Avicenna J Dent Res. 16(1):28-34.
doi: 10.34172/ajdr.1750
Original Article
Accuracy of Panoramic Radiography in Comparison With Cone-Beam Computed Tomography for the Detection of Idiopathic Osteosclerosis: An Original Cross-sectional Study
Samareh Mortazavi 1  , Najmeh Anbiaee 1
, Najmeh Anbiaee 1  , Sara Mishian 2
, Sara Mishian 2  , Berahman Sabzevari 3, *
, Berahman Sabzevari 3, * 
Author information:
1Department of Oral and Maxillofacial Radiology, Dental School, Mashhad University of Medical Sciences, Mashhad, Iran
2General Dentist, Gorgan, Iran
3Orthodontist, Private Practice, Mashhad, Iran
Abstract
Background: The accuracy of radiography for the detection of bone lesions is a critical issue. This study aimed to assess the accuracy of panoramic radiography in comparison with cone-beam computed tomography (CBCT) for the detection of idiopathic osteosclerosis (IO).
Methods: This cross-sectional study was conducted on imaging records of 201 patients who had both panoramic radiographs and CBCT scans. Panoramic radiographs of patients were evaluated for lesions suspected of IO. After two weeks, the accuracy of diagnoses was investigated by assessing the patients’ CBCT scans. The location, number, shape, internal structure, and size of lesions and their relationship with teeth were also assessed on CBCT scans using Romexis Viewer software, version 3.8.0. Data were analyzed by the chi-square test (alpha=0.05).
Results: Of all, 73.4% of IO lesions were correctly diagnosed on panoramic radiographs, yielding an accuracy of 0.85 for this modality. IO lesions were detected in 51 patients (n=64 lesions, 25.73%), mainly located in the mandibular molar (45.3%) and premolar (29.7%) regions. All lesions were well-defined, and most of them were spherical (42.1%). The majority of them had a cortical internal structure (73.4%) and did not correlate with teeth (78.1%). The mean size of large and small diameters of lesions was 5.4 and 3.1 mm, respectively.
Conclusion: Identifying the radiographic characteristics of common lesions such as IO can be a guide for dentists to avoid incorrect treatments and unnecessary biopsies. In this way, panoramic radiography with 0.85 accuracy helps in diagnosing these lesions.
Keywords: Osteosclerosis, Cone-beam computed tomography, Radiography, Panoramic
Copyright and License Information
© 2024 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Mortazavi S, Anbiaee N, Mishian S, Sabzevari B. Accuracy of panoramic radiography in comparison with cone-beam computed tomography for the detection of idiopathic osteosclerosis: an original cross-sectional study. Avicenna J Dent Res. 2024; 16(1):28-34. doi:10.34172/ajdr.1750
Background
After sclerosing osteitis, idiopathic osteosclerosis (IO) is the second most common radiopacity of the jawbone (1). In a recent study, Hlongwa et al have shown that IO is the most common incidental pathologic finding after altered tooth morphology in orthodontic patients (2). It has no known definite cause and is defined as increased calcification or local proliferation of dense cortical bone within the cancellous bone, which may be single or multiple (3). It may develop due to genetic, neoplastic, hematological, infectious, metabolic, or gastrointestinal disorders (4). IO is not exclusive to the jawbone but is also found in the hip, femur, and some other long bones (5). It is incidentally found in bony areas on radiographs and has the highest frequency in premolar-molar regions. It often varies in size from 2 mm to 2 cm (6,7). IO commonly occurs in the mandible and may be close to the inferior border of the mandible (6).
Gardner syndrome is a genetic disorder and a subgroup of familial adenomatous polyposis that occurs as the result of mutations in the adenomatous polyposis coli gene. This mutation results in the formation of several polyps in the colon, and such patients are at high risk of colon cancer. Multiple osteomas and dense bone islands (DBIs) are among other characteristics of this syndrome. Osteomas may be absent in some cases. However, the presence of five or more DBIs may indicate familial adenomatous polyposis syndrome. Osteomas and DBIs are often detected before the colon polyps, thus their early detection is important for early diagnosis of this syndrome (8).
Dentists are in the first line of encountering oral lesions. Therefore, their adequate knowledge and appropriate techniques for the early detection of such lesions are highly important. Such lesions are often detected as an incidental finding on radiographs since they are asymptomatic (9).
Panoramic radiography is an accurate imaging modality commonly requested for a comprehensive assessment of oral and facial structures (10). It can also show dental anomalies and pathological or traumatic bony lesions (8). However, the two-dimensional nature, distortion, blurring, and superimposition of anatomical structures are among its limitations that can compromise its diagnostic accuracy (11). Some recent efforts have been made to use an artificial intelligence system for the accurate detection of IO radiographs on panoramic radiographs (12). Cone-beam computed tomography (CBCT) is a novel three-dimensional imaging modality with high resolution and a lower patient radiation dose than CT. It does not cause image distortion or superimposition of structures. It has high scanning speed and affordable cost and can be used as the gold standard for comparison with other imaging modalities (13-16). CBCT can also be utilized as the gold standard for the correct diagnosis of IO of the jaw. Considering all the above-mentioned explanations, this study aimed to assess the accuracy of panoramic radiography in comparison with CBCT for the detection of IO.
Materials and Methods
This retrospective cross-sectional study was conducted on the imaging records of 201 patients who had both panoramic radiographs and CBCT scans in their records. The imaging records were selected from the archives of a private radiology clinic in Mashhad, Iran.
Eligibility Criteria
The inclusion criteria were the availability of both CBCT and panoramic radiographs of patients and high quality of images.
Sample Size
The sample size was calculated to be 193 according to a study by Radic et al (11), assuming a 95% confidence interval and a 90% study power. Overall, 200 samples were enrolled to increase the accuracy of the results.
Assessments
A total of 55 maxillary and 60 mandibular CBCT scans and 86 CBCT scans of both the maxilla and mandible (a total of 146 CBCT scans of the maxilla and 141 CBCT scans of the mandible) were evaluated in this study. All images were taken with a Planmeca ProMax 3D Mid CBCT scanner (Helsinki, Finland), with the exposure settings of 90 kVp and 10 mA with a 10 × 10 cm field of view. The voxel size was 0.2 mm. All CBCT scans were evaluated by Romexis Viewer, version 3.8.0 (Planmeca, Helsinki, Finland). The panoramic images were obtained with the Scara 3 X-ray unit (Planmeca, Finland). The age and gender of patients were also recorded.
A Lenovo Z41 monitor (China) with a resolution of 1920 × 1080 was used to view the images. Changing the brightness and contrast of the image was allowed according to the needs of the observers.
The background light in the place where the images were examined was set indirectly and gently.
All images were evaluated by a senior dental student under the supervision of an oral and maxillofacial radiologist (with 8 years of experience). Magnification was used if required, and cases of disagreement were discussed with a second radiologist (with 20 years of experience).
The panoramic images of all patients were primarily evaluated for the presence of IO. After a 2-week interval, their CBCT scans were evaluated as the gold standard to verify the diagnosis of IO made according to the panoramic radiographs.
For the assessment of CBCT scans by Planmeca Romexis (version 3.8.0), initially, each jaw was separately selected, and then its plane was adjusted in the axial and sagittal planes using the draw panoramic curve feature of the software. Next, on cross-sectional views, the 1 × 1 feature was selected from the viewport setting menu, and the images were precisely assessed from one side of the jaw to the other side for the presence of IO. The coronal and axial sections were also examined if further assessments were necessary (Figure 1).
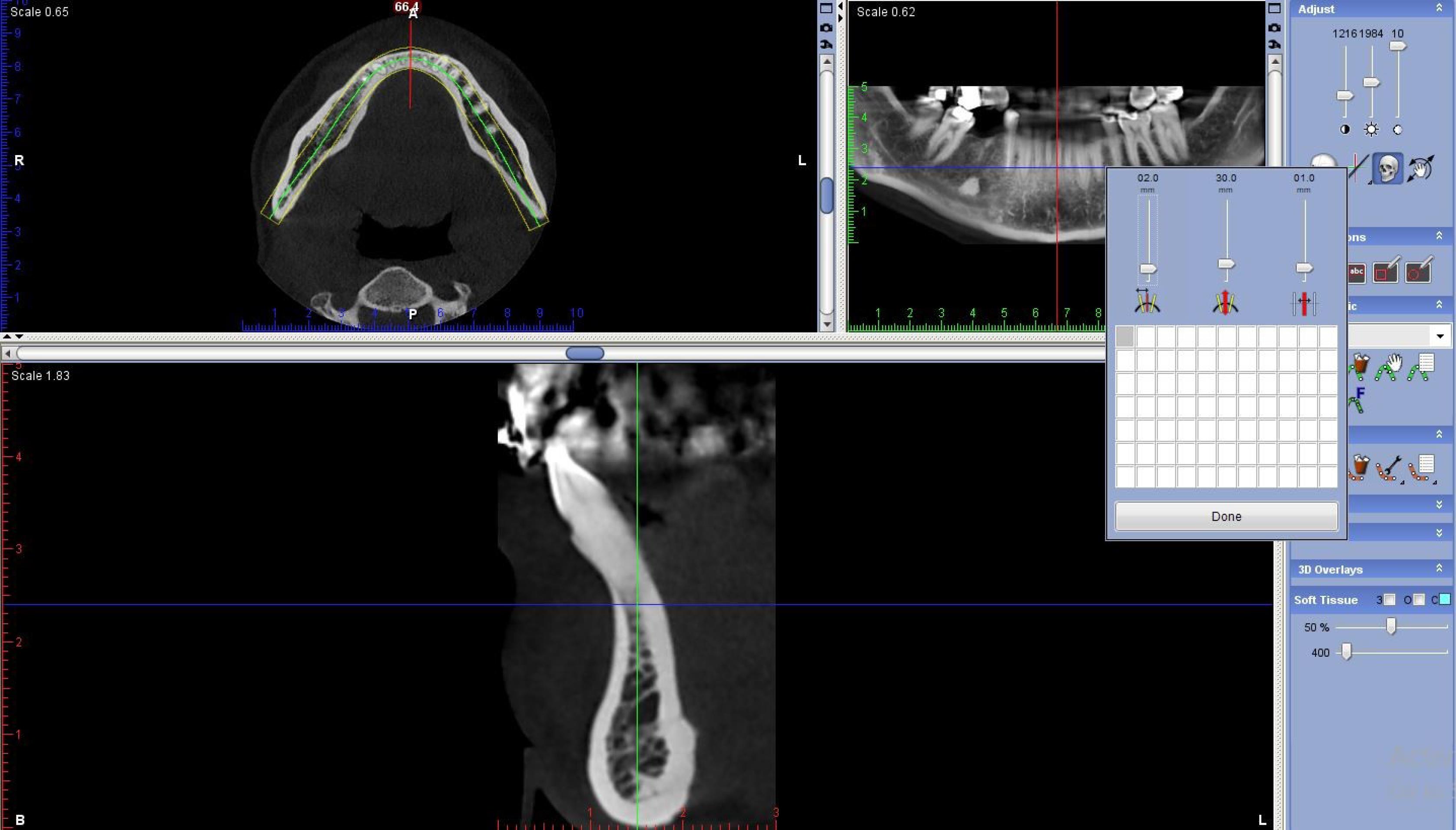
Figure 1.
Assessment of the Cross-sectional View
.
Assessment of the Cross-sectional View
Subsequently, in the case of the presence of IO, the large and small diameters of the lesion were measured by choosing the measure length feature on the cross-section visualizing the largest size of the lesion (Figure 2).

Figure 2.
Measurement of the Lesion Size
.
Measurement of the Lesion Size
The lesions were measured on different sections, depending on their direction of extension.
Shape of Lesions
According to a study by Imani Moghaddam and Eatemadi-Sadjadi (4), the IO lesions were divided into 6 groups based on their shapes (irregular, tubular, saddle-shaped, spherical, oval, and triangular), which are depicted in Figure 3 (Schematic and radiographic view).
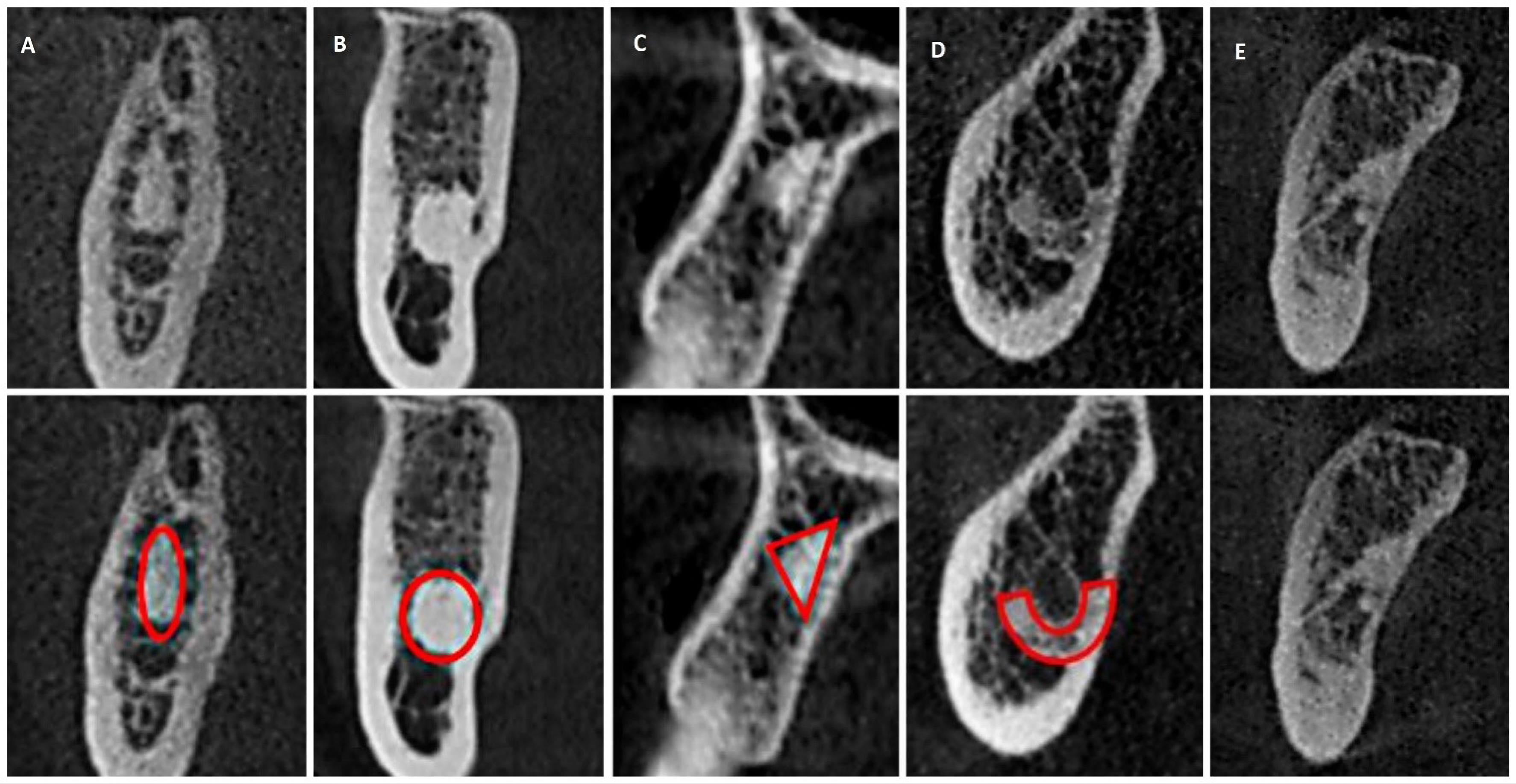
Figure 3.
Different Shapes of IO Lesions: (A) Oval, (B) Spherical, (C) Triangular, (D) Saddle-shaped, and (E) Irregular. Note. IO: Idiopathic osteosclerosis
.
Different Shapes of IO Lesions: (A) Oval, (B) Spherical, (C) Triangular, (D) Saddle-shaped, and (E) Irregular. Note. IO: Idiopathic osteosclerosis
Periphery of Lesions
The lesions were categorized as well-defined or ill-defined based on their periphery.
Internal Structure of Lesions
The lesions were categorized into cortical, trabecular, and mixed groups based on their internal structure.
Correlation of Lesions With Teeth
The lesions were classified into the following five groups according to their correlation with teeth based on a study by Sisman et al (17):
-
Inter-radicular: The IO lesion is confined to the inter-radicular area.
-
Apical: The IO lesion is at the root apex.
-
Apical/inter-radicular: The IO lesion is at the root apex and extends to the inter-radicular area. Separate: The IO lesion is not related to the root apex and lamina dura.
-
Separate/inter-radicular: The IO lesion is not related to the root apex and lamina dura and is confined to the inter-radicular area (Figure 4).
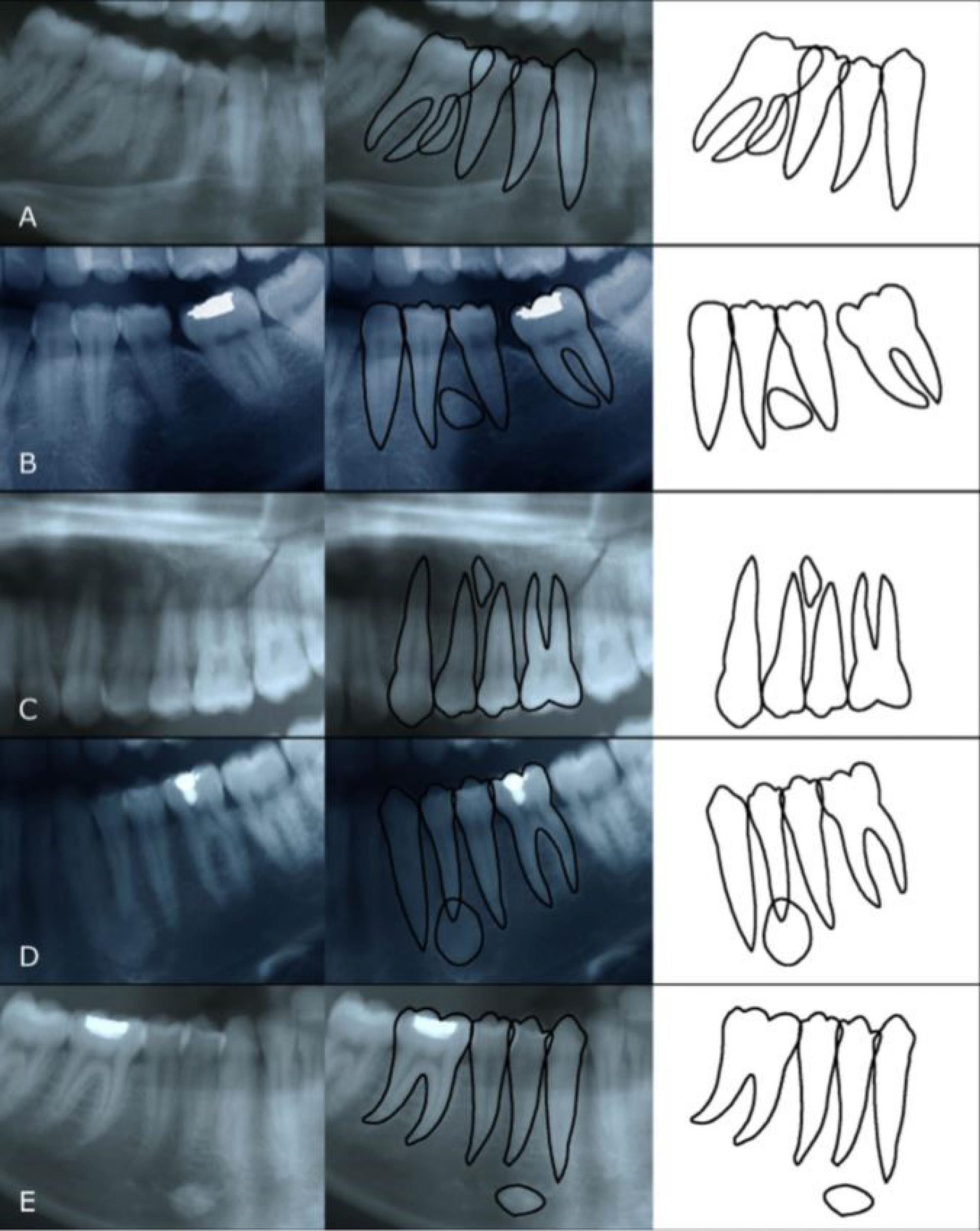
Figure 4.
Relationship Between IO and Teeth: (A) Inter-radicular, (B) Separate/Inter-radicular, (C) Apical/Inter-radicular, (D) Apical, and (E) Separate. Note. IO: Idiopathic osteosclerosis. Reproduced from Sisman under the Creative Commons CC-BY-NC-ND license
.
Relationship Between IO and Teeth: (A) Inter-radicular, (B) Separate/Inter-radicular, (C) Apical/Inter-radicular, (D) Apical, and (E) Separate. Note. IO: Idiopathic osteosclerosis. Reproduced from Sisman under the Creative Commons CC-BY-NC-ND license
Root Resorption
Root resorption was also evaluated in lesions related to the teeth.
Location of Lesion
In terms of location, the lesions were assigned to anterior, premolar, molar, and angle and ramus/tuberosity groups (18).
Statistical Analysis
Sensitivity, specificity, positive and negative predictive values, and accuracy were calculated. Sensitivity and specificity were defined as the number of correctly diagnosed IO lesions based on panoramic radiographs and the correct detection of absence of IO, respectively. Comparisons were made by the chi-square test at a 0.05 level of significance using SPSS, version 24 (SPSS Inc., IL, USA).
Results
A total of 201 patients, including 101 females (50.2%) and 100 males (49.8%), with a mean age of 47.45 ± 13.81 years (range 6 to 75 years), participated in this study. The mean number of IO lesions was 0.63 ± 0.32. Of all 201 patients, 150 did not have IO. Overall, 64 cases of IO were found in 51 patients; of whom, 42 (20.9%) had one, 6 (3%) had two, 2 (1%) had three, and 1 (0.5%) had four lesions. Thus, 25.37% of patients had IO. The assessment of 64 IO lesions revealed that 50% of the cases (n = 32) were observed in males, and 50% (n = 32) belonged to females. No case of root resorption was found based on the results.
Location of Lesions
Table 1 presents the location of IO lesions. The mandibular molar region had the highest (45.3%), while the maxillary molar and anterior regions had the lowest (0%) frequency of IO.
Table 1.
Location of IO Lesions
|
Location of IO
|
|
Jaw
|
Anterior, No. (%)
|
Premolar, No. (%)
|
Molar, No. (%)
|
Ramus, Angle, Tuberosity, No. (%)
|
Total
|
| Maxilla |
0 (0) |
3 (4.7) |
0 (0) |
2 (3.1) |
5 (7.8) |
| Mandible |
7 (10.9) |
19 (29.7) |
29 (45.3) |
4 (6.3) |
59 (92.2) |
| Total |
7 (10.9) |
22 (34.4) |
29 (45.3) |
6 (9.4) |
64 (100) |
Note. IO: Idiopathic osteosclerosis.
Correlation With Teeth
Among 64 IO lesions, the separate type had the highest frequency (n = 50, 78.1%), while the inter-radicular and apical types had the lowest frequency (n = 1, 1.6%).
Borders
All 64 IO lesions were well-defined.
Shape
Among 64 IO lesions, spherical lesions (n = 27, 42.1%) had the highest prevalence (n = 27, 42.1%), whereas saddle-shaped lesions had the lowest prevalence (n = 1, 1.5%). Figure 5 shows the frequency distribution of different shapes of IO lesions.
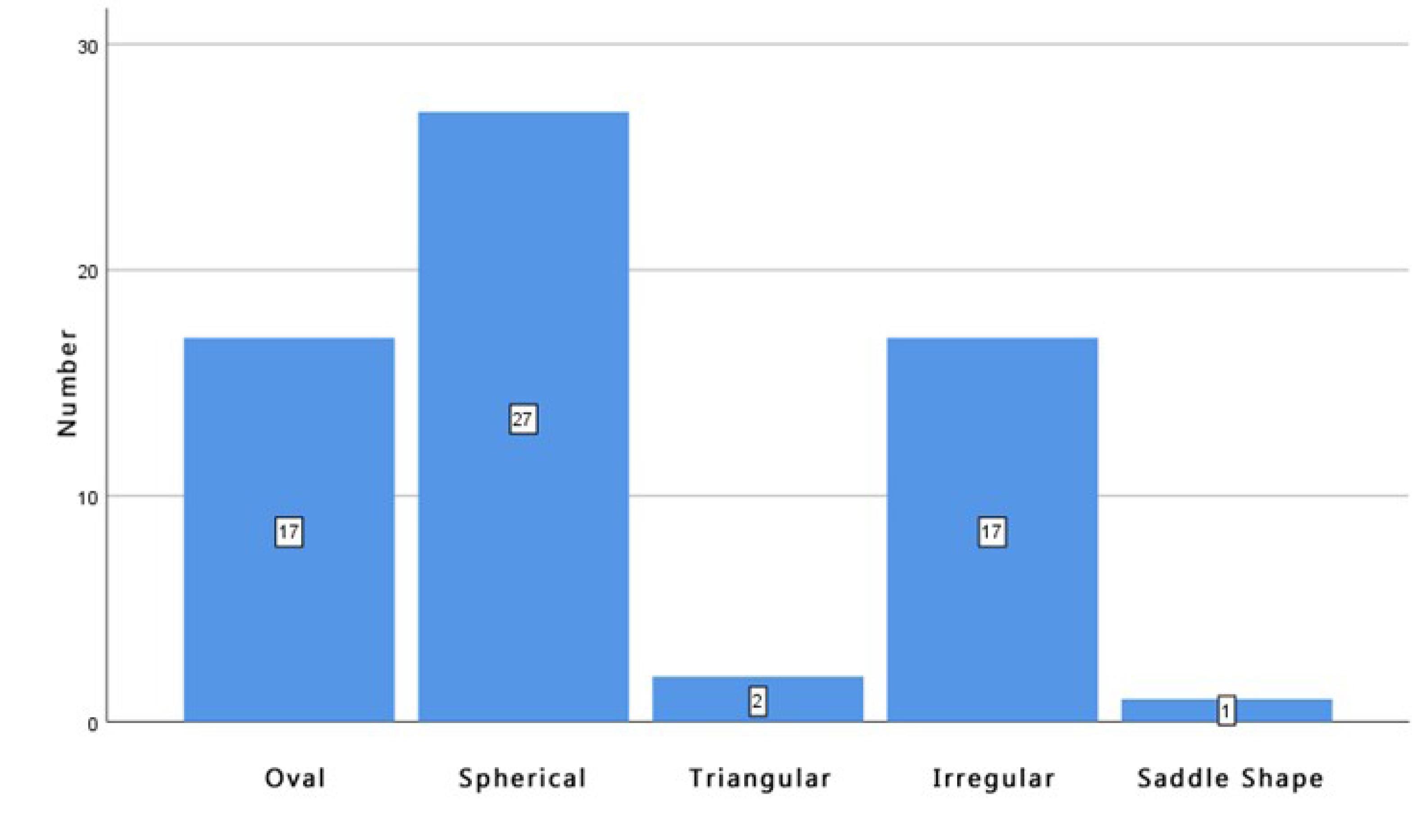
Figure 5.
Frequency Distribution of Different Shapes of IO Lesions. Note. IO: Idiopathic osteosclerosis
.
Frequency Distribution of Different Shapes of IO Lesions. Note. IO: Idiopathic osteosclerosis
Diameters of IO Lesions
The mean length of the small diameter of IO lesions was 3.48 ± 1.25 mm (range of 2–7 mm), and that of the large diameter of IO lesions was 5.62 ± 1.82 mm (range of 3–10 mm).
Comparison of Panoramic Radiography and Cone-beam Computed Tomography
Each jaw was separately evaluated to more precisely compare the two imaging modalities. In addition, each detected IO lesion underwent a separate analysis. Accordingly, the two techniques were compared in 313 cases of IO lesions (Table 2).
Table 2.
Frequency of Detection of IO Lesions by Panoramic Radiography and CBCT
|
Diagnosis Based on Panoramic Radiography and CBCT
|
Number
|
Percent
|
| IO was not detected on any of them. |
198 |
63.3 |
| Both detected IO. |
47 |
15.0 |
| Panoramic radiography detected IO, but CBCT did not confirm it. |
31 |
9.9 |
| Panoramic radiography did not detect IO but CBCT detected it. |
17 |
5.4 |
| Panoramic radiography and CBCT yielded different diagnoses. |
20 |
6.4 |
|
Total
|
313 |
100.0 |
Note. IO: Idiopathic osteosclerosis; CBCT: Cone-beam computed tomography.
According to the CBCT diagnoses as the gold standard, panoramic radiography correctly detected IO in 73.5% (n = 47), while it could not detect IO in 26.5% (n = 17) of the cases. The highest frequency of wrong diagnoses of IO lesions by panoramic radiography was due to residual roots (n = 13; 10 at the molar, 2 at the premolar, and 1 in the tuberosity site). Sclerosing osteitis ranked second (n = 3; 2 at the molar and 1 at the premolar site). Florid cemento-osseous dysplasia at the molar and genial tubercle, sclerotic socket in the anterior region, and calcified lymph node at the ramus all ranked third, each observed in 1 case.
Calculation of Diagnostic Indices
Table 3 presents the frequency of correct and incorrect diagnoses of IO by panoramic radiography in comparison with CBCT. As shown, panoramic radiography had a sensitivity of 0.73, a specificity of 0.87, a positive predictive value of 0.60, a negative predictive value of 0.93, and a diagnostic accuracy of 0.85.
Table 3.
Frequency of Correct and Incorrect Diagnoses of IO by Panoramic Radiography in Comparison With CBCT
|
Radiography
|
CBCT
|
|
Yes
|
No
|
Total
|
| OPG |
Yes |
47 |
31 |
78 |
| No |
17 |
218 |
235 |
| Total |
64 |
249 |
313 |
Note. IO: Idiopathic osteosclerosis; OPG: Orthopantomogram; CBCT: Cone-beam computed tomography.
Discussion
This study assessed the accuracy of panoramic radiography in comparison with CBCT for the detection of IO. As mentioned earlier, IO is an asymptomatic radiopaque localized lesion with no expansion and no specific etiology, which is often accidentally found on radiographs and requires no treatment. Thus, familiarity with its radiographic manifestations is important to prevent unnecessary biopsy and differentiate it from other radiopaque bony lesions, particularly sclerosing osteitis. Furthermore, since multiple DBIs develop before intestinal polyps in Gardner syndrome and that patients are at high risk of colon cancer, early radiographic detection of this syndrome by dentists is highly important and can aid in prompt treatment (8).
The prevalence of IO lesions in different populations ranges from 1.7% to 31% using different radiographic modalities (19). The frequency of IO in the present study was found to be 25.37%, which is almost in agreement with the results of Demir and Pekiner (19) on a Turkish population (26.9%) and those of Austin and Moule (20) on a Chinese population (31%). However, this frequency rate was almost 3 times higher than that reported by Azizi et al (18) in Iran (8.33%) and Farhadi et al (21) in Iran (7.5%), and over 2 times higher than the rates reported by Imani Moghaddam and Eatemadi-Sadjadi (4) in Iran (9%) and Lu et al (22) on a Thai population (9.43%). Such a controversy in the reported prevalence rates can be due to the use of different radiographic modalities (panoramic radiography versus CBCT).
In the present study, IO had a higher frequency in the mandible than in the maxilla (92.2% versus 7.8%). The mandibular molar region (45.3%) was more commonly involved, followed by the premolar region (29.7%), which is in line with the available literature (17-19,23,24).
In the current study, the frequency of IO was the same in males and females, which conforms to the results of some studies (4,18,19), while contradicting those of some other studies that reported its higher predilection for females (25,26).
In the present study, the separate type was the most frequent correlation of IO lesions with teeth (78.1%), followed by the apical type (15%). The inter-radicular and apical type had the lowest frequency (1.5%). Similar results were reported in the literature (4,18,19). However, Geist and Katz (26) and many others (17,21,26,27) demonstrated that the apical type had the highest frequency in their study populations. Such variation in the results can be due to racial differences and different radiographic techniques. For instance, Geist and Katz (26) found a full series of periapical radiography in their study. The 10 lesions with apical correlation with teeth did not cause root resorption. However, Azizi et al (18) showed that of 5 apical lesions, 1 had caused root resorption. Most IO lesions were spherical (42.1%), followed by irregular shape (26.5%), which matches the results of Ledesma-Montes et al (23) and Azizi et al (18). The mean size of large and small diameters of lesions was 5.4 and 3.1 mm, respectively, in the present study. All lesions were well-defined, and the majority of them had a cortical internal structure (73.4%). These findings differ from the findings of Imani Moghaddam and Eatemadi-Sadjadi (4), which is most probably due to the difference in the type of radiographic modality (panoramic radiography in their study). The main goal of the present study was to assess the accuracy of panoramic radiography for the detection of IO in comparison with CBCT as the gold standard. The results revealed that panoramic radiography had a sensitivity of 0.73, a specificity of 0.87, a positive predictive value of 0.60, a negative predictive value of 0.93, and a diagnostic accuracy of 0.85. Similarly, Schreiner-Tiefenbacher et al (28) reported a 63.5% agreement between the diagnosis of IO by panoramic radiography and three-dimensional (3D) imaging, and of all IO lesions detected on 3D images, 79.7% were detected on panoramic radiographs. In the present study, although IO was misdiagnosed in 16.3% of the cases by panoramic radiography, this modality had adequately high accuracy (0.85) and approximately 76% agreement with CBCT and can serve as a low-cost modality with a low radiation dose for the detection of IO.
Using CBCT as the gold standard was the main strength of the present study. Moreover, IO lesions were evaluated on all CBCT sections, which was another strength. However, a wide age range of patients and the unavailability of their medical records due to the retrospective nature of the study were among the limitations of this study.
Future studies are required to assess the relationship of IO with the inferior alveolar nerve. Additionally, the agreement of panoramic radiography and CBCT findings with histological analysis may be evaluated in further studies.
Conclusion
IO lesion had a relatively high prevalence and was found in 25.7% of our statistical population. Therefore, dentists should have the necessary familiarity with the radiographic appearance of this lesion to differentiate it from similar lesions. Gardner’s syndrome should be ruled out, particularly if several IO lesions are observed. Panoramic radiography with an accuracy of 0.85 can be helpful as a suitable radiography for initial screening and investigation of random findings such as IO.
Acknowledgements
The authors would like to gratefully acknowledge the Vice-Chancellor of Research of Mashhad University of Medical Sciences for the financial support of this project.
Authors’ Contribution
Conceptualization: Samareh Mortazavi and Najmeh Anbiaee.
Data curation: Samareh Mortazavi and Sara Mishian.
Formal analysis: Samareh Mortazavi and Berahman Sabzevari.
Funding acquisition: Samareh Mortazavi and Najmeh Anbiaee.
Investigation: Samareh Mortazavi and Sara Mishian.
Methodology: Samareh Mortazavi and Najmeh Anbiaee.
Project administration: Samareh Mortazavi and Najmeh Anbiaee.
Resources: Samareh Mortazavi and Najmeh Anbiaee.
Software: Sara Mishian and Berahman Sabzevari.
Supervision: Samareh Mortazavi, Najmeh Anbiaee.
Validation: Samareh Mortazavi and Sara Mishian.
Visualization: Samareh Mortazavi and Sara Mishian.
Writing–original draft: Samareh Mortazavi and Berahman Sabzevari.
Writing–review and editing: Samareh Mortazavi and Berahman Sabzevari.
Competing Interests
There is no conflict of interests to declare.
Ethical Approval
This study was approved by the Ethics Committee of Mashhad University of Medical Sciences (ethical approval No. IR.MUMS.DENTISTRY.REC.1400.057).
Funding
This study was financially supported by the Vice-Chancellor of Research of Mashhad University of Medical Sciences (Research Project No. 4000257).
References
- Wood N, Goaz P. Differential Diagnosis of Oral and Maxillofacial Lesions. 5th ed. Michigan: Mosby; 1997. p. 480.
- Hlongwa P, Moshaoa MA, Musemwa C, Khammissa RA. Incidental pathologic findings from orthodontic pretreatment panoramic radiographs. Int J Environ Res Public Health 2023; 20(4):3479. doi: 10.3390/ijerph20043479 [Crossref] [ Google Scholar]
- Ezaddini F, Salari M. Idiopatic osteo sclerosis. J Shahid Sadoughi Univ Med Sci 2004;12(3):58-64. [Persian].
- Imani Moghaddam M, Eatemadi-Sadjadi M. Radiographic evaluation of idiopathic osteosclerosis in patients referring to Mashhad dental school from November 2002 to May 2004. J Shahid Sadoughi Univ Med Sci 2006;14(2):61-7. [Persian].
- Greenspan A. Bone island (enostosis): current concept--a review. Skeletal Radiol 1995; 24(2):111-5. doi: 10.1007/bf00198072 [Crossref] [ Google Scholar]
- Halse A, Molven O. Idiopathic osteosclerosis of the jaws followed through a period of 20-27 years. Int Endod J 2002; 35(9):747-51. doi: 10.1046/j.1365-2591.2002.00561.x [Crossref] [ Google Scholar]
- Misirlioglu M, Nalcaci R, Adisen MZ, Yilmaz S. The evaluation of idiopathic osteosclerosis on panoramic radiographs with an investigation of lesion′s relationship with mandibular canal by using cross-sectional cone-beam computed tomography images. J Oral Maxillofac Radiol 2013; 1(2):48-54. doi: 10.4103/2321-3841.120108 [Crossref] [ Google Scholar]
- White SC, Pharoah MJ. White and Pharoah’s Oral Radiology: Principles and Interpretation. 8th ed. Missouri: Elsevier; 2019. p. 437.
- Costa AG, Costa RO, de Oliveira LR, Grossmann S. Multiple oral radiopaque masses leading to Gardner’s syndrome diagnosis. Gen Dent 2013; 61(4):e12-4. [ Google Scholar]
- Sklavos A, Beteramia D, Delpachitra SN, Kumar R. The panoramic dental radiograph for emergency physicians. Emerg Med J 2019; 36(9):565-71. doi: 10.1136/emermed-2018-208332 [Crossref] [ Google Scholar]
- Radic J, Patcas R, Stadlinger B, Wiedemeier D, Rücker M, Giacomelli-Hiestand B. Do we need CBCTs for sufficient diagnostics?-dentist-related factors. Int J Implant Dent 2018; 4(1):37. doi: 10.1186/s40729-018-0147-1 [Crossref] [ Google Scholar]
- Yesiltepe S, Bayrakdar IS, Orhan K, Çelik Ö, Bilgir E, Aslan AF. A deep learning model for idiopathic osteosclerosis detection on panoramic radiographs. Med Princ Pract 2022; 31(6):555-61. doi: 10.1159/000527145 [Crossref] [ Google Scholar]
- Mehdizadeh M, Torabinia A, Kasaei S, Farhad F. Evaluation of the prevalence of accidental findings in maxillary sinus in the CBCT archives of Isfahan Faculty of Dentistry. J Isfahan Dent Sch 2015;11(3):223-9. [Persian].
- Maillet M, Bowles WR, McClanahan SL, John MT, Ahmad M. Cone-beam computed tomography evaluation of maxillary sinusitis. J Endod 2011; 37(6):753-7. doi: 10.1016/j.joen.2011.02.032 [Crossref] [ Google Scholar]
- Pazera P, Bornstein MM, Pazera A, Sendi P, Katsaros C. Incidental maxillary sinus findings in orthodontic patients: a radiographic analysis using cone-beam computed tomography (CBCT). Orthod Craniofac Res 2011; 14(1):17-24. doi: 10.1111/j.1601-6343.2010.01502.x [Crossref] [ Google Scholar]
- Varshosaz M, Sharifi S. Cone beam volumetric tomography versus conventional computed tomography in evaluation of paranasal sinuses. Tehran Univ Med J 2010;68(7):406-11. [Persian].
- Sisman Y, Ertas ET, Ertas H, Sekerci AE. The frequency and distribution of idiopathic osteosclerosis of the jaw. Eur J Dent 2011; 5(4):409-14. [ Google Scholar]
- Azizi Z, Mosafery H, Safi Y, Dabirzadeh S, Vasegh Z. Prevalence of idiopathic osteosclerosis on cone beam computed tomography images. J Dent Sch 2017; 35(2):67-70. doi: 10.22037/jds.v35i2.24626 [Crossref] [ Google Scholar]
- Demir A, Pekiner FN. Idiopathic osteosclerosis of the jaws in Turkish subpopulation: cone-beam computed tomography findings. Clin Exp Health Sci 2019; 9(2):117-23. doi: 10.33808/clinexphealthsci.563958 [Crossref] [ Google Scholar]
- Austin BW, Moule AJ. A comparative study of the prevalence of mandibular osteosclerosis in patients of Asiatic and Caucasian origin. Aust Dent J 1984; 29(1):36-43. doi: 10.1111/j.1834-7819.1984.tb04541.x [Crossref] [ Google Scholar]
- Farhadi F, Razavi Ruhani M, Zarandi A. Frequency and pattern of idiopathic osteosclerosis and condensing osteitis lesions in panoramic radiography of Iranian patients. Dent Res J (Isfahan) 2016; 13(4):322-6. doi: 10.4103/1735-3327.187880 [Crossref] [ Google Scholar]
- Lu PC, Chuang FH, Roan RT, Chen JH. The prevalence of idiopathic osteosclerosis and condensing Ostitis in South Taiwan population. J Dent Res 2003; 82:B300. [ Google Scholar]
- Ledesma-Montes C, Jiménez-Farfán MD, Hernández-Guerrero JC. Idiopathic osteosclerosis in the maxillomandibular area. Radiol Med 2019; 124(1):27-33. doi: 10.1007/s11547-018-0944-x [Crossref] [ Google Scholar]
- Yonetsu K, Yuasa K, Kanda S. Idiopathic osteosclerosis of the jaws: panoramic radiographic and computed tomographic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997; 83(4):517-21. doi: 10.1016/s1079-2104(97)90156-6 [Crossref] [ Google Scholar]
- McDonnell D. McDonnell DDense bone islandA review of 107 patients. Oral Surg Oral Med Oral Pathol 1993; 76(1):124-8. doi: 10.1016/0030-4220(93)90307-p [Crossref] [ Google Scholar]
- Geist JR, Katz JO. The frequency and distribution of idiopathic osteosclerosis. Oral Surg Oral Med Oral Pathol 1990; 69(3):388-93. doi: 10.1016/0030-4220(90)90307-e [Crossref] [ Google Scholar]
- Kawai T, Hirakuma H, Murakami S, Fuchihata H. Radiographic investigation of idiopathic osteosclerosis of the jaws in Japanese dental outpatients. Oral Surg Oral Med Oral Pathol 1992; 74(2):237-42. doi: 10.1016/0030-4220(92)90389-8 [Crossref] [ Google Scholar]
- Schreiner-Tiefenbacher B, Forster V, Pauli K, Sutter W, Meier M, Roland H. Evaluation of mandibular calcification on 3D volume images. Heliyon 2019; 5(5):e01698. doi: 10.1016/j.heliyon.2019.e01698 [Crossref] [ Google Scholar]