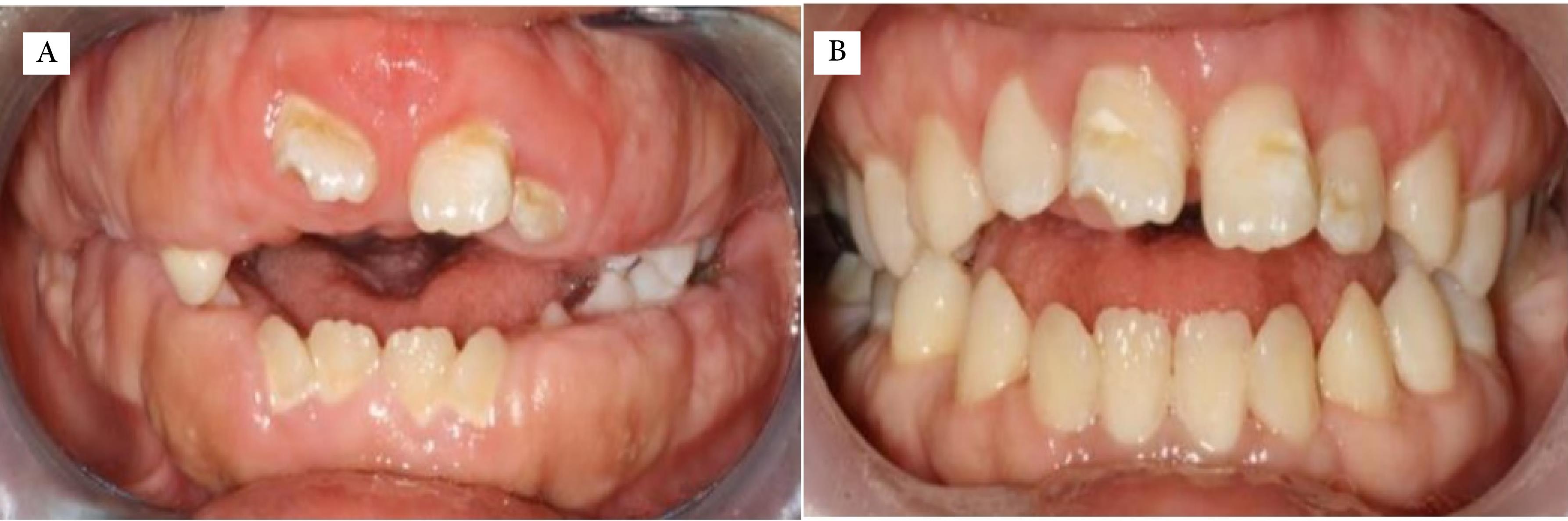
Figure 4.
(A) Pre-treatment view. (B) Post-treatment view after 2 years.
.
(A) Pre-treatment view. (B) Post-treatment view after 2 years.
Limitations
Considering the relapsing nature of this condition, it is advisable to implement longer follow-up periods.
Conclusion
This report documented a rare condition of gingival overgrowth. The diagnosis was established based on initial radiological and histological findings. Surgical treatments are frequently employed to address functional and aesthetic concerns, though recurrence remains uncertain. However, the psychological benefits of enhanced appearance surpass the associated risks of recurrence.
Authors’ Contribution
Conceptualization: Lina Zarifpour.
Data curation: Lina Zarifpour.
Formal analysis: Ali Modaberi.
Investigation: Lina Zarifpour.
Methodology: Lina Zarifpour.
Project administration: Lina Zarifpour.
Resources: Ali Modaberi.
Software: Lina Zarifpour.
Supervision: Ali Modaberi.
Validation: Ali Modaberi.
Visualization: Lina Zarifpour.
Writing–original draft: Lina Zarifpour.
Writing–review & editing: Ali Modaberi.
Competing Interests
There are no conflicts of interest.
Ethical Approval
After thoroughly explaining the treatment procedures, written consent was obtained from the patient’s mother, and verbal consent was secured from the patient. The study was conducted in accordance with the Declaration of Helsinki.
Funding
None.
References
- Jayachandran M, Kapoor S, Mahesh R. Idiopathic gingival fibromatosis rehabilitation: a case report with two-year followup. Case Rep Dent 2013; 2013:513153. doi: 10.1155/2013/513153 [Crossref] [ Google Scholar]
- Mahendra L, Govindarajan S, Jayanandan M, Shamsudeen SM, Kumar N, Madasamy R. Complete bilateral gemination of maxillary incisors with separate root canals. Case Rep Dent 2014; 2014:425343. doi: 10.1155/2014/425343 [Crossref] [ Google Scholar]
- Jaju PP, Desai A, Desai RS, Jaju SP. Idiopathic gingival fibromatosis: case report and its management. Int J Dent 2009; 2009:153603. doi: 10.1155/2009/153603 [Crossref] [ Google Scholar]
- Aboujaoude S, Aoun G. Hereditary gingival fibromatosis: a report of a severe case. Cureus 2022; 14(3):e23280. doi: 10.7759/cureus.23280 [Crossref] [ Google Scholar]
- Coletta RD, Graner E. Hereditary gingival fibromatosis: a systematic review. J Periodontol 2006; 77(5):753-64. doi: 10.1902/jop.2006.050379 [Crossref] [ Google Scholar]
- Dongari-Bagtzoglou A. Drug-associated gingival enlargement. J Periodontol 2004; 75(10):1424-31. doi: 10.1902/jop.2004.75.10.1424 [Crossref] [ Google Scholar]
- Almiñana-Pastor PJ, Buitrago-Vera PJ, Alpiste-Illueca FM, Catalá-Pizarro M. Hereditary gingival fibromatosis: characteristics and treatment approach. J Clin Exp Dent 2017; 9(4):e599-602. doi: 10.4317/jced.53644 [Crossref] [ Google Scholar]
- Nitta H, Kameyama Y, Ishikawa I. Unusual gingival enlargement with rapidly progressive periodontitis Report of a case. J Periodontol 1993; 64(10):1008-12. doi: 10.1902/jop.1993.64.10.1008 [Crossref] [ Google Scholar]
- Bozzo L, Machado MA, de Almeida OP, Lopes MA, Coletta RD. Hereditary gingival fibromatosis: report of three cases. J Clin Pediatr Dent 2000; 25(1):41-6. doi: 10.17796/jcpd.25.1.e254616x22403280 [Crossref] [ Google Scholar]
- Ramer M, Marrone J, Stahl B, Burakoff R. Hereditary gingival fibromatosis: identification, treatment, control. J Am Dent Assoc 1996; 127(4):493-5. doi: 10.14219/jada.archive.1996.0242 [Crossref] [ Google Scholar]
- Baptista IP. Hereditary gingival fibromatosis: a case report. J Clin Periodontol 2002; 29(9):871-4. doi: 10.1034/j.1600-051x.2002.290913.x [Crossref] [ Google Scholar]
- Tripathi AK, Dete G, Saimbi CS, Kumar V. Management of hereditary gingival fibromatosis: a 2 years follow-up case report. J Indian Soc Periodontol 2015; 19(3):342-4. doi: 10.4103/0972-124x.148643 [Crossref] [ Google Scholar]
- Coletta RD, Almeida OP, Graner E, Page RC, Bozzo L. Differential proliferation of fibroblasts cultured from hereditary gingival fibromatosis and normal gingiva. J Periodontal Res 1998; 33(8):469-75. doi: 10.1111/j.1600-0765.1998.tb02346.x [Crossref] [ Google Scholar]
- Cunha JL, da Cruz Ramos MA, Regis DM, Sanchéz-Romero C, de Andrade ME, Bezerra BT. Generalized hereditary gingival fibromatosis in a child: clinical, histopathological and therapeutic aspects. Autops Case Rep 2020; 10(1):e2020140. doi: 10.4322/acr.2020.140 [Crossref] [ Google Scholar]
- Miller MC. Lasers in dentistry: an overview. CDS Rev 1992; 85(4):26-8. [ Google Scholar]