Avicenna J Dent Res. 16(3):184-188.
doi: 10.34172/ajdr.1803
Brief Report
Orthodontic-Orthognathic Management of a Patient With Severe Mandibular Deficiency Due to Bicondylar Fracture: A Case Report
Nasrin Farhadian 1  , Amirfarhang Miresmaeili 1, Behrooz Khodabandehloo 1, *
, Amirfarhang Miresmaeili 1, Behrooz Khodabandehloo 1, *  , Omid Soltani–nia 2, Faryad Fatehi 2
, Omid Soltani–nia 2, Faryad Fatehi 2
Author information:
1Department of Orthodontics, Faculty of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran
2Department of Oral & Maxillofacial Surgery, School of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran
Abstract
This case report is about a 30-year-old Iranian female. The patient’s chief complaint was the backwardness of the lower jaw. The patient reported a history of condylar fractures in childhood. There was crowding in the maxillary and mandibular arch, and the midline in the mandible was 2 mm deviated to the left. The canine and first premolar on the left side of the maxilla were extracted, and the canine on the left side of the mandible was impacted. Clinical examinations and paraclinical documents revealed that the patient was a skeletal class II case with mandibular deficiency, complicated by a vertical maxillary excess. Virtual surgery planning was used to plan the patient’s treatment. The amount of adhesion of soft tissue to hard tissue was also taken into consideration. According to the measurements of the patient and the class II, vertical maxillary excess of the patient, the shortness of the ramus, and the large angle of the occlusal plane, our chosen orthognathic surgery included bilateral sagittal split osteotomy, advancement genioplasty, and maxillary impaction.
Keywords: Orthognathic surgery, Mandibular advancement, Mandibular condyle
Copyright and License Information
© 2024 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Farhadian N, Miresmaeili A, Khodabandehloo B, Soltani–nia O, Fatehi F. Orthodontic-orthognathic management of a patient with severe mandibular deficiency due to bicondylar fracture: a case report. Avicenna J Dent Res. 2024; 16(3):184-188. doi:10.34172/ajdr.1803
Background
Condylar fracture in early childhood is relatively common, and about 75% of children with this fracture have normal growth, but condylar fracture possibly affects occlusion and mandible movement and leads to the maldevelopment of the mandible and even temporomandibular joint ankylosis (1). A gummy smile, which may be a chief complaint in some patients, can be of skeletal, dentoalveolar, dentogingival, or neuromuscular origin, or a combination of these (2). Severe dental crowding, which can be caused by a combination of hereditary and environmental factors, is one of the main reasons for referrals for orthodontic treatment. A three-dimensional (3D) evaluation of all aspects of malformation is necessary to achieve the best treatment result. Virtual surgical planning (VSP) allows the 3D replication of the surgical procedures to more accurately show the estimated outcome to the clinician and the patient (3,4). This manuscript presents orthodontic-orthognathic management of a case with severe skeletal class II, followed by a bicondylar fracture and a gummy smile, revealing complications due to pre-extraction and impacted teeth.
Case Presentation
Diagnosis and Etiology
A 30-year-old female referred to the Department of Orthodontics at the Hamadan University of Medical Sciences. Her chief complaint was the back of her lower jaw and the crowding of her teeth. A history of bilateral condylar fracture followed by the condylectomy of both sides at age 10 was reported, and clinical evaluation showed a severe skeletal class II with a mandibular deficiency, short ramus, severe gingival display on smiling, a high facial angle, and incompetent lips. The patient’s face was symmetric in the frontal dimension. In addition, the midline of the maxillary teeth related to the face was coinside, and the midline of the mandibular teeth was 2 mm off to the right side related to the chin. The maximum mouth opening was 30 mm. There was no click in the temporomandibular joint region. Intra-oral examination revealed that overbite was decreaed, overjet was increased, maxilla was constricted, space deficiency was seen in both arch, the canine and the first premolar in the left side of maxilla were previously exracted and the canine in the left side of mandible was impacted. Radiographic findings demonstrated the backward rotation of the mandible, bidentoalveolar protrusion, significant chin deficiency, and lower right canine impaction (Figure 1). Table 1 presents the skeletal and dental angles, as well as the amount of overbite and overjet at pre-treatment. The etiology of skeletal problems was generally related to bilateral condylectomy, and the cause of dental crowding was attributed to tooth size/arch size discrepancies.

Figure 1.
Initial Photos and Graphs
.
Initial Photos and Graphs
Table 1.
Pre-treatment Skeletal and Dental Angle, Overbite, Overjet, and Space Deficiency
|
Parameters
|
Measurement
|
| Spaced deficiency upper arch |
5 mm |
| Spaced deficiency lower arch |
9 mm |
| SNA |
81° |
| SNB |
64° |
| ANB |
17° |
| SN-GOGN |
56° |
| FMIA |
28° |
| U1-SN |
108° |
| Overbite |
1 mm |
| Overjet |
12 mm |
Treatment Objectives
-
Decreasing gumminess and improving profile appearance and chin deficiency by mandibular advancement, maxillary impaction, and genioplasty advancement
-
Helping to relieve maxillary constriction and crowding through wire expansion and tooth extraction
-
Helping to relieve mandibular crowding and incisor protrusion by tooth extraction
Treatment Alternative
The severity of mandibular deficiency was in favor of distraction osteogenesis (DO) in the mandible. DO is a useful and well-established technique for bone and soft tissue formation in moderate-to-severe bone deficiency cases. It demonstrates good results with long-term stability, is more comfortable for the patients, and permits greater retention periods, which contribute to long-term stability (5). Due to the lack of access to the device and its cost, orthognathic surgery (maxillary impaction and mandibular advancement with genioplasty) was planned for the patient.
Treatment Progress
After the extraction of the upper and lower right first premolars and the impacted lower left canine, the presurgical orthodontic treatment was started using Standard Edge Wise 0.018-inch system brackets bonded to the upper arch, followed by the lower arch. The first and second molars were banded. Initial aligning and levelling were begun using 0.012-inch NiTi wire and sequentially progressed to 0.018-inch stain less steel (SS), considering wire expansion to improve the upper arch form. Next, space closing and midline correction were performed using 0.016 × 0.022-inch SS with closing loops. The space for replacing the upper left canine remained accordingly. A coordinated upper and lower 0.016 × 0.022 SS wire was placed before surgery. Presurgical prediction and planning for inverted L or bilateral sagittal split osteotomy were evaluated on cone-beam computed tomography and a face scan of the patient (Figure 2).

Figure 2.
Virtual Surgical Planning
.
Virtual Surgical Planning
For the advancement of the mandible, inverted ‘L’ surgery was considered, and the VSP was designed accordingly. The inverted ‘L’ osteotomy is frequently applied to class II skeletal deformities that possess a short vertical ramus height and concomitant high mandibular plane angle. The skeletal correction often requires significant counterclockwise movement to improve the projection of the lower facial third. These osteotomy and subsequent fixation are typically performed through a submandibular (Risdon) skin incision and require the preparation of the graft (6); however, the patient did not accept this operation due to the need for a separate surgery for graft preparation. Therefore, the bilateral sagittal split osteotomy surgery was performed for the patient according to VSP, with the surgyguide digitally constructed and printed. Maxilla was repositioned superiorly by 3 mm and set back by 2 mm. Subsequently, the mandible was advanced by 8 mm. Then, genioplasty advancement was considered by 5 mm.
Treatment Results
Two months after the surgery, the patient was visited for post-surgical orthodontics. The patient was debonded after achieving a normal occlusion five months after the surgery. Post-treatment records showed a successfully well-balanced and harmonious facial profile and occlusion. Intraorally, the gumminess was corrected after the Lefort I surgical procedure, while the extraoral profile and aesthetics were improved. The patient was also referred for an upper left canine tooth implant (Figure 3).

Figure 3.
Final Photos and Graphs
.
Final Photos and Graphs
Post-treatment cephalometric findings revealed that the soft tissue convexity significantly decreased, while skeletally, the SNB improved from 64 to 72, and the ANB angle decreased from 17 to 5 (Table 2). The superimposition of before- and after-treatment lateral cephalometry was performed (Figure 4).
Table 2.
Post-treatment Skeletal and Dental Angles, Overbite, and Overjet
|
Parameters
|
Measurement
|
| SNA |
77° |
| SNB |
72° |
| ANB |
5° |
| SN-GOGN |
42° |
| FMIA |
40° |
| U1-SN |
100° |
| Overbite |
2 mm |
| Overjet |
2 mm |
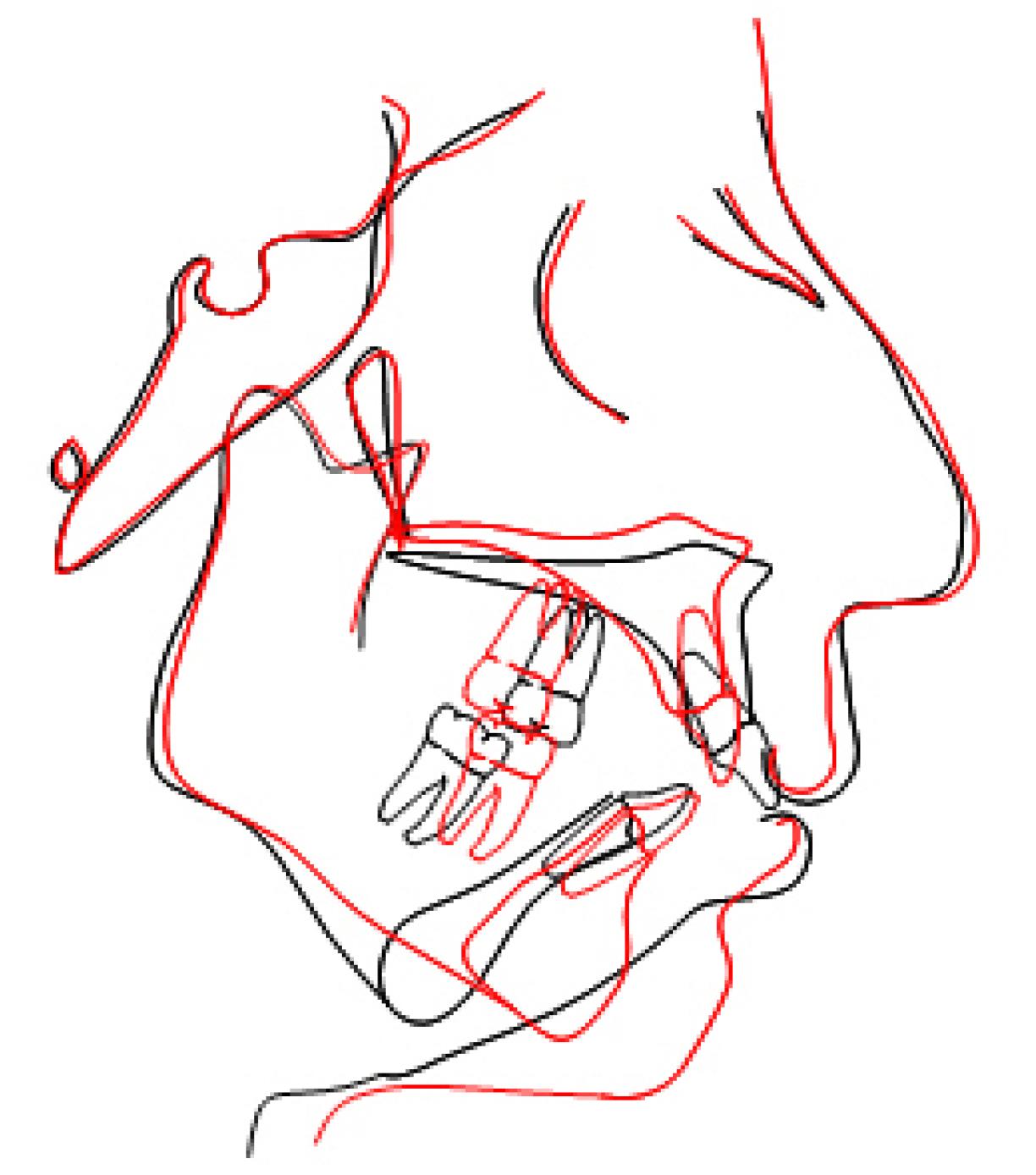
Figure 4.
Super Imposition of Initial and Final Lateral Cephalometric Radiographs
.
Super Imposition of Initial and Final Lateral Cephalometric Radiographs
The treatment successfully addressed the patient’s chief complaint (both aesthetic and functional needs).
For the maxilla, a Hawley retainer was considered, along with the pontic of the left canine tooth, and a fixed orthodontic retainer from canine to canine was considered in the mandible. The patient was visited at intervals of 3, 6, and 12 months later. Dental occlusion and facial aesthetics were in stable condition, and the patient was satisfied with the treatment results.
Discussion
This particular case study sheds light on the various aspects of treatment planning and management. Class II malocclusions with severe mandibular deficiency and high angle are most commonly treated with a combination of maxillary and mandibular osteotomies (7). In many instances, orthognathic surgery aims to correct occlusal discrepancies; but, more importantly, it is performed for the patient to correct facial imbalances and significantly enhance the facial profile (8). Due to the complexity of this patient’s treatment, close communication between the orthodontic and surgical teams was needed at different stages. In this case, VSP was used to predict the results. VSP allows the surgeon and orthodontist to accurately visualize the hard and soft tissue changes that would occur with the surgery. However, despite hard tissue predictions being accurate, soft tissue changes remain an unpredictable factor in the outcome of treatment (9,10). There are many individual variations in the soft response to surgery, and the causes of these variations can include changes in the thickness of the soft tissue, muscle tone, and where the muscles connect to the underlying skeletal structures. If the soft tissue is thinner and the muscle tone is higher, the adherence of the soft tissue to the underlying hard tissue will be greater. In addition, this adherence is greater near the muscle connection to the underlying skeleton. The amount of soft tissue cut, the position of the osteotomy cut, and the fixation method are also among the things that affect the soft tissue response (11). Because of these variations in soft tissue response, it is important to talk with the patient before treatment to achieve realistic expectations and consider side surgeries if necessary. Anyway, according to the studies, on average, soft tissue adherence to hard tissue changes in VSP was taken into consideration (9,10,12).
Maxillary impaction causes widening of the alar base, raising the tip of the nose, and thinning and shortening of the lips. In the case of maxillary impaction, it should be kept in mind that if the amount is more than needed, it will make the patient appear older.
The mentalis muscle plays an important role in raising the lower lip. This muscle is cut in genioplasty, so the display of lower incisors may increase after genioplasty (11).
Patients with a severe mandibular deficiency may have difficulty keeping the airway open during the surgery. Therefore, during surgery, experienced clinicians should perform this task correctly.
Facial swelling after surgery may last up to 6 months. Thus, the final response of the soft tissue should be evaluated after this period, and ideally, the required adjunctive surgeries should be performed after this period.
Conclusion
Complete data collection using 3D imaging and scanning tools to evaluate and predict treatment results can lead to acceptable facial balance and function in complex orthognathic cases.
Acknowledgments
The authors would like to thank the Department of Radiology, Surgery, and Orthodontics of the Faculty of Dentistry of Hamadan University of Medical Sciences.
Authors’ Contribution
Conceptualization: Nasrin Farhadian and Amirfarhang Miresmaeili.
Data curation: Behrooz Khodabandehloo.
Investigation: Behrooz khodabandehloo and Faryad Fatehi.
Methodology: Nasrin Farhadian and Omid Soltani-Nia.
Project administration: Behrooz Khodabandehloo.
Resources: Behrooz Khodabandehloo.
Supervision: Nasrin Farhadian.
Validation: Nasrin Farhadian and Behrooz Khodabandehloo.
Visualization: Nasrin Farhadian.
Writing–original draft: Nasrin Farhadian and Behrooz Khodabandehloo.
Writing–review and editing: Behrooz Khodabandehloo.
Competing Interests
The authors declare that they have no competing interests.
Ethical Approval
This study was confirmed by the Ethics Committee of Hamadan Dental School (Ethical Code: IR.UMSHA.REC.1402.645).
Funding
This study received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Li MX, Xing X, Li ZB, Li Z. Classification and treatment strategies for condylar fractures in children. Br J Oral Maxillofac Surg 2021; 59(7):776-82. doi: 10.1016/j.bjoms.2020.09.016 [Crossref] [ Google Scholar]
- Ser Yun JB, Luo M, Yin Y, Zhi Hui VL, Fang B, Han XL. Etiology-based treatment strategy for excessive gingival display: literature review. World J Surg Surg Res 2019; 2:1103. [ Google Scholar]
- van Twisk PH, Tenhagen M, Gül A, Wolvius E, Koudstaal M. How accurate is the soft tissue prediction of Dolphin Imaging for orthognathic surgery?. Int Orthod 2019; 17(3):488-96. doi: 10.1016/j.ortho.2019.06.008 [Crossref] [ Google Scholar]
- Wong WW, Davis DG, Camp MC, Gupta SC. Contribution of lip proportions to facial aesthetics in different ethnicities: a three-dimensional analysis. J Plast Reconstr Aesthet Surg 2010; 63(12):2032-9. doi: 10.1016/j.bjps.2009.12.015 [Crossref] [ Google Scholar]
- Rachmiel A, Shilo D. The use of distraction osteogenesis in oral and maxillofacial surgery. Ann Maxillofac Surg 2015; 5(2):146-7. doi: 10.4103/2231-0746.175777 [Crossref] [ Google Scholar]
- Franco PB, Farrell BB. Inverted L osteotomy: a new approach via intraoral access through the advances of virtual surgical planning and custom fixation. Oral Maxillofac Surg Cases 2016; 2(1):1-9. doi: 10.1016/j.omsc.2016.01.001 [Crossref] [ Google Scholar]
- Chu YM, Bergeron L, Chen YR. Bimaxillary protrusion: an overview of the surgical-orthodontic treatment. Semin Plast Surg 2009; 23(1):32-9. doi: 10.1055/s-0028-1110099 [Crossref] [ Google Scholar]
- Oueis R, Waite PD, Wang J, Kau CH. Orthodontic-orthognathic management of a patient with skeletal class II with bimaxillary protrusion, complicated by vertical maxillary excess: a multi-faceted case report of difficult treatment management issues. Int Orthod 2020; 18(1):178-90. doi: 10.1016/j.ortho.2019.09.002 [Crossref] [ Google Scholar]
- Lo LJ, Weng JL, Ho CT, Lin HH. Three-dimensional region-based study on the relationship between soft and hard tissue changes after orthognathic surgery in patients with prognathism. PLoS One 2018; 13(8):e0200589. doi: 10.1371/journal.pone.0200589 [Crossref] [ Google Scholar]
- Fabré M, Mossaz C, Christou P, Kiliaridis S. Professionals’ and laypersons’ appreciation of various options for Class III surgical correction. Eur J Orthod 2010; 32(4):395-402. doi: 10.1093/ejo/cjp104 [Crossref] [ Google Scholar]
- Naini FB, Gill DS. Orthognathic Surgery: Principles, Planning and Practice. John Wiley & Sons; 2017.
- Ajmera DH, Singh P, Leung YY, Gu M. Three-dimensional evaluation of soft-tissue response to osseous movement after orthognathic surgery in patients with facial asymmetry: a systematic review. J Craniomaxillofac Surg 2021; 49(9):763-74. doi: 10.1016/j.jcms.2021.04.010 [Crossref] [ Google Scholar]