Avicenna J Dent Res. 16(1):42-45.
doi: 10.34172/ajdr.1763
Original Article
Clinicopathologic Evaluation and Management of Twenty Cases of Oral Mucoceles
Neeraj Kumar 1, *  , Richa Kumari 2
, Richa Kumari 2
Author information:
1Department of Pediatric Dentistry, Post Graduate Institute of Child Health, Noida, Uttar Pradesh
2Government Dental College, Rohtak, Haryana
Abstract
Background: Oral mucoceles are benign minor salivary gland lesions characterized by a single or multiple, soft, fluctuant nodule, ranging from normal oral mucosal color to deep blue depending upon the extent of the swelling in deeper layers. This study evaluated clinicopathological features, including the etiology and management of oral mucoceles.
Methods: Twenty cases of oral mucoceles were diagnosed, and parameters such as age, gender, etiology, site, clinical presentation, including size, any symptoms, and treatment mode underwent evaluation.
Results: In 20 cases, the lesions were found to be more common in males compared to females (16:4). The most common site was the lower lip, and the etiology of mucocele was lip biting, with 80% of cases normal in color and size ranging between 5 mm and 10 mm. The most common type based on histopathology evaluation was the extravasation type in almost all cases.
Conclusion: The non-neoplastic benign lesions of minor or major salivary glands pose a diagnostic challenge because of their close resemblance to other pathologies and iatrogenic responses. Thus, the clinical knowledge and pathogenesis of these lesions are necessary for the correct diagnosis and appropriate treatment.
Keywords: Mucocele, Extravasation, Surgical excision, Minor salivary glands, Benign lesions
Copyright and License Information
© 2024 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Kumar N, Kumari R. Clinicopathologic evaluation and management of twenty cases of oral mucoceles. Avicenna J Dent Res. 2024; 16(1):42-45. doi:10.34172/ajdr.1763
Background
Oral mucocele is a common benign lesion of the oral mucosa due to the accumulation of mucin from minor salivary glands. The etiology of mucocele is due to trauma or the obstruction of the ducts of minor salivary glands. Oral mucoceles are usually single, painless, soft, translucent, and asymptomatic with fluctuant swelling (1). The most common locations of oral mucoceles are the lower and upper lips, followed by the buccal mucosa, the floor of the mouth, the retromolar area, and the hard palate (2). The prevalence of oral mucocele was 0.11% in Sweden, 0.08% in Brazil, and 2.5 lesions per 1000 in the American population (3). Mucoceles are classified into two types (i.e., extravasation and retention). Extravasation mucocele is a more common type of oral mucocele due to mechanical trauma to the excretory duct and extravasation of the mucin into the connective tissue stroma. The extravasation type of mucocele is devoid of epithelial lining and is most commonly found on the lower lip, buccal mucosa, and retromolar area (4). The retention type of mucocele is less common and typically located on the upper lip, hard palate, floor of the mouth, and maxillary sinus (5,6). In the retention type, mucus is retained in the excretory ducts/acini due to the obstruction, which may be due to sialolith or stricture (7). The diagnosis of the mucocele is normally based on clinical signs and symptoms. In a few cases, it spontaneously resolves by itself, but in some cases, it requires surgical excision. Other treatment modalities, such as micro-marsupialization, cryosurgery, intra-lesional steroids, and CO2 lasers, have been used in the literature (6). The aim of this study was to evaluate diagnosed cases of mucoceles in terms of their clinical and histological characteristics and treatment in order to assist health professionals in clinical practice.
Materials and Methods
A clinical cross-sectional study was conducted between September 2018 and September 2020 in the Outpatient Department of Dentistry, Government Medical College, Khandwa, Madhya Pradesh. The patients referred to the department with a chief complaint of asymptomatic swelling on the lower lip for 2‒5 months. Oral mucocele cases were diagnosed based on the clinical signs and symptoms. Written consent was obtained from each patient before surgical invention and participation. Detailed information related to age, gender, clinical appearance, location and size of the lesion, associated signs and symptoms, and treatment given for mucoceles was collected and recorded. A total of 20 patients (16 males and 4 females) aged 16‒60 years diagnosed with asymptomatic swelling on the lower lip were included in the study, which were managed by surgical excision. The excised lesions were sent for histopathological examinations in a few cases to confirm the diagnosis of oral mucocele. These variables were analyzed, and the frequency distribution was evaluated in all cases.
Results
A total of 20 cases of oral mucocele were involved from September 2018 to September 2020. The details of the 20 patients diagnosed with oral mucoceles are presented in Table 1. The age of the patients ranged from 16 to 60 years, out of whom 16 were males and 4 were females (Figures 1 and 2). The most common cause of oral mucocele was lip biting in 95% of cases, and the most common site was the lower lip in all study samples. In 80% of the cases, the mucosa had normal color and a size between 5 mm and 10 mm. All the cases presented with swelling and were asymptomatic only. Surgical excision was performed in few cases with no recurrence or any complication after a 6-month follow-up. A histopathological examination was performed, which showed hyperplastic parakeratinized stratified squamous epithelium, connective tissue fibrosis, and mucus-filled cells. The lesion also demonstrated small cystic spaces containing mucin, areas of spilled mucin surrounded by granulation tissue, and sebaceous cells in the connective tissue (Figure 3), which confirmed the extravasation type of oral mucocele.
Table 1.
Demographics and Distribution of the 20 Cases of Oral Mucoceles Evaluated in the Present Study
|
Demographic and Other Parameters
|
Frequency (N)
|
Percent
|
| Gender |
|
|
| Male |
16 |
80.0 |
| Female |
4 |
20.0 |
| Age group |
|
|
| 16-30 |
12 |
60.0 |
| 31-45 |
6 |
30.0 |
| 45-60 |
2 |
10.0 |
| Etiology |
|
|
| Lip sucking |
19 |
95.0 |
| Cheek biting |
0 |
0.0 |
| Malocclusion |
0 |
0.0 |
| Lip sucking and malocclusion |
1 |
5.0 |
| Color |
|
|
| Normal |
16 |
80.0 |
| Inflammatory red |
0 |
0.0 |
| Fibrous white |
4 |
20.0 |
| Size |
|
|
| 5-10 mm |
16 |
80.0 |
| 11-15 mm |
0 |
0.0 |
| > 15 mm |
4 |
20.0 |
| Site |
|
|
| Lower lip |
20 |
100.0 |
| Upper lip |
0 |
0.0 |
| Tongue |
0 |
0.0 |
| Hard palate |
0 |
0.0 |
| Floor of mouth |
0 |
0.0 |
| Associated symptoms |
|
|
| Asymptomatic swelling |
20 |
100.0 |
| Pain |
0 |
0 |
| Treatment |
|
|
| Surgical |
20 |
100.0 |
| Conservative |
0 |
0 |
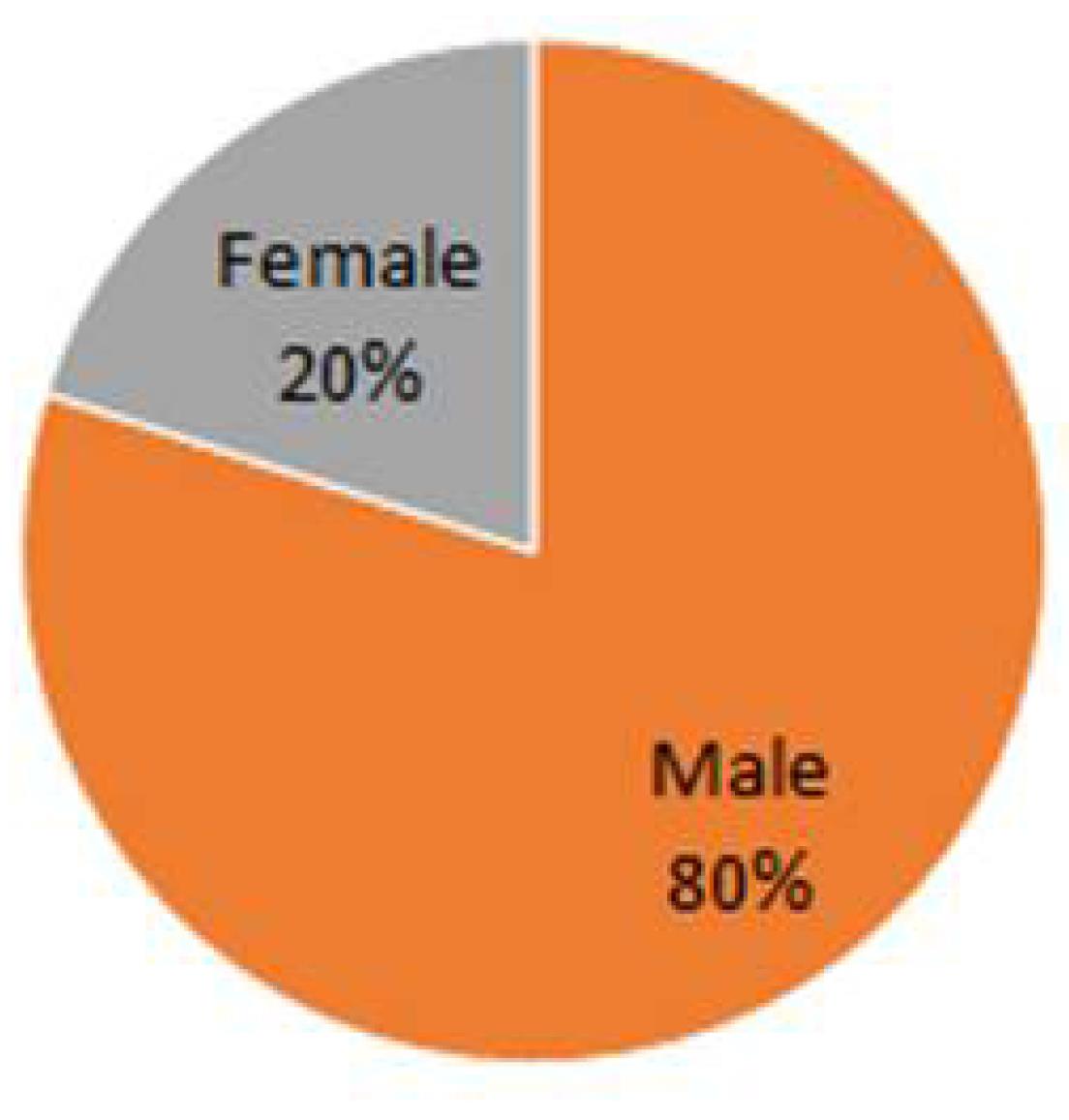
Figure 1.
Gender wise distribution of study sample in the present study
.
Gender wise distribution of study sample in the present study
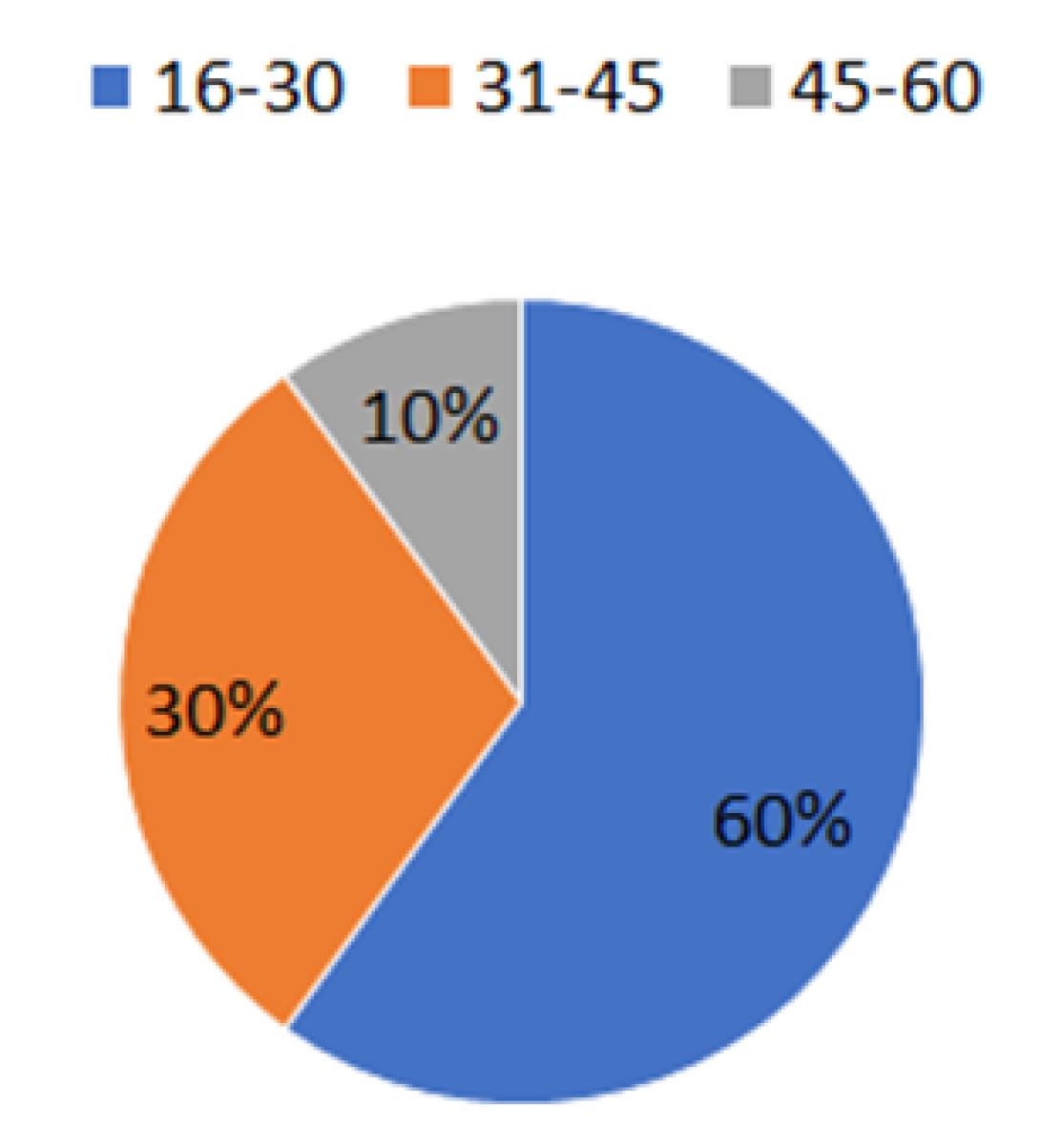
Figure 2.
Age-wise distribution of study sample in the present study
.
Age-wise distribution of study sample in the present study
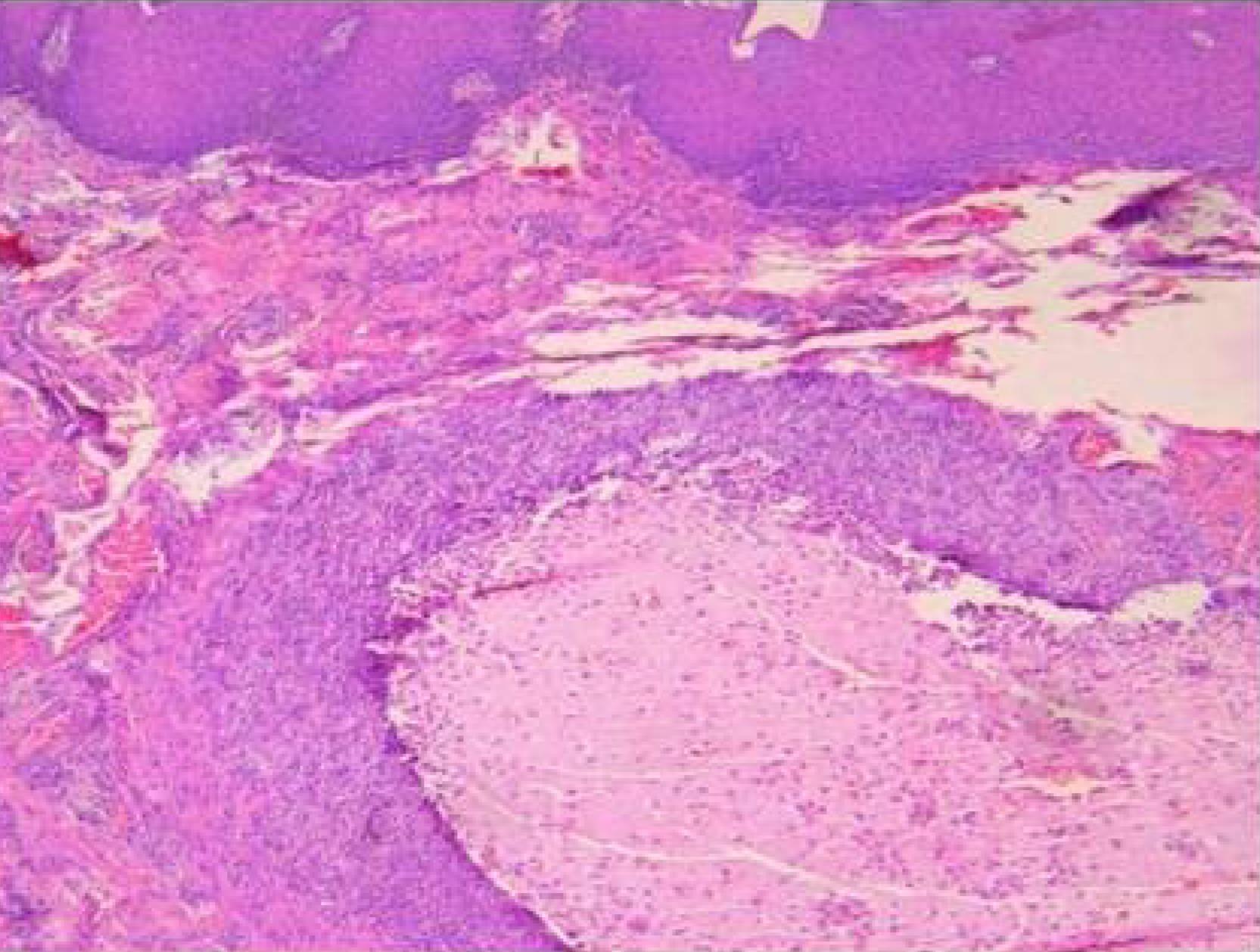
Figure 3.
Histopathological findings of extravasation type of oral mucocele showing hyperplastic parakeratinized stratified squamous epithelium, small cystic spaces containing mucin and mucus-filled cells, areas of spilled mucin surrounded by a granulation tissue and sebaceous cells in the connective tissue
.
Histopathological findings of extravasation type of oral mucocele showing hyperplastic parakeratinized stratified squamous epithelium, small cystic spaces containing mucin and mucus-filled cells, areas of spilled mucin surrounded by a granulation tissue and sebaceous cells in the connective tissue
Discussion
Oral mucocele is a clinical pathology in which mucus is accumulated in the connective tissue stroma due to trauma or obstruction in the excretory duct of minor salivary glands (5). It is a self-limiting mucous-containing pseudocyst of minor salivary glands commonly occurring in the oral cavity (3). The lesion may sometimes rupture, but the resorption and reaccumulation of the mucin occur and may cause the lesion to reform (6). Most mucoceles are devoid of the epithelial lining or covered by granulation tissue in some cases (4,6). Oral mucoceles can be single or multiple, usually rupturing and creating slight painful erosions that normally heal within a few days (8). It may take several days to weeks to occur, depending on the severity of the habits, such as lip sucking, malocclusion, and the like. The clinical presentation may be superficial or classical, depending on the depth of the lesion. In superficial mucoceles, lesions are located directly under the mucous membrane, and in classical mucoceles, they are located in the upper submucosa or deep within the connective tissue. (3)Spontaneous drainage may occur in superficial lesions, followed by recurrence in most cases. In long-standing cases, the surfaces of the mucocele may show fibrotic changes (9).Superficial lesions are bluish because of thin-walled overlying mucosa, while deeper lesions are well-circumscribed and usually covered by normal-appearing oral mucosa. Oral mucoceles are believed to occur in all ages, but children and teenagers are most commonly affected. (5) The incidence of mucocele most commonly happens in the second decade of life. Although oral mucoceles can occur in both genders, there is a male predominance, as reported by Nico et al (10),Yamasoba et al (11), and Oliveira et al (12). In this study, male predominance was also observed, which is in line with the results of other studies reported in the literature.
Oral mucoceles normally occur on mucosal surfaces that have minor salivary glands. The lower lip is the most commonly affected site; however, cases in the upper lip, palate, buccal mucosa, retromolar region, dorsal tongue, and lingual frenum have been rarely reported (8). In this study, most cases of oral mucoceles were also present on the lower lip.
The color of mucoceles ranged from a blue hue to the normal color of the oral mucosa, depending on the size and proximity to the mucosal surface and the elasticity of the mucosa (6). The blue hue results from vascular congestion and the translucency of the accumulated fluid beneath the stretched mucosa. (4,13), which conforms to the findings of this study, showing no interference with speech or swallowing; however, esthetic concerns were observed in a few cases. Trauma and obstruction of minor salivary gland ducts are considered crucial etiological factors. In the majority of our cases, lip biting was found to be the main etiological factor, which is in line with the findings of Bowers and Schaitkin (14), Lopez-Jornet and Bermejo-Fenoll (15), and Essaket et al (16). In the histopathology examination, there was acute inflammation with traces of mucus and fibrosis in the connective tissue. The lesion may demonstrate hyperplastic parakeratinized stratified squamous epithelium, small mucin-containing cystic spaces, spilled mucin surrounded by granulation tissue, and sebaceous cells in the connective tissue. The appearance of mucocele is pathognomonic, and the location, history of trauma, size, color, and consistency should be taken into consideration (17). Mucoceles are mobile lesions that are fluctuant with soft and elastic consistency, depending on the overlying tissue present over the lesion. A chronic mucocele with fibrosis would have less fluctuation, while a self-drained one would have no fluctuation (4). For chronic and larger-sized mucocele cases, the diagnosis may require routine radiographs, ultrasonography, or cone beam computed tomography for the determination of the origin, form, diameter, and position of the lesion. Oral mucocele shall be differentiated from lipoma, soft tissue abscess, oral lymphangioma, pyogenic granuloma, benign or malignant salivary gland neoplasms, irritational fibroma, oral lymphoepithelial cyst, oral hemangioma, gingival cyst of adults, cysticercosis, and the like. However, superficial mucoceles may sometimes be confused with cicatricial pemphigoid, lichen planus, or bullous lesions (8,9).
The various treatment modalities for mucoceles shall be marsupialization, complete surgical excision, cryosurgery, electrocautery, carbon dioxide lasers, and intra-lesional injection of sclerosing agents or steroids (6). However, recurrence may occasionally occur, and a second surgery is necessary CO2 lasers have been recently used for treating mucoceles as they provide a precise incision, a bloodless operating field, decreased post-operative swelling, edema, a minimized scar, and reduced postoperative pain (18). On the other hand, cryotherapy is an alternative, effective, non-surgical therapeutic, proposed method in which the application of an extreme cold temperature causes lesion destruction and the necrotic tissue is allowed to slough spontaneously. There are various advantages, such as a painless procedure, low chances of secondary infection, and hemorrhage (19). In this study, all the cases of oral mucocele were surgically excised using the scalpel blade method, and no recurrence or any other complication was reported after 6 months of follow-up.
Conclusion
Mucoceles are benign oral mucosal lesions usually diagnosed based on clinical findings and a definitive diagnosis based on the histopathological examination. The most common etiological factor is local trauma, followed by lip-biting, an abnormal oral habit that could be due to malocclusion or psychological stress. Although all cases were surgically treated without any complication, thorough clinical knowledge is essential to diagnose and treat these lesions due to their high recurrence rate. The study included only twenty patients within the specified duration; thus, more patients with oral mucoceles would be evaluated with long-term follow-ups.
Acknowledgements
The authors would like to thank all participants who gave their consent to participate in the study.
Authors’ Contribution
Conceptualization: Neeraj Kumar, Richa Kumari.
Data curation: Neeraj Kumar.
Formal analysis: Neeraj Kumar.
Investigation: Neeraj Kumar.
Methodology: Neeraj Kumar, Richa Kumari.
Project administration: Neeraj Kumar.
Resources: Neeraj Kumar.
Software: Neeraj Kumar.
Supervision:Neeraj Kumar, Richa Kumari.
Validation: Neeraj Kumar, Richa Kumari.
Visualization: Neeraj Kumar, Richa Kumari.
Writing–original draft:Neeraj Kumar, Richa Kumari.
Writing–review & editing: Neeraj Kumar, Richa Kumari.
Competing Interests
The authors have no conflict of interests.
Ethical Approval
Written consent was taken from each patient for recording and surgical excision.
Funding
Nil.
References
- Bagán Sebastián JV, Silvestre Donat FJ, Peñarrocha Diago M, Milián Masanet MA. [Clinico-pathological study of oral mucoceles]. Av Odontoestomatol 1990;6(7):389-91. [Spanish].
- Boneu-Bonet F, Vidal-Homs E, Maizcurrana-Tornil A, González-Lagunas J. Submaxillary gland mucocele: presentation of a case. Med Oral Patol Oral Cir Bucal 2005; 10(2):180-4. [ Google Scholar]
- Rashid AK, Anwar N, Azizah AM, Narayan KA. Cases of mucocele treated in the Dental Department of Penang Hospital. Arch Orofac Sci 2008; 3(1):7-10. [ Google Scholar]
- Ata-Ali J, Carrillo C, Bonet C, Balaguer J, Penarrocha M, Peñarrocha M. Oral mucocele: review of the literature. J Clin Exp Dent 2010; 2(1):e18-21. doi: 10.4317/jced.2.e18 [Crossref] [ Google Scholar]
- Daniels J, Mohammed I. Mucocele of lingual glands of Blandin and Nuhn: a report of 5 cases. Saudi Dent J 2005; 17(3):154-61. [ Google Scholar]
- Re Cecconi D, Achilli A, Tarozzi M, Lodi G, Demarosi F, Sardella A. Mucoceles of the oral cavity: a large case series (1994-2008) and a literature review. Med Oral Patol Oral Cir Bucal 2010; 15(4):e551-6. doi: 10.4317/medoral.15.e551 [Crossref] [ Google Scholar]
- de Camargo Moraes P, Bönecker M, Furuse C, Thomaz LA, Teixeira RG, de Araújo VC. Mucocele of the gland of Blandin-Nuhn: histological and clinical findings. Clin Oral Investig 2009; 13(3):351-3. doi: 10.1007/s00784-009-0252-x [Crossref] [ Google Scholar]
- Gupta B, Anegundi R, Sudha P, Gupta M. Mucocele: two case reports. J Oral Health Community Dent 2007; 1(3):56-8. doi: 10.5005/johcd-1-3-56 [Crossref] [ Google Scholar]
- Hayashida AM, Zerbinatti DC, Balducci I, Cabral LA, Almeida JD. Mucus extravasation and retention phenomena: a 24-year study. BMC Oral Health 2010; 10:15. doi: 10.1186/1472-6831-10-15 [Crossref] [ Google Scholar]
- Nico MM, Park JH, Lourenço SV. Mucocele in pediatric patients: analysis of 36 children. Pediatr Dermatol 2008; 25(3):308-11. doi: 10.1111/j.1525-1470.2008.00672.x [Crossref] [ Google Scholar]
- Yamasoba T, Tayama N, Syoji M, Fukuta M. Clinicostatistical study of lower lip mucoceles. Head Neck 1990; 12(4):316-20. doi: 10.1002/hed.2880120407 [Crossref] [ Google Scholar]
- Oliveira DT, Consolaro A, Freitas FJ. Histopathological spectrum of 112 cases of mucocele. Braz Dent J 1993; 4(1):29-36. [ Google Scholar]
- Jani DR, Chawda J, Sundaragiri SK, Parmar G. Mucocele-a study of 36 cases. Indian J Dent Res 2010; 21(3):337-40. doi: 10.4103/0970-9290.70793 [Crossref] [ Google Scholar]
- Bowers EM, Schaitkin B. Management of mucoceles, sialoceles, and ranulas. Otolaryngol Clin North Am 2021; 54(3):543-51. doi: 10.1016/j.otc.2021.03.002 [Crossref] [ Google Scholar]
- Lopez-Jornet P, Bermejo-Fenoll A. Point of care: what is the most appropriate treatment for salivary mucoceles? Which is the best technique for this treatment. J Can Dent Assoc 2004; 70(7):484-5. [ Google Scholar]
- Essaket S, Hakkou F, Chbicheb S. [Mucocele of the oral mucous membrane]. Pan Afr Med J 2020; 35:140. doi: 10.11604/pamj.2020.35.140.21079.[French] [Crossref] [ Google Scholar]
- Yadav A, Grover H, Yadav P, Nanda P. A novel technique for the treatment of mucocele: a case report. Arch Dent Sci 2011; 2(2):33-5. [ Google Scholar]
- Yagüe-García J, España-Tost AJ, Berini-Aytés L, Gay-Escoda C. Treatment of oral mucocele-scalpel versus CO2 laser. Med Oral Patol Oral Cir Bucal 2009; 14(9):e469-74. [ Google Scholar]
- Yeh CJ. Simple cryosurgical treatment for oral lesions. Int J Oral Maxillofac Surg 2000; 29(3):212-6. [ Google Scholar]