Avicenna J Dent Res. 16(3):134-139.
doi: 10.34172/ajdr.1759
Original Article
Primary Stability and Osseointegration of the Implant in an Iatrogenically Oversized Cavity by Bone Substitute: An Animal Study
Mohammad Reza Jamalpour 1, 2  , Seyed Masoud Zolhavarieh 3, Hamid Zarei 4, *, Alireza Soltanian 5, Farshid Vahdatinia 2
, Seyed Masoud Zolhavarieh 3, Hamid Zarei 4, *, Alireza Soltanian 5, Farshid Vahdatinia 2 
Author information:
1Department of Oral and Maxillofacial Surgery, Hamadan University of Medical Sciences, Hamadan, Iran
2Dental Implants Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
3Veterinary Surgeon, Bu-Ali Sina University, Hamadan, Iran
4Oral and Maxillofacial Surgeoon, Private practice, Tehran, Iran
5Department of Biostatistics, Hamadan University of Medical Sciences, Hamadan, Iran
Abstract
Background: The aim of this study was to compare the success rate of autogenous bone and combination of autogenous bone and beta-tricalcium phosphate (β-TCP) grafts in restoring the primary stability and osseointegration of dental implants after the oversized preparation of the bone cavity in animal models.
Methods: Three months after extracting 3 premolars from 4 male Terrier dogs, 24 implants were inserted in cavities larger than the fixture size. Then, based on the type of graft materials around the implant fixture, they were randomly divided into the autogenous bone group (A, n=8), the autogenous bone group with β-TCP (B, n=8), and the control group with no grafts (C, n=8). After 16 weeks, the removal torque quantity (RTQ) test and Periotest® were used for osseointegration assessment.
Results: According to the results of the RTQ test, group B was significantly higher than group C (P=0.022), but no statistical difference was observed between groups A and B, as well as groups A and C. Based on the results, the Periotest® value significantly differed in group B compared to groups A (P=0.049) and C (P=0.014), but there was no difference between groups A and C in this regard.
Conclusion: According to the findings of the study, the combination of autogenous bone graft and TCP could improve secondary stability and osseointegration of dental implants.
Keywords: Dental implant, Primary stability, Autogenous bone graft, Tricalcium phosphate
Copyright and License Information
© 2024 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Jamalpour MR, Zolhavarieh SM, Zarei H, Soltanian A, Vahdatinia F.. Primary stability and osseointegration of the implant in an iatrogenically oversized cavity by bone substitute: an animal study. Avicenna J Dent Res. 2024; 16(3):134-139. doi:10.34172/ajdr.1759
Background
According to the Branemark paradigm, good primary stability immediately after implant insertion plays a key role in establishing optimal secondary stability and long-term success (1,2). However, achieving proper primary stability is not always easy, and, in some cases, such as insufficient bone volume and poor bone quality, it is a major challenge for the surgeon (3,4).
Insufficient stability of the fixture inside the cavity during the healing time and the occurrence of micromotions above a threshold of 50–100 μm cause the failure of the osseointegration process and result in the formation of fibrous tissue instead of bone. Therefore, it is highly important to use alternative methods in order to achieve proper stability of the fixture inside the implant cavity or to improve the osseointegration process (5,6).
Modifying the contact surfaces of the implant with the bone by creating surface roughness through acid etching or the coating of biocompatible materials can play an important role in increasing bone formation around the implant and improving the osseointegration process (5). Further, using larger diameter fixtures is another routine measure in the case of an unintentional increase in the size of the implant cavity (7). In addition, the use of autogenous bone or other types of bone substitutes is the proposed method to prevent osseointegration failure in cases of inadequate primary stability (7).
Various compounds are available as bone substitutes, including calcium phosphate ceramics, which behave similarly to bone (8,9). Although beta-tricalcium phosphate (β-TCP)is highly similar to hydroxyapatite (HA), it is not considered a natural bone material. However, the β-TCP in the body can be converted into HA (8). The rate of resorption and durability of this material depend on the characteristics of its chemical structure, porosity, and particle size. β-TCP is osteoconductive and forms a physical matrix that is highly suitable for the deposition of a new bone. Furthermore, β-TCP can be used to restore non-pathological defects. The combination of β-TCP with osteoinductive or osteogenic materials can increase the graft quality. β-TCP is safe and well-tolerated by the body (8,10).
Various methods have been introduced for evaluating implant stability before and after surgery. The most important methods for assessing the stability and osseointegration of implants after surgery are radiographic, percussion, Periotest, and measurement of insertion and cutting torque. Radiography can be considered for both pre-operative and post-operative assessments. Bone quality and quantity analysis is one of the most important pre-operative assessments performed by cone-beam computerized tomography. Moreover, crestal bone changes are measured through conventional radiographic techniques as a common post-operative examination. Periotest evaluation is based on Periotest values (PTVs), in which electromagnetic signal generation is determined in the range of (-8) to (+50), and PTV decreases with an increase in implant stability (11). Additionally, the reverse torque quantity (RTQ) test, based on the study by Sennerby et al, is considered another important value for measuring the interfacial shear strength between the fixture and bone tissue (12,13).
According to the above-mentioned evidence, this study sought to evaluate the ability of the autogenous bone and autogenous-β-TCP graft to improve the primary stability and osseointegration of dental implants after the improper preparation of cavities in the dog’s jaw.
Materials and Methods
Overall, four 2-year-old adult male dogs that were healthy according to veterinary examinations were used in this animal study. The study was approved by the Ethics Committee of Hamadan University of Medical Sciences (Exclusive ID No. D/P/16/35/9/2755). Then, the vaccination was completely performed, and all animals were kept individually in the Animal Care Center of Hamadan University of Medical Sciences. All animals had free access to water and food.
Preliminary Surgery
In the preliminary surgery, the first, second, and third mandibular premolars on both sides were extracted under general anesthesia. The anesthesia regimen consisted of acepromazine 2% (0.1 mg/kg IV), ketamine 10% (20 mg/kg IV), atropine sulfate 0.6 mg/cc (0.04-0.05 mg/kg IV), and xylazine 2% (1.1 mg/kg IV) (14).
It is worth noting that due to the high pull-out strength and thin periodontal ligament space of the dog’s premolar teeth, the roots of the teeth were removed by performing full-thickness flaps and using a standard surgical handpiece. Before incision closure, intraoral periapical radiographs were prepared for each quadrant to ensure complete removal of the roots. Finally, the flap was sutured using 4/0 chromic, and the dogs received oral antibiotics at a dose of 20 mg/kg (suspension amoxicillin) for 5 days.
The First-Stage Surgery of Implantation
Three months after the healing process (15), each specimen was anesthetized by a veterinarian using a combination of ketamine, xylazine, and acepromazine (as mentioned), along with a continuous infusion of Ringer’s lactate serum. Then, periapical radiographs were taken under general anesthesia using a radiopaque reference to measure the height of the mandibular bone ridge. Next, both mandibular nerves were blocked by the injection of 2% lidocaine, and the edentulous bone ridge was exposed by mucoperiosteal flaps. After drilling three oversized cavities on each side, the samples were allocated to two experimental groups and a control group with three-block randomization and closed envelope concealment:
-
Implant + autogenous bone graft
-
Implant + autogenous bone graft and β-TCP (KASIOS TCP Dental HP, France)
-
Implant without any graft material (control)
Therefore, 24 implants (SM, DIO, Implant, Busan, Korea) were placed in the oversized cavities. According to the size of the fixtures (8 x 3.8 mm, SM, DIO, Implant, Busan, Korea), the size of the drilled cavities was prepared with a diameter of 4.5 mm (two drills more than the designated drill for diameter 3.8) and a depth of 10 mm, so that after placing the fixtures inside the cavity (the fixtures were 0.35 mm away from the cavity wall), no stability was observed using tissue forceps.
KASIOS TCP Dental HP is a high-porosity (90%) synthetic bone substitute with total interconnection. Due to this porosity and its chemical composition (β-TCP), when placed in a bone site, it is replaced in 6 or 7 months by new bone.
The veterinary surgeon harvested the thirteenth rib of each specimen under aseptic conditions as an autograft. Then, the harvested bone was crushed using a bone mill (Surgical Smart, British Columbia, Canada) and then placed in two experimental cavities with or without β-TCP. In the experimental groups (A and B), after holding the fixture in the center of oversized cavities by a fixture driver, the free space between the fixtures and cavity walls was filled with bone substitutes. The graft material was packed until the fixtures were immobile during the placement of the rod of Periotest®. The control group (C) was still left without any graft material, and the fixtures were placed while they were loose in their cavities.
The primary stability of the fixtures in the A and B groups was measured with Periotest® (Medizintechnik Gulden, Modautal, Germany). Periotest® has a rod that comes out of the device and strikes fixtures or abutments in the form of a magnetic pulse at a certain speed (16).
Two-stage surgery was applied to all fixtures, and after closing the cover screw with a 10 N/cm torque, the flaps were closed using a 4/0 chromic suture. The antibiotic diet, including Gentamycin (40 mg/one dose daily) and Penicillin G (400 000 U/two doses daily), was administered for 5 days. Additionally, for the first 24 hours after the surgery, the liquid diet was used, and then the soft diet was established for up to 2 weeks.
The Second-Stage Surgery of Implantation
After 4 months, the second-stage surgery was performed under general anesthesia for uncovering fixtures and evaluating the osseointegration of fixtures. At this stage, Periotest® was used to measure the degree of osseointegration of each fixture (Figure 1).
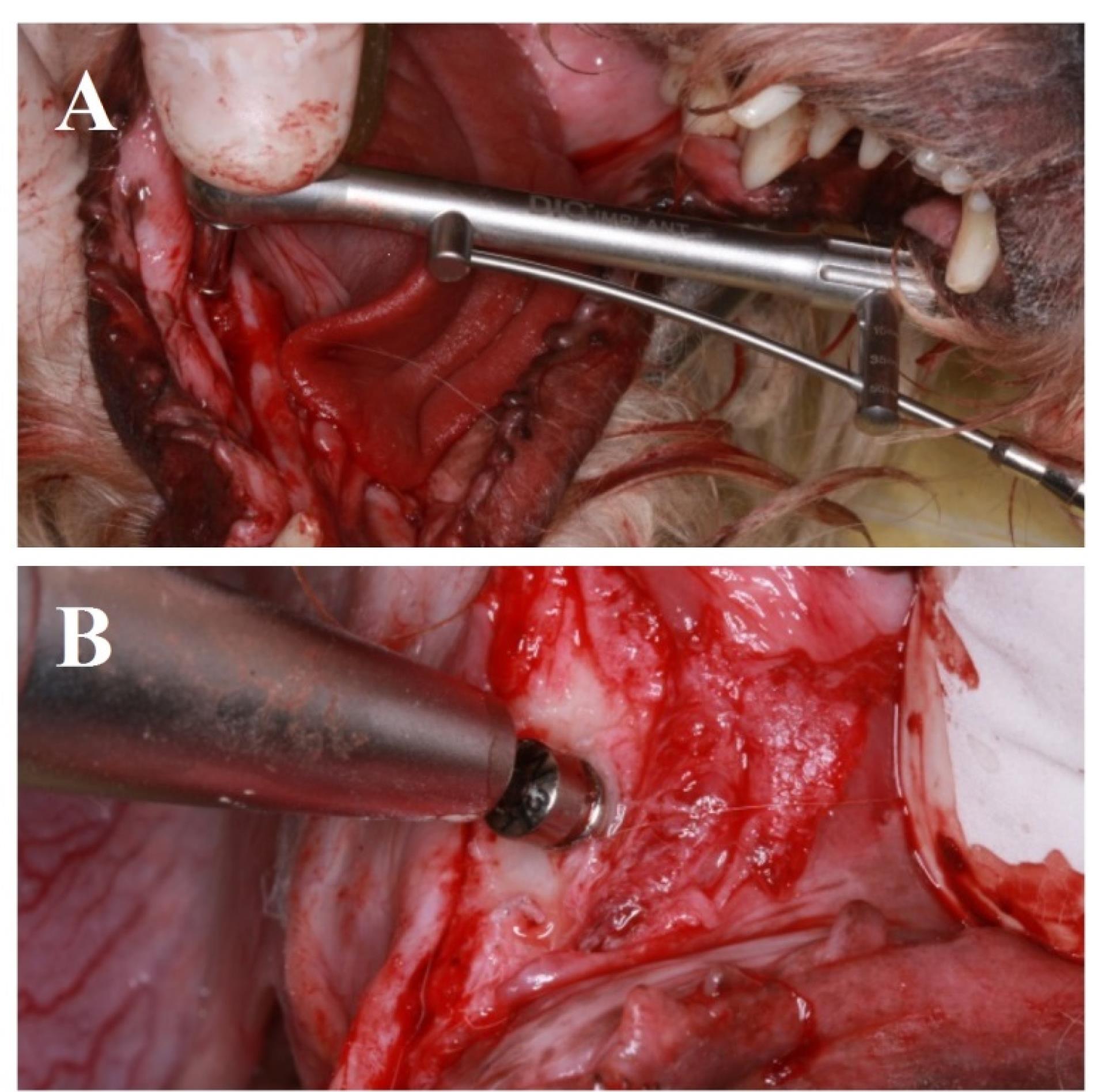
Figure 1.
A. RTQ test and B. Periotest® examination. Note. RTQ: Reverse torque quantity
.
A. RTQ test and B. Periotest® examination. Note. RTQ: Reverse torque quantity
In addition, RTQ in Newton centimeters (N/cm) was utilized to evaluate the shear strength between implants and bone tissue. A dental implant Ratchet and Torque Wrench (DIO, Busan, Korea) was employed in this test. Finally, the flaps were closed using 4/0 chromic sutures (Figure 1).
Results
After 4 months, the implants were exposed, and 18 out of the 24 implants remained in the jaws of the specimens. The other 6 were not present in the area. The frequency of residual implants was as follows:
-
6 in the autograft group (group A)
-
7 in the alloplastic-autograft group (B)
-
5 in the control group (C)
According to the results of the statistical analysis (Table 1) and the Monte-Carlo simulation, no significant difference was found between the survival ratios in the three groups.
Table 1.
Results of Statistical Analysis and the Monte-Carlo Simulation Related to the Survival Ratios of Implants in the A, B, and C Groups
|
Groups
|
|
Outcome
|
Exact-test
(
P
Value)
|
Monte-Carlo
P
Value
(99% CI)
|
|
Non-durable
|
Durable
|
Total
|
| C (controls) |
Count |
3 |
5 |
8 |
1.33
(0.837) |
0.842*
(0.80-0.88) |
| % Within groups |
37.5% |
62.5% |
100.0% |
| A (autograph) |
Count |
2 |
6 |
8 |
| % Within groups |
25.0% |
75.0% |
100.0% |
| B (alloplastic-autograph) |
Count |
1 |
7 |
8 |
| % Within groups |
12.5% |
87.5% |
100.0% |
|
|
Note. *Based on 500 sampled tables with starting seed 1502173562. CI: Confidence interval.
Reverse Torque Quantity Index
The RTQ test is an important value for measuring the interfacial shear strength between fixtures and bone tissue (12). All implants remaining in the jaw had RTQs above 35 N/cm, so there was no significant difference between the three groups (P > 0.05).
Periotest Value
PTv (PT) value is determined in the range of (-8) to (+50), and PT decreases with an increase in the stability of the implant (11). The Kruskal-Wallis test demonstrated that the mean PT was not the same in all three groups before (A = 7.00, B = 7, C = 7) and after (A = -7.00, B = -7.85, C = -3.20) surgery, and an improvement in the mean PT was observed in the second surgery. Furthermore, the highest and lowest PT values after performing the second surgery in groups A (-6,-8) and B (-7,-8) were both in the negative range, while a positive PT value was detected in the C group (+3,-8), the details of which are shown in Table 2 and Figure 2.
Table 2.
Descriptive Results of Periotest® of Osseointgrated Implants Related to A, B, and C Groups
|
Groups
|
PT-Before
|
PT-After
|
| Autograft |
N |
6 |
6 |
| Mean |
7.0000 |
-7.0000 |
| Standard deviation |
0.00000 |
0.89443 |
| Minimum |
7.00 |
-8.00 |
| Maximum |
7.00 |
-6.00 |
| Autograft + alloplastic |
N |
7 |
7 |
| Mean |
7.0000 |
-7.8571 |
| Standard deviation |
.00000 |
0.37796 |
| Minimum |
7.00 |
-8.00 |
| Maximum |
7.00 |
-7.00 |
| Control |
N |
5 |
5 |
| Mean |
7.0000 |
-3.2000 |
| Standard deviation |
0.00000 |
4.32435 |
| Minimum |
7.00 |
-8.00 |
| Maximum |
7.00 |
3.00 |
| Total |
N |
18 |
18 |
| Mean |
7.0000 |
-6.2778 |
| Standard deviation |
0.00000 |
2.94669 |
| Minimum |
7.00 |
-8.00 |
| Maximum |
7.00 |
3.00 |
Note. PT: Periotest; Std. deviation; Standard deviation.
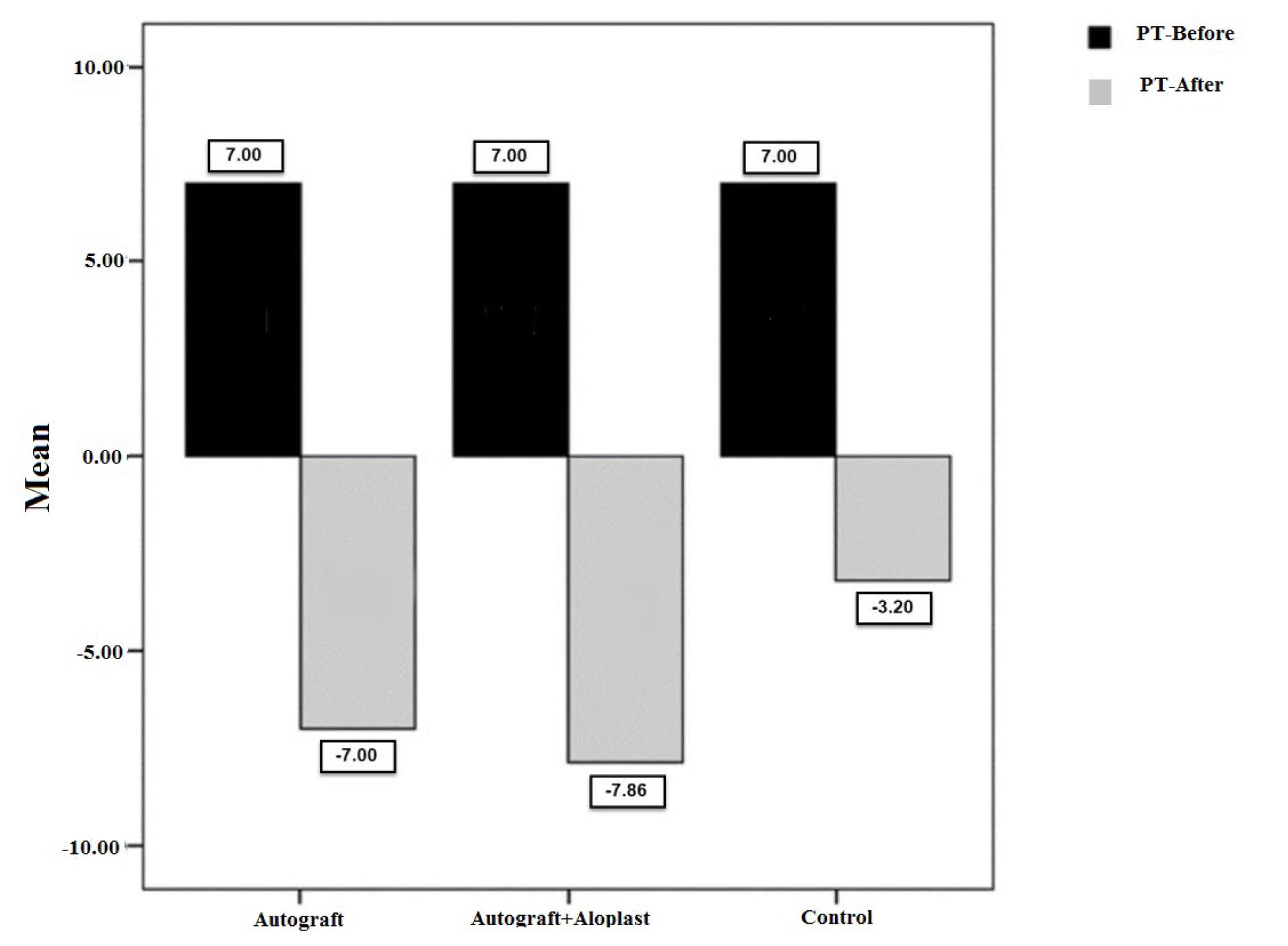
Figure 2.
The Mean PT Values Before and After Surgery in the Study and Control Groups Note. PT: Periotest
.
The Mean PT Values Before and After Surgery in the Study and Control Groups Note. PT: Periotest
The results of the Mann-Whitney U test (Table 3) revealed that there was a statistically significant difference in the PT index between groups A and B (P = 0.049). However, no significant difference was found between groups A and C (P = 0.093). On the other hand, a statistically significant difference was observed after comparing the PT index between groups B and C (P = 0.014).
Table 3.
Results of the Mann-Whitney U Test for the PT Index
|
Test
|
Groups
|
Mean Rank
|
P
Value
|
| PT |
Autogenous bone graft |
9.00 |
0.049 |
| Autogenous bone graft and TCP |
5.29 |
| Autogenous bone graft |
4.50 |
0.093 |
| Control |
7.80 |
| Autogenous bone graft and TCP |
4.57 |
0.014 |
| Control |
9.20 |
Note. PT: Periotest; TCP: Tricalcium phosphate.
Discussion
There was no significant difference between the three groups in terms of the number of osseointegrated fixtures. Although, due to the small number of specimens, it cannot be concluded with certainty, it seems that there is a possibility of obtaining osteointegration in cases where the implant cavity is too large and the fixture has no primary stability. Moreover, it may not be necessary to postpone the fixture implantation and extend the treatment period for several months. According to the results of this study, it is recommended to achieve primary stability by using a bone substitute in the large cavity.
Based on the results of the study, all the remaining fixtures were stable and did not move with a 35 N/cm reverse torque. In other words, when the fixtures remained in the cavity, osteointegration could be created even without any intervention. It seems that the main reason for osteointegration is immobilization through the insertion of fixtures 1 mm below the surface of the bone crest. However, according to the PT index, there was a significant difference between the three groups in terms of the success of secondary stability.
The highest quality was obtained when the combination of the alloplast-autogenous bone was used for gaining primary stability, which was significantly different from the autogenous bone or C group. However, the quality of osteointegration was not significantly different between the autogenous bone and control groups. In this regard, Ivanova et al, based on the findings of a clinical study, emphasized that bone density and the percentage of vital bone formation determine the primary and secondary stability of the implants (17).
The slow rate of resorption (in comparison to bone) of β-TCP crystals increased the strength of the graft material, likely improved the quality of the osseointegration process, and reduced the volume of the harvesting bone graft. It seems that the osteoconductive properties and slow rate of resorption of β-TCP make it a reliable structure for the osteogenic effects of the autogenous bone graft. Furthermore, β-TCP is a safe substitute and well-tolerated by the body (15,18).
On the other hand, the results of the study performed by Huang et al on bone defects in the dog mandible showed that bone repair in cavities filled with HA was histologically superior to the C group (without any grafts) (19). In addition, the findings of the study by Kim et al on a biomaterial containing calcium and phosphorus, such as TCP, demonstrated its positive effects on inducing osseointegration and restoring the stability of implants with larger cavities in terms of transverse and longitudinal dimensions (20). This finding could be due to the function of CaP in improving surface biointeractivity during initial osseointegration (21). Further, the results of our study confirmed that osseointegration was significantly increased by the combination of TCP and an autogenous bone graft.
Another factor that plays a crucial role in achieving adequate primary stability is the presence of an appropriate three-dimensional contact surface between the implant and the surrounding bone. Hsu et al stated that increasing the contact surface improves the primary stability (22). In an animal study of compromised primary stability, Queiroz et al also found that implant placement without primary stability and in cavities with a gap of less than 0.2 mm between the fixture and the bone could achieve osteointegration. According to their findings, the use of polylactide and polyglycolide copolymers (PLA/PGA) had no effect on improving the osseointegration process (7). The results of this study also indicated that the simultaneous use of the autogenous bone graft and TCP caused a significant improvement in secondary stability, and therefore, increasing the contact surface can be considered an important cause.
Although there was no statistically significant difference between the RTQ and PT of the autogenous and C groups in this study, the improvement in the mean of both indices in the autogenous group was another emphasis on the positive effects of bone growth factors on the quality of osseointegration.
Conclusion
The combination of the autogenous bone graft and TCP improved the secondary stability and osseointegration of implant treatments. Therefore, this method can be used to restore the primary stability of implants in larger cavities. Nevertheless, due to the small number of specimens, it cannot be concluded with certainty, and conducting studies with a larger number of samples can help achieve more accurate results.
Acknowledgments
This study has been adapted from a research project submitted to Hamadan University of Medical Sciences (No. 9110193767).
Authors’ Contribution
Conceptualization: Mohammad Reza Jamalpour.
Data curation: Mohammad Reza Jamalpour, Hamid Zarei.
Formal analysis: Alireza Soltanian.
Investigation: Mohammad Reza Jamalpour, Seyed Masoud Zolhavarieh, Hamid Zarei.
Methodology: Mohammad Reza Jamalpour, Seyed Masoud Zolhavarieh, Hamid Zarei, Alireza Soltanian.
Project administration: Mohammad Reza Jamalpour, Hamid Zarei
Resources: Mohammad Reza Jamalpour, Hamid Zarei.
Software: Hamid Zarei, Alireza Soltanian, Farshid Vahdatinia.
Supervision: Mohammad Reza Jamalpour.
Validation: Mohammad Reza Jamalpour, Seyed Masoud Zolhavarieh, Hamid Zarei, Alireza Soltanian, Farshid Vahdatinia.
Visualization: Mohammad Reza Jamalpour, Seyed Masoud Zolhavarieh, Hamid Zarei.
Writing–original draft: Mohammad Reza Jamalpour, Hamid Zarei, Alireza Soltanian, Farshid Vahdatinia.
Writing–review & editing: Mohammad Reza Jamalpour, Farshid Vahdatinia.
Competing Interests
The authors declare that there is no conflict of interests.
Ethical Approval
The study was approved by the Committee of Ethics in Hamadan University of Medical Sciences (Exclusive ID No. D/P/16/35/9/2755).
Funding
Deputy of research of Hamadan University of Medical Sciences (No. 9110193767).
References
- Al-Sabbagh M, Eldomiaty W, Khabbaz Y. Can osseointegration be achieved without primary stability?. Dent Clin North Am 2019; 63(3):461-73. doi: 10.1016/j.cden.2019.02.001 [Crossref] [ Google Scholar]
- Staedt H, Heimes D, Lehmann KM, Ottl P, Bjelopavlovic M, Wagner W. Does the modification of the apical geometry of a dental implant affect its primary stability? A comparative ex vivo study. Materials (Basel) 2021; 14(7):1728. doi: 10.3390/ma14071728 [Crossref] [ Google Scholar]
- Fanuscu MI, Chang TL, Akça K. Effect of surgical techniques on primary implant stability and peri-implant bone. J Oral Maxillofac Surg 2007; 65(12):2487-91. doi: 10.1016/j.joms.2007.04.017 [Crossref] [ Google Scholar]
- Rues S, Schmitter M, Kappel S, Sonntag R, Kretzer JP, Nadorf J. Effect of bone quality and quantity on the primary stability of dental implants in a simulated bicortical placement. Clin Oral Investig 2021; 25(3):1265-72. doi: 10.1007/s00784-020-03432-z [Crossref] [ Google Scholar]
- Kim MS, Jung UW, Kim S, Lee JS, Lee IS, Choi SH. Bone apposition on implants coated with calcium phosphate by ion beam assisted deposition in oversized drilled sockets: a histologic and histometric analysis in dogs. J Periodontal Implant Sci 2013; 43(1):18-23. doi: 10.5051/jpis.2013.43.1.18 [Crossref] [ Google Scholar]
- Cohen O, Ormianer Z, Tal H, Rothamel D, Weinreb M, Moses O. Differences in crestal bone-to-implant contact following an under-drilling compared to an over-drilling protocol A study in the rabbit tibia. Clin Oral Investig 2016; 20(9):2475-80. doi: 10.1007/s00784-016-1765-8 [Crossref] [ Google Scholar]
- Queiroz TP, Souza F, Okamoto R, Luvizuto ER, Margonar R, Garcia IR Jr. Compromised primary implant stability. J Craniofac Surg 2012; 23(5):e524-8. doi: 10.1097/SCS.0b013e31825b3863 [Crossref] [ Google Scholar]
- Bouwman WF, Bravenboer N, Ten Bruggenkate CM, Eijsackers FA, Stringa N, Schulten E. Tissue level changes after maxillary sinus floor elevation with three types of calcium phosphate ceramics: a radiological study with a 5-year follow-up. Materials (Basel) 2021; 14(6):1471. doi: 10.3390/ma14061471 [Crossref] [ Google Scholar]
- Batas L, Stavropoulos A, Papadimitriou S, Nyengaard JR, Konstantinidis A. Evaluation of autogenous PRGF + β-TCP with or without a collagen membrane on bone formation and implant osseointegration in large size bone defects A preclinical in vivo study. Clin Oral Implants Res 2016; 27(8):981-7. doi: 10.1111/clr.12742 [Crossref] [ Google Scholar]
- Meredith N, Alleyne D, Cawley P. Quantitative determination of the stability of the implant-tissue interface using resonance frequency analysis. Clin Oral Implants Res 1996; 7(3):261-7. doi: 10.1034/j.1600-0501.1996.070308.x [Crossref] [ Google Scholar]
- Ajeebi AM, Alquraishi SA. Primary stability of dental implant: a review International Journal of Medicine in Developing Countries. 2020 A ug 5; 4(8):1281-6. doi: 10.24911/ijmdc.51-1586791181 [Crossref] [ Google Scholar]
- Calvo-Guirado JL, Satorres M, Negri B, Ramirez-Fernandez P, Maté-Sánchez de Val JE, Delgado-Ruiz R. Biomechanical and histological evaluation of four different titanium implant surface modifications: an experimental study in the rabbit tibia. Clin Oral Investig 2014; 18(5):1495-505. doi: 10.1007/s00784-013-1120-2 [Crossref] [ Google Scholar]
- Sennerby L, Dasmah A, Larsson B, Iverhed M. Bone tissue responses to surface-modified zirconia implants: A histomorphometric and removal torque study in the rabbit. Clin Implant Dent Relat Res 2005; 7 Suppl 1:S13-20. doi: 10.1111/j.1708-8208.2005.tb00070.x [Crossref] [ Google Scholar]
- Adams HR. Veterinary Pharmacology and Therapeutics. Ames: Iowa State University Press; 2001.
- Mayer Y, Zigdon-Giladi H, Machtei EE. Ridge preservation using composite alloplastic materials: a randomized control clinical and histological study in humans. Clin Implant Dent Relat Res 2016; 18(6):1163-70. doi: 10.1111/cid.12415 [Crossref] [ Google Scholar]
- Tricio J, Laohapand P, van Steenberghe D, Quirynen M, Naert I. Mechanical state assessment of the implant-bone continuum: a better understanding of the Periotest method. Int J Oral Maxillofac Implants 1995; 10(1):43-9. [ Google Scholar]
- Ivanova V, Chenchev I, Zlatev S, Mijiritsky E. Correlation between primary, secondary stability, bone density, percentage of vital bone formation and implant size. Int J Environ Res Public Health 2021; 18(13):6994. doi: 10.3390/ijerph18136994 [Crossref] [ Google Scholar]
- Menezes JD, dos Santos Pereira R, Bonardi JP, Griza GL, Okamoto R, Hochuli-Vieira E. Bioactive glass added to autogenous bone graft in maxillary sinus augmentation: a prospective histomorphometric, immunohistochemical, and bone graft resorption assessment. J Appl Oral Sci 2018; 26:e20170296. doi: 10.1590/1678-7757-2017-0296 [Crossref] [ Google Scholar]
- Huang MS, Wu HD, Teng NC, Peng BY, Wu JY, Chang WJ. In vivo evaluation of poorly crystalline hydroxyapatite-based biphasic calcium phosphate bone substitutes for treating dental bony defects. J Dent Sci 2010; 5(2):100-8. doi: 10.1016/s1991-7902(10)60014-1 [Crossref] [ Google Scholar]
- Kim DS, Lee WJ, Choi SC, Lee SS, Heo MS, Huh KH. A new method for the evaluation of dental implant stability using an inductive sensor. Med Eng Phys 2012; 34(9):1247-52. doi: 10.1016/j.medengphy.2011.12.012 [Crossref] [ Google Scholar]
- Zamparini F, Prati C, Generali L, Spinelli A, Taddei P, Gandolfi MG. Micro-nano surface characterization and bioactivity of a calcium phosphate-incorporated titanium implant surface. J Funct Biomater 2021; 12(1):3. doi: 10.3390/jfb12010003 [Crossref] [ Google Scholar]
- Hsu JT, Huang HL, Tsai MT, Wu AY, Tu MG, Fuh LJ. Effects of the 3D bone-to-implant contact and bone stiffness on the initial stability of a dental implant: micro-CT and resonance frequency analyses. Int J Oral Maxillofac Surg 2013; 42(2):276-80. doi: 10.1016/j.ijom.2012.07.002 [Crossref] [ Google Scholar]