Avicenna J Dent Res. 16(1):35-41.
doi: 10.34172/ajdr.1778
Original Article
Evaluating the Effects of Diode Laser 940 nm Adjunctive to Conventional Scaling and Root Planning for Gingival Sulcus Disinfection in Chronic Periodontitis Patients
Banafsheh Poormoradi 1  , Nazli Rabinezhad 2
, Nazli Rabinezhad 2  , Leila Mohamadpour 3
, Leila Mohamadpour 3  , Maryam Kazemi 4, *
, Maryam Kazemi 4, *  , Maryam Farhadian 5
, Maryam Farhadian 5 
Author information:
1Department of Periodontology, Dental Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
2Department of Periodontology, Dental School, Hamadan University of Medical Sciences, Hamadan, Iran
3Department of Pedodontology, School of Dentistry, Shahid Beheshti University of Medical Sciences, Tehran, Iran
4Department of Periodontology, Dental School, Hamadan University of Medical Sciences, Hamadan, Iran
5Department of Biostatistics, Hamadan University of Medical Sciences, Hamadan, Iran
Abstract
Background: Chronic periodontitis (CP) can lead to the loss of tooth-supporting structures. Scaling and root planning (SRP) is the standard treatment, but lasers may provide additional benefits. This study evaluated a 940 nm diode laser as an adjunct to SRP for CP treatment.
Methods: In this split-mouth, randomized clinical trial, 32 CP patients with at least two teeth with a pocket depth of more than 4 mm were treated with regular treatment of SRP plus health education with or without the intervention group. Further, a 940 nm diode laser was applied for the decontamination of the gingival groove. Probing pocket depth, clinical attachment loss (CAL), gingival index (GI), bleeding on probing (BOP), and plaque index (PI) were evaluated at baseline, 4 weeks, and 8 weeks after scaling. The data were analyzed by SPSS software (version 21), where descriptive methods and statistical tests such as the analysis of variance test were used with repeated measurements, and P<0.05 was accepted as statistically significant.
Results: All parameters improved significantly in both groups (P<0.05), except for GI, which decreased significantly more with a laser versus SRP alone (P<0.05). The results revealed no other statistically significant between-group differences.
Conclusion: The adjunctive diode laser provided limited additional improvements compared to SRP alone over 8 weeks. The significant GI reduction indicated that a diode laser may provide some benefits for enhancing non-surgical periodontal treatment. Larger trials are needed to determine if this extra improvement is clinically meaningful in the long term.
Clinical Relevance: Diode laser adjuncts to SRP demonstrated minimal short-term benefits over SRP alone in CP patients. The role of lasers in periodontal therapy requires further study.
Trial Registration: IRCT20120215009014N234 (retrospectively registered).
Keywords: Chronic periodontitis, Low-level laser therapy, Non-surgical periodontal treatment, Diode laser, Scaling and root planning
Copyright and License Information
© 2024 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Poormoradi B, Rabinezhad N, Mohamadpour L, Kazemi M, Farhadian M. Evaluating the effects of diode laser 940 nm adjunctive to conventional scaling and root planning for gingival sulcus disinfection in chronic periodontitis patients. Avicenna J Dent Res. 2024; 16(1):35-41. doi:10.34172/ajdr.1778
Background
Periodontal disease has been a major challenge for oral health and quality of life for decades(1). Periodontitis, a multifactorial disease affecting tooth-supporting tissues, is influenced by several predisposing factors, including genetic, environmental, and systemic factors(2). These factors can alter the expression of the disease and the patient’s susceptibility to its development. Oral microbial biofilms, also known as dental plaques, commonly provoke an inflammatory response, resulting in gingival inflammation. Without effective treatment, this inflammation may progress and lead to the destruction of supporting periodontal structures in susceptible hosts (3).
Due to the close link between bacteria and plaque, along with chronic periodontitis (CP), eliminating bacterial deposits is undoubtedly the primary goal of periodontal therapy (4). Scaling and root planning (SRP) is the most commonly performed procedure for the treatment of CP (5,6). SRP involves the mechanical eradication of supra- and subgingival plaque/calculus from the tooth and root surfaces using manual, sonic, and/or ultrasonic instruments (7). Its advantage lies in its safety and universal applicability in the vast majority of cases. However, there are still some limitations in terms of non-surgical mechanical treatment. In areas with difficult access, such as deep or winding periodontal pockets, furcation sites, root curvature, and poorly contoured restorations, SRP alone is prone to incomplete elimination of periodontal pathogens. The residual subgingival calculus and bacterial deposits remaining on the root surface result in unsatisfactory treatment effects. Considering the deficiency, various techniques have been recommended as adjunctive approaches, such as laser radiation (4).
The most common laser applications for periodontal therapy include a diode, carbon dioxide (CO2), neodymium-doped: yttrium aluminium garnet (Nd:YAG), erbium-doped: yttrium aluminium garnet (Er:YAG) and erbium, chromium-doped: yttrium, scandium, gallium, and garnet (Er,Cr:YSGG) lasers with wavelengths ranging from 635 to 10 600 nm. All these wavelengths can be used adjunctively to mechanical non-surgical instrumentation to debride connective tissue and epithelium within periodontal pockets, inactivate bacteria, and ablate subgingival calculus (8). The diode laser is a solid-state semiconductor laser that typically uses a combination of gallium, arsenide, and other elements such as aluminum and indium to alter electrical energy into light energy. Considering that the diode basically does not interact with dental hard tissues, the laser is an excellent soft tissue surgical laser suggested for cutting and coagulation of gingiva plus oral mucosa, as well as for soft tissue curettage or sulcular debridement. The diode lasers are currently used for pocket curettage by clinicians because of their flexible fiber delivery system, which is suitable for pocket insertion (9).
Periodontal therapy is closely associated with new technological developments and tends to constantly improve. Modern therapy for periodontitis includes classic treatment methods, improved periodontal surgery techniques, and the use of laser technology.Diode lasers in the wavelength range of 655–980 nm can accelerate wound healing, increase angiogenesis and the release of growth factors, and prevent damage to the root surface. The 940 nm wavelength falls within this range. The most common wavelengths considered in nonsurgical and surgical periodontal therapy are 800–980 nm. In addition, 940 nm is included in this commonly used range (10). Given the lack of studies that observe the results of the effect of a 940 nm diode laser in patients with CP, this study aimed to investigate the effect of a 940 nm diode laser supplemented with the conventional treatment of SRP for gingival sulcus disinfection in patients with CP.
Materials and Methods
Thirty-two subjects (7 men and 25 women, with a mean age ± standard deviation of 38.24 ± 10,67 years) were selected from the population referring to the Periodontology Department of Hamadan University of Medical Sciences, Hamadan, Iran, between 2017 and 2018. Subjects who fulfilled the inclusion criteria were invited to participate in the study (IR.UMSHA.REC.1397.044). All eligible subjects signed an informed consent form. The study was designed according to the CONSORT 2010 guidelines (Figure 1). The study protocol was evaluated and approved by the Human Research Ethics Committee of the institution (IRCT20120215009014n234).
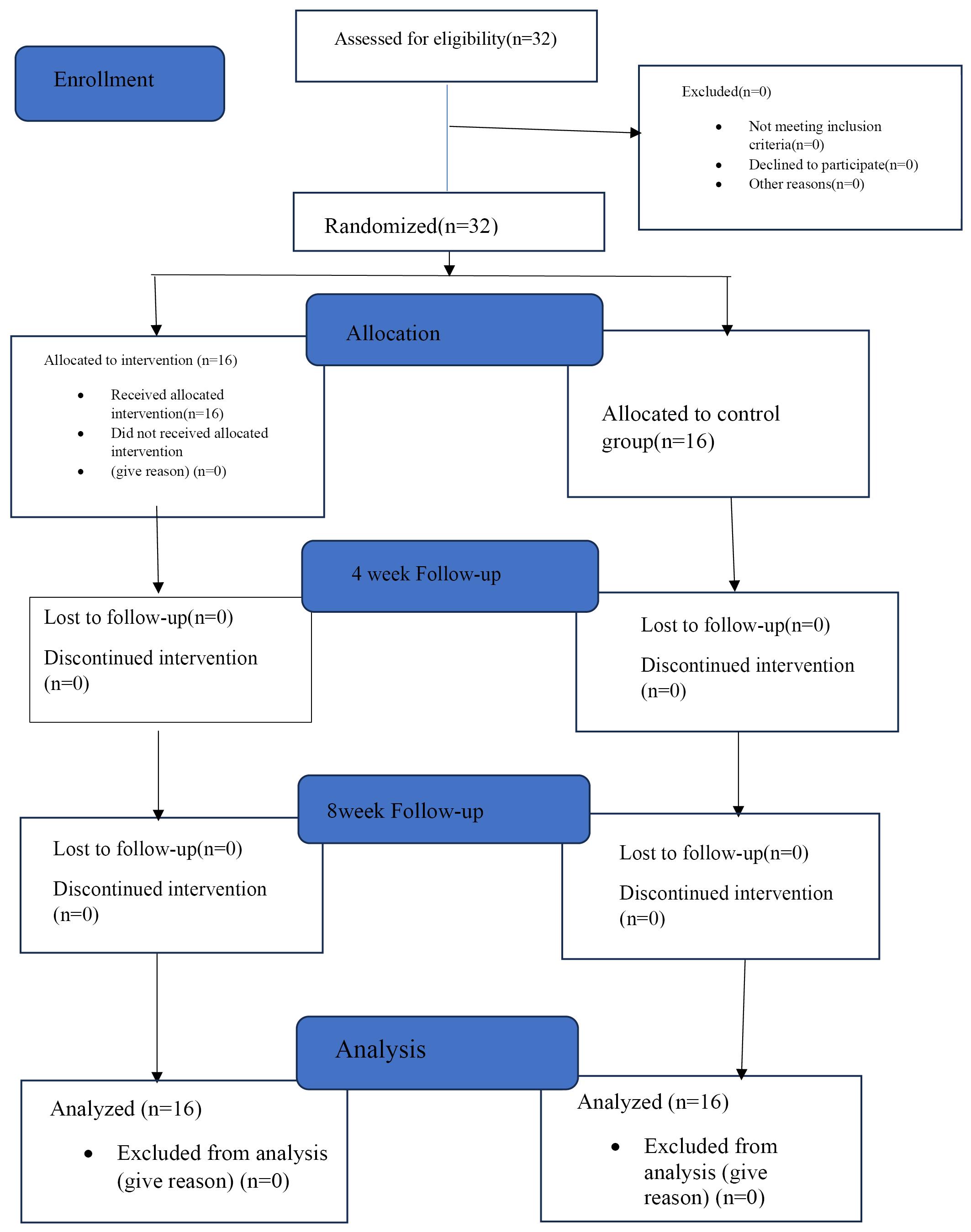
Figure 1.
Study Design According to the CONSORT 2010 Guidelines. Note. CONSORT: Consolidated standards of reporting trials
.
Study Design According to the CONSORT 2010 Guidelines. Note. CONSORT: Consolidated standards of reporting trials
Inclusion and Exclusion Criteria
The inclusion criteria were age 18 years and above, lack of systemic health conditions, lack of taking any medications, presence of at least 15 teeth, visible plaques (30% or less), positive bleeding on probing (BOP), and at least 2 teeth with a pocket depth of more than 4 mm.
On the other hand, the exclusion criteria included alcohol consumption and smoking, pregnant or lactating women, use of antioxidants (vitamin C, A, D, or E), antibiotics, anti-inflammatory drugs, anti-septic mouthwash during the six months before the study, and any non-surgical periodontal treatment during the last one year before the study. The other exclusion criteria were the presence of any systemic diseases such as diabetes or cardiovascular disease, the usage of any medications that could impact periodontal status, and teeth with furcation involvement or mobility of any stage.
The studied parameters included probing pocket depth (PPD), clinical attachment loss (CAL), gingival index (GI), BOP, and plaque index (PI).
In each patient, the mouth was randomly divided into test and control parts. To ensure that the examiner is unaware of the placement of the patients in each group, someone as the research guide opened an envelope and entered the patient into a group, inputting the patient’s first and last name as well as the group in which the patient was placed in a form. He kept this form to himself. To ensure that the statistical analyst was unaware of the groups, in this form, each group was marked with a color, and only the research director and the therapist were aware of the color of each group. All laser-related treatments were performed by a periodontologist, and all measurements related to probing were conducted by a dental student under the supervision of another periodontologist. All patients were given the usual treatment of scaling and leveling the root surface by piezo (Woodpecker, Dte-d5, UK; Figure 2) and health education. Then, the patient’s health was checked every week, and professional prophylaxis was performed if necessary.
In the intervention group, in addition to the usual treatment, there was periodontal pocket debridement by a diode laser. In the intervention group, a laser (Biolase, Epic10, California, USA; Table 1) with a wavelength of 940 nm, an E3 type, and an optical fiber diameter of 300 microns was applied to the inner surface of the envelope in a non-initiated manner, and at an angle of 10 degrees to the inner surface of the envelope, 1 mm less than the depth of the probe was irradiated from top to bottom with a spiral movement from apical to coronal and in chopped mode and a duty cycle of 50% for 15 seconds (Figure 3). The laser used for cellular cleaning was Diode 940 1W, a pulsed laser with a pulse duration of 15 seconds and an off time of 50 seconds. The average power was 0.7W. Laser treatment was performed by placing the fiber inside the periodontal pocket, almost parallel to the tooth, and moving continuously from the mesial to the distal direction and then from the coronal to the apical end. In the treatment session, the laser was irradiated to reduce the contamination of the gingival groove before SRP. In addition, it was used for the decontamination of the gingival groove, and non-initiated bleeding was performed with a power of 0.8 watts and 10 seconds in each place.
Table 1.
Laser Parameters
|
Laser Parameters
|
|
| Type of laser |
940 nm nGaAsP semi-conductor diode |
| Laser company |
Biolase, San Clemente, CA, USA |
| Emission mode |
Chopped mode |
| Delivery system |
Optical fiber |
| Power |
0.7-0.8-1 W |
| Time on/time off |
10-15s on/50s off |

Figure 3.
Laser Radiation Inside the Periodontal Pocket
.
Laser Radiation Inside the Periodontal Pocket
Thus, the 940 nm diode laser was applied before, during, and after the conventional mechanical debridement (SRP) procedure in the test group (11).
A file containing the examination of clinical parameters (PPD, GI, BOP, CAL, and PI) was completed for all patients. PPD was measured by Williams probe from the gingival margin to the periodontal pocket floor BOP is the presence or absence of bleeding within 30 seconds after probing. It is classified by the Löe and Silness index (12) from 0 to 3, so that grades 0, 1, 2, and 3 represent no inflammation, mild, moderate, and severe inflammation, respectively. PI was measured with the O’Leary index (13). In this way, the patient is given a detector tablet, and PI is expressed as a percentage by dividing the number of stained surfaces by the total surfaces. Four and eight weeks after the treatment (6,14), the patients were called back to the faculty for follow-up and re-measurement of periodontal indicators.
Statistical Analysis
The data were collected according to the objectives of the study and analyzed using SPSS 21 software via descriptive statistics methods, and statistical tests such as the analysis of variance test were considered with repeated measurements. It is noteworthy that the significance level of 0.05 was taken into consideration in all the examined tests.
Results
This study investigated five periodontal parameters (PPD, CAL, GI, BOP, and PI) in 32 patients with CP. The patients were divided into a control group receiving SRP alone and a test group receiving SRP plus adjunctive 940 nm diode laser therapy. Clinical parameters were evaluated at baseline, 4 weeks, and 8 weeks post-treatment. In all cases, P < 0.05 was considered to be statistically significant.
Probing Pocket Depth
Intragroup comparisons revealed significant reductions in PPD over time in both the control (P< 0.001) and test (P< 0.001) groups. However, intergroup comparisons showed no significant differences in PPD reduction between the two groups at any time point (Table 2, Figure 4A).
Table 2.
Clinical Periodontal Parameters at Baseline, Four Weeks, and Eight Weeks Post-treatment (Mean ± SD)
|
Variable
|
Experimental Groups
|
Intragroup Comparison of Two Groups
Over Time (RM-ANOVA)
|
Between-Group Comparisons
(T-test)
|
|
Time/Group
|
Control
|
Test
|
P
Value
|
P
Value
|
| PPD |
Baseline |
3.09 ± 065 |
3.16 ± 0.67 |
|
0.253 |
| 4 weeks |
2.40 ± 0.73 |
2.12 ± 0.64 |
|
0.002 |
| 8 weeks |
2.21 ± 0.82 |
1.92 ± 0.65 |
|
0.001 |
| Intragroup comparison: P value |
< 0.001 |
< 0.001 |
< 0.326 |
|
| CAL |
Baseline |
2.32 ± 0.15 |
2.29 ± 0.15 |
|
0.698 |
| 4 weeks |
1.89 ± 0.11 |
1.74 ± 0.11 |
|
0.018 |
| 8 weeks |
1.74 ± 0.11 |
1.61 ± 0.11 |
|
0.009 |
| Intragroup comparison: P value |
< 0.001 |
< 0.001 |
< 0.552 |
|
| GI |
Baseline |
0.43 ± 0.22 |
0.57 ± 0.27 |
|
< 0.001 |
| 4 weeks |
0.30 ± 0.19 |
0.29 ± 0.14 |
|
0.818 |
| 8 weeks |
0.26 ± 0.15 |
0.17 ± 0.07 |
|
< 0.001 |
| Intragroup comparison: P value |
< 0.001 |
< 0.001 |
< 0.001 |
|
| BOP |
Baseline |
0.27 ± 0.15 |
0.32 ± 0.15 |
|
0.015 |
| 4 weeks |
0.16 ± 0.14 |
0.11 ± 0.09 |
|
0.003 |
| 8 weeks |
0.12 ± 0.13 |
0.06 ± 0.07 |
|
0.003 |
| Intragroup comparison: P value |
< 0.001 |
< 0.001 |
< 0.001 |
|
| PI |
Baseline |
0.45 ± 0.16 |
0.48 ± 0.11 |
|
0.252 |
| 4 weeks |
0.26 ± 0.08 |
0.29 ± 0.09 |
|
0.070 |
| 8 weeks |
0.22 ± 0.07 |
0.26 ± 0.10 |
|
0.002 |
| Intragroup comparison: P value |
< 0.001 |
< 0.001 |
< 0.116 |
|
Note. PPD: Probing pocket depth; CAL: Clinical attachment loss; GI: Gingival index; BOP: Bleeding on probing; PI: Plaque index. SD: Standard deviation; RM-ANOVA: Repeated measures analysis of variance.
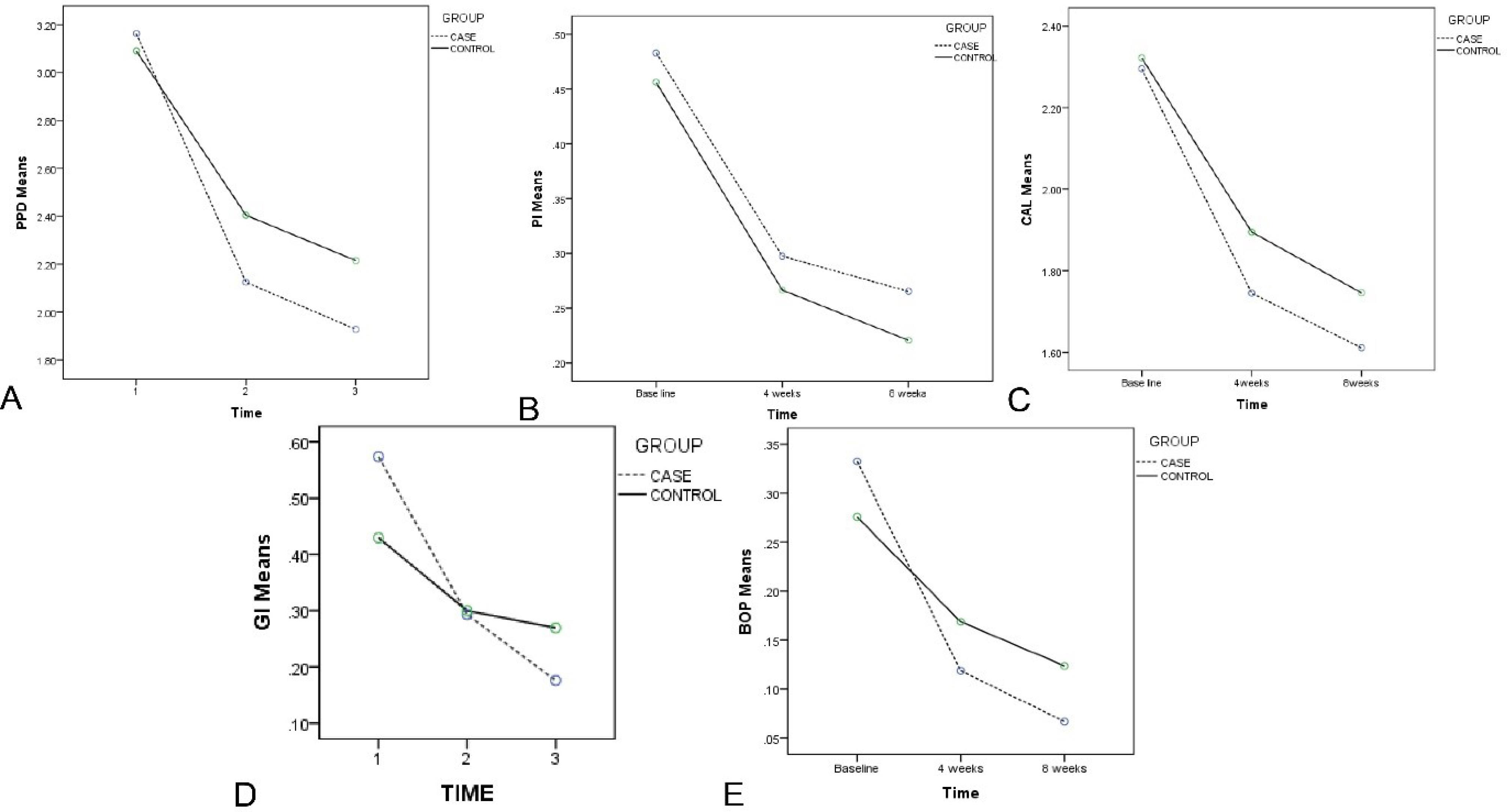
Figure 4.
The Trend of Changes in Indices in the Test and Control Groups: (A) PPD, (B) PI, (C) CAL, (D) GI, and (E) BOP. Note. PPD: Probing depth; PI: Plaque index; CAL: Clinical attachment; GI: Gingival index; BOP: Bleeding on probing
.
The Trend of Changes in Indices in the Test and Control Groups: (A) PPD, (B) PI, (C) CAL, (D) GI, and (E) BOP. Note. PPD: Probing depth; PI: Plaque index; CAL: Clinical attachment; GI: Gingival index; BOP: Bleeding on probing
Clinical Attachment Loss
Both groups demonstrated significant improvements in CAL over time (P< 0.001). Intergroup comparisons represented greater CAL gain in the test group compared to the control group 4 (P= 0.018) and 8 (P= 0.009) weeks post-treatment (Table 2, Figure 4C).
Gingival Index
GI scores decreased significantly over time in both groups (P< 0.001). Intergroup comparisons indicated significantly lower GI scores in the test group in comparison to the control group at baseline (P< 0.001) and 8 weeks (P< 0.001) but not at 4 weeks (P= 0.818), the details of which are shown in Table 2 and Figure 4D.
Bleeding on Probing
BOP percentages decreased significantly over time in both groups (P< 0.001). Intergroup comparisons showed no significant differences in BOP reduction between the two groups at any time point (Table 2, Figure 4E).
Plaque Index
Both groups exhibited significant reductions in PI scores over time (P< 0.001). Intergroup comparisons revealed no significant differences in PI reduction between the two groups at baseline (P= 0.252)or 4 weeks (P= 0.070), but significantly lower PI scores were observed in the control group at 8 weeks (P= 0.002), the results of which are provided in Table 2 and Figure 4B.
In summary, both SRP alone and SRP plus 940 nm diode laser therapy led to significant improvements in all investigated periodontal parameters over 8 weeks. Adjunctive laser therapy resulted in significantly greater gains in CAL at 4 weeks and 8 weeks and lower GI scores at baseline and 8 weeks compared to SRP alone. No significant differences between groups were observed for PPD or BOP at any time point, while PI scores were lower in the control group at 8 weeks. These findings suggest that 940 nm diode laser therapy may provide some additional clinical benefits when used as an adjunct to SRP in the treatment of CP.
Discussion
This randomized, split-mouth clinical trial investigated the efficacy of adjunctive 940 nm diode laser therapy compared to SRP alone in the treatment of CP. The results demonstrated significant improvements in all evaluated periodontal parameters (PPD, CAL, GI, BOP, and PI) over 8 weeks in both treatment groups. However, the adjunctive use of diode laser therapy provided limited additional clinical benefits compared to SRP alone. The findings of this study are consistent with several previous investigations that have reported modest improvements in clinical outcomes with the use of diode lasers as an adjunct to non-surgical periodontal therapy (8,15,16). For instance, a recent systematic review by Salvi et al (8) has shown that adjunctive laser therapy resulted in slightly greater reductions in PPD and gains in CAL compared to mechanical debridement alone, but the differences were not statistically significant. Similarly, Gurpegui Abud et al (15) and Özdemir et al (16) observed no significant differences in clinical parameters between SRP plus laser therapy and SRP alone in split-mouth randomized clinical trials.On the other hand, some studies have reported more substantial benefits of adjunctive laser therapy in the treatment of CP (17,18). Birang et al (17) found significantly greater reductions in PPD and gains in CAL with the combination of SRP and diode laser therapy compared to SRP alone in a split-mouth trial. Likewise, Dukić et al (18) found significantly better clinical outcomes with the adjunctive use of diode lasers in a parallel-arm randomized clinical study. The discrepancies in findings among studies may be attributed to variations in laser parameters, treatment protocols, and patient characteristics.
The limited additional benefits of laser therapy observed in the present study could be explained by several factors. First, applied laser parameters (940 nm wavelength, 0.7-1 W power, pulsed mode, and 10–15-second exposure time) may not have been optimal for achieving maximum clinical efficacy. Second, the sample size of 32 patients may have been insufficient to detect small but potentially clinically meaningful differences between groups. Third, the relatively short follow-up period of 8 weeks may not have captured the full extent of the long-term effects of laser therapy on periodontal healing and stability. Despite the limited additional benefits, the adjunctive use of 940 nm diode laser therapy resulted in significantly greater gains in CAL at 4 weeks and 8 weeks and lower GI scores at baseline and 8 weeks compared to SRP alone. The findings revealed that laser therapy may have some potential to enhance periodontal attachment and reduce gingival inflammation beyond the effects of mechanical debridement. The biological mechanisms underlying these effects may involve the ability of laser light to promote tissue healing, reduce bacterial loads, and modulate inflammatory responses (4). To optimize the clinical outcomes of adjunctive laser therapy, future studies should investigate different laser parameters (e.g., wavelength, power, and exposure time) and treatment protocols (e.g., number and timing of laser applications). Additionally, larger randomized clinical trials with longer follow-up periods are needed to establish the long-term efficacy and safety of laser therapy as an adjunct to non-surgical periodontal treatment. Cost-effectiveness analyses should also be conducted to determine whether the additional benefits of laser therapy justify the increased costs and resources required for its implementation in clinical practice.
Conclusion
In general, the findings of this study revealed that adjunctive 940 nm diode laser therapy provided limited additional clinical benefits compared to SRP alone in the treatment of CP over 8 weeks.
While laser therapy resulted in significantly greater gains in CAL and reductions in GI scores at some time points, the overall magnitude of the additional improvements was modest. Further research is needed to identify the optimal laser parameters and treatment protocols that can maximize the clinical efficacy of adjunctive laser therapy in periodontal practice. Until more definitive evidence is available, the routine use of laser therapy as an adjunct to non-surgical periodontal treatment cannot be strongly recommended based on the findings of this study alone.
Author’s Contribution
Conceptualization: Banafsheh Poormoradi.
Data curation: Leila Mohamadpour.
Formal analysis: Maryam Farhadian.
Funding acquisition: Nazli Rabinezhad.
Investigation: Leila Mohamadpour.
Methodology: Banafsheh Poormoradi.
Project administration: Banafsheh Poormoradi.
Resources: Maryam Kazemi.
Software: Maryam Kazemi.
Supervision: Nazli Rabinezhad.
Validation: Nazli Rabinezhad.
Visualization: Maryam Kazemi.
Writing–original draft: Maryam Kazemi.
Writing–review & editing: Maryam Kazemi.
Competing Interests
The authors declare that they have no conflict of interests.
Ethical Approval
The study protocol was approved by the Ethics Committee of Hamadan University of Medical Sciences(No. IR. UMSHA. REC. 1397.044).
Funding
None.
References
- Ren C, McGrath C, Jin L, Zhang C, Yang Y. The effectiveness of low-level laser therapy as an adjunct to non-surgical periodontal treatment: a meta-analysis. J Periodontal Res 2017; 52(1):8-20. doi: 10.1111/jre.12361 [Crossref] [ Google Scholar]
- Cadore UB, Reis MB, Martins SH, Invernici MM, Novaes AB Jr, Taba M Jr. Multiple sessions of antimicrobial photodynamic therapy associated with surgical periodontal treatment in patients with chronic periodontitis. J Periodontol 2019; 90(4):339-49. doi: 10.1002/jper.18-0373 [Crossref] [ Google Scholar]
- Chambrone L, Ramos UD, Reynolds MA. Infrared lasers for the treatment of moderate to severe periodontitis: an American Academy of Periodontology best evidence review. J Periodontol 2018; 89(7):743-65. doi: 10.1902/jop.2017.160504 [Crossref] [ Google Scholar]
- Jiang Y, Feng J, Du J, Fu J, Liu Y, Guo L. Clinical and biochemical effect of laser as an adjunct to non-surgical treatment of chronic periodontitis. Oral Dis 2022; 28(4):1042-57. doi: 10.1111/odi.13847 [Crossref] [ Google Scholar]
- Drisko CL. Periodontal debridement: still the treatment of choice. J Evid Based Dent Pract 2014;14 Suppl:33-41.e1. 10.1016/j.jebdp.2014.02.007.
- Cobb CM. Clinical significance of non-surgical periodontal therapy: an evidence-based perspective of scaling and root planing. J Clin Periodontol 2002; 29(Suppl 2):22-32. doi: 10.1034/j.1600-051X.29.s2.4.x [Crossref] [ Google Scholar]
- Al-Hamoudi N, Abduljabbar T, Mirza S, Al-Sowygh ZH, Vohra F, Javed F. Non-surgical periodontal therapy reduces salivary adipocytokines in chronic periodontitis patients with and without obesity. J Investig Clin Dent 2018; 9(2):e12314. doi: 10.1111/jicd.12314 [Crossref] [ Google Scholar]
- Salvi GE, Stähli A, Schmidt JC, Ramseier CA, Sculean A, Walter C. Adjunctive laser or antimicrobial photodynamic therapy to non-surgical mechanical instrumentation in patients with untreated periodontitis: a systematic review and meta-analysis. J Clin Periodontol 2020; 47 Suppl 22:176-98. doi: 10.1111/jcpe.13236 [Crossref] [ Google Scholar]
- Aoki A, Sasaki KM, Watanabe H, Ishikawa I. Lasers in nonsurgical periodontal therapy. Periodontol 2000 2004; 36:59-97. doi: 10.1111/j.1600-0757.2004.03679.x [Crossref] [ Google Scholar]
- Seyed-Monir A, Seyed-Monir E, Mihandoust S. Evaluation of 940-nm diode laser effectiveness on pocket depth, clinical attachment level, and bleeding on probing in chronic periodontitis: a randomized clinical single-masked split-mouth study. Dent Res J (Isfahan) 2023; 20:113. [ Google Scholar]
- Slot DE, Jorritsma KH, Cobb CM, Van der Weijden FA. The effect of the thermal diode laser (wavelength 808-980 nm) in non-surgical periodontal therapy: a systematic review and meta-analysis. J Clin Periodontol 2014; 41(7):681-92. doi: 10.1111/jcpe.12233 [Crossref] [ Google Scholar]
- Löe H. The gingival index, the plaque index and the retention index systems. J Periodontol 1967;38(6):Suppl:610-6. 10.1902/jop.1967.38.6.610.
- O’Leary TJ, Drake RB, Naylor JE. The plaque control record. J Periodontol 1972; 43(1):38. doi: 10.1902/jop.1972.43.1.38 [Crossref] [ Google Scholar]
- Sgolastra F, Petrucci A, Ciarrocchi I, Masci C, Spadaro A. Adjunctive systemic antimicrobials in the treatment of chronic periodontitis: a systematic review and network meta-analysis. J Periodontal Res 2021; 56(2):236-48. doi: 10.1111/jre.12821 [Crossref] [ Google Scholar]
- Gurpegui Abud D, Shariff JA, Linden E, Kang PY. Erbium-doped: yttrium-aluminum-garnet (Er:YAG) versus scaling and root planing for the treatment of periodontal disease: a single-blinded split-mouth randomized clinical trial. J Periodontol 2022; 93(4):493-503. doi: 10.1002/jper.21-0133 [Crossref] [ Google Scholar]
- Özdemir H, Gündoğar H, Akpınar A. Photobiomodulation therapy by 820 nm diode laser on nonsurgical periodontal treatment of smoker and nonsmoker patients: a single-blind parallel randomized clinical trial. Photochem Photobiol 2021; 97(4):860-4. doi: 10.1111/php.13394 [Crossref] [ Google Scholar]
- Birang R, Shahaboui M, Kiani S, Shadmehr E, Naghsh N. Effect of nonsurgical periodontal treatment combined with diode laser or photodynamic therapy on chronic periodontitis: a randomized controlled split-mouth clinical trial. J Lasers Med Sci 2015; 6(3):112-9. doi: 10.15171/jlms.2015.04 [Crossref] [ Google Scholar]
- Dukić W, Bago I, Aurer A, Roguljić M. Clinical effectiveness of diode laser therapy as an adjunct to non-surgical periodontal treatment: a randomized clinical study. J Periodontol 2013; 84(8):1111-7. doi: 10.1902/jop.2012.110708 [Crossref] [ Google Scholar]