Avicenna J Dent Res. 16(2):97-107.
doi: 10.34172/ajdr.1741
Review Article
A Simple Approach for the Diagnosis of Oral Ulcers: A Novel Algorithm
Fatemeh Ahmadi-Motamayel 1  , Fereshteh Najar-Karimi 2, *
, Fereshteh Najar-Karimi 2, *  , Deniz Safabakhsh 3
, Deniz Safabakhsh 3  , Fatemeh Abbasi 4, Parya Atapour 5
, Fatemeh Abbasi 4, Parya Atapour 5  , Laleh Shahabi 6
, Laleh Shahabi 6 
Author information:
1Dental Implants Research Center and Dental Research Center, Department of Oral Medicine, School of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran
2Department of Oral and Maxillofacial Medicine, School of Dentistry, Alborz University of Medical Sciences, Karaj, Iran./
3Razi Herbal Medicines Research Center, School of Dentistry, Lorestan University of Medical Sciences, Khorramabad, Iran.
4Department of Oral Medicine, School of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran.
5Department of Oral and Maxillofacial Medicine, Faculty of Dentistry, Tabriz University of Medical Sciences, Tabriz, Iran
6Department of Oral and Maxillofacial Medicine, School of Dentistry, Yasuj University of Medical Sciences, Yasuj, Iran
Abstract
Ulcers are one of the most common lesions in the oral cavity and are caused by injuries to the oral mucosa for different reasons. These ulcers are clinically characterized by the loss of the whole thickness of the epithelium and the denuding of the underlying lamina propria in the presence of a white/yellow layer called the fibrinoleukocytic layer and are usually accompanied by pain. Due to the wide array of etiologic agents for oral ulcers, pinpointing the etiologic agent can be highly challenging, and the availability of a good diagnostic guide assists in the diagnosis and selection of proper treatment modalities because a fast and accurate diagnosis of some ulcers (e.g., the early stages of squamous cell carcinoma) is crucial for the early initiation of treatment. The present study attempts to present a proper and comprehensive diagnostic guide to facilitate the classification and diagnosis of different oral ulcers.
Keywords: Diagnosis, Oral Ulcer, Algorithm
Copyright and License Information
© 2024 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Ahmadi-Motamayel F, Najar-Karimi F, Safabakhsh D, Abbasi F, Atapour P; Shahabi L. A simple approach for the diagnosis of oral ulcers: a novel algorithm. Avicenna J Dent Res. 2024; 16(2):97-107. doi:10.34172/ajdr.1741
Background
An oral ulcer is defined as a disruption of the integrity of the oral mucosa and denuding of the underlying connective tissue, typically surrounded by an erythematous halo (1). During the diagnostic workup, the first priority is paying attention to the patient’s chief complaint. Then, it is necessary to evaluate its history, including the history and course of the condition up to now, the medical and dental history, family history, patient’s habits (e.g., smoking, alcohol use, and the like), social and personal history, and a thorough evaluation of the body systems (e.g., respiratory, digestive, and other symptoms and signs). Next, extraoral (to cover the skin and other mucosal structures) and intraoral examinations are performed, and subsequently, depending on the need, proper preclinical tools (e.g., radiography) and laboratory tests (e.g., biopsies and histopathologic samples) are used to reach a final diagnosis and prepare an appropriate treatment plan (2).
One of the most important clinical criteria that can assist in the diagnostic workup of oral ulcers is to evaluate the presence or absence of a history of ulcers or other lesions in the skin and other mucosa, symptoms and signs such as fever, malaise, arthritis, and the like, and the presence of blisters or vesicles in association with the ulcers. In addition, culturing or biopsy procedures and histopathological evaluation of the samples are sometimes necessary, especially with the immunofluorescence technique (3).
Considering that ulcers might be a nonspecific sign of some background conditions, it is a challenge to pinpoint the etiologic factor(s) for oral ulcers, mostly due to the wide range of ulcer types (chronic and acute) and reasons (trauma, systemic conditions, and the like) for their induction. Correct treatment depends on the correct and early diagnosis of the etiologic agents and a precise understanding of the immunopathologic nature of the lesions (4,5). The present study discusses the differential diagnosis of different oral lesions.
In the present study, ulcers are initially classified into aphthous-, map-, and cater-like categories based on their shape.
Aphthous-Like Ulcers
These ulcers are divided into two subgroups, namely, recurrent (similar, recurring ulcers with frequent healing) and non-recurring ulcers. Further, each subgroup is again categorized based on the presence or absence of other concomitant symptoms and signs.
Recurrent Ulcers
Without Accompanying Symptoms and Signs
Recurrent Aphthous Stomatitis: It is a condition with recurrent ulcers that is highly common and painful. The most common age of onset is childhood and adolescence, with an unknown etiology. The predisposing conditions include genetics, stress, local trauma, nutritional deficiencies, and the like. This condition is diagnosed based on history and clinical findings and mostly occurs as solitary or multiple, small, round, or oval (symmetrical) ulcers with an erythematous halo in the non-keratinized mucosa. Based on their size, these ulcers are categorized into minor and major RAS and herpetiform. Minor RAS is the most common type, with ulcers measuring 3‒10 mm; healing takes place spontaneously in 10‒14 days, without scars. Major RAS includes deeper ulcers that are irregular, and longer and measure > 10 mm; healing occurs with scars and might take weeks or months and might be accompanied by fever, dysphagia, and weakness. Herpetiform is the least common type, which mostly occurs in women, with several small 2‒3-mm ulcers up to 10‒100 in number that tend to merge to form large, irregular ulcers (6,7).
With Accompanying Symptoms and Signs
Aphthous and oral ulcers might be detected in association with other clinical findings in many systemic, autoimmune, and other conditions.
Δ Aphthous-dependent syndromes: This group includes classic oral aphthous ulcers associated with other symptoms and signs and is divided into three groups based on the signs and affected locations:
-
Behçet’s syndrome: It is a recurrent systemic vasculitis with an unknown etiology that affects several organs, including the oral-genital mucosa. The principal triad of this condition includes ocular, genital, and oral mucosal involvement (the most common clinical finding is in the form of several RAS ulcers with minor, major, and herpetiform types, mostly affecting the non-keratinized mucosa). The prevalence of this condition is higher in young adults (20‒40 years of age), and it is more severe in women than in men (8,9).
-
Periodic fever, aphthous stomatitis, pharyngitis, and adenitis syndrome: It is the most common self-limiting condition with periodic fever in children that mostly appears at 5 years of age and resolves at adolescence in most cases. In this condition, periodic fever appears with at least one of the three main symptoms and signs, namely, pharyngitis, aphthous stomatitis (in 50% of the cases, small round ulcers in the non-keratinized mucosa), and/or oral adenitis (10,11). This syndrome is diagnosed based on history (no contact with an etiologic agent/an infected patient) and clinical findings (10).
-
Mouth and genital ulcers with inflamed cartilage syndrome: This syndrome is a rare disease that is clinically similar to Behçet’s syndrome and is manifested with a clinical trial mainly composed of recurrent oral and genital ulcers in association with the inflamed cartilage syndrome in the form of relapsing polychondritis (with different patterns of involvement of extremities and a clinical prognosis similar to Behçet’s syndrome) (12).
Δ Hematologic disorders: Nutritional deficiencies and relevant hematologic (e.g., different types of anemia related to iron deficiency and the like) and other hematologic (e.g., neutropenia, hematologic malignancies, and the like) disorders can be important risk factors for the incidence of oral ulcers, and even oral ulcers can occasionally be the first sign of hematologic disorders (13,14). Of all the hematologic disorders, the most common ones related to aphthous-like ulcers in the oral cavity are different anemias related to nutritional deficiencies and cyclic neutropenia. Notably, cyclic neutropenia can cause aphthous-like ulcers; however, it predominately tends to create crater-like ulcers in the oral cavity (15).
Δ Cyclic neutropenia: Neutropenia, consisting of cyclic neutropenia and chronic neutropenia, is associated with decreased blood neutrophil counts. In cyclic neutropenia, neutrophil counts decrease significantly in regular periods, almost every 21 days ( < 200/µL equivalent to < 0.2×109/L) (16). The signs and clinical manifestations of cyclic neutropenia (including fatigue, recurrent fever, weakness, malaise, mucous ulcers, and the like) might be mild to severe, depending on the severity and duration of neutropenia. Of the most common oral manifestations of cyclic neutropenia are periodontitis (early tooth loss in children), gingivitis, and painful recurrent mucosal ulcers (predominantly in the form of RAS) in most areas of the tongue, buccal mucosa, and lips that heal spontaneously after the neutrophil counts improve (17). If cyclic neutropenia is on the differential diagnosis list, a chronic bullous disease (CBC)-diff test should be requested at least 2‒3 times a week for 4‒6 weeks (18).
Δ Systemic diseases: Apart from hematologic disorders, many systemic conditions can also cause aphthous-like ulcers in the oral cavity (19). In some digestive conditions, oral lesions might appear before digestive system lesions (20). Patients with a history of skin, genetic, or ocular ulcerative lesions concomitant with arthritis should be evaluated for conditions such as Behçet’s syndrome, mouth and genital ulcers with inflamed cartilage, and Reiter’s syndrome. In addition, RAS associated with recurrent fevers and infections is observed in some conditions, including periodic fever, aphthous stomatitis, pharyngitis, adenitis syndrome, cyclic neutropenia, and Sweet syndrome.
-
Systemic lupus erythematosus: In 45% of cases, it might be associated with oral manifestations such as ulcers (with no pain in most cases and mostly in the palate and oropharynx), erythema, or hyperkeratosis. Further, ulcerated areas with white diametral striae and an erythematous halo appear around the ulcers (19).
-
Inflammatory bowel diseases: This group of multifactorial diseases includes Crohn’s disease and ulcerative colitis, and during the active course of the disease, oral manifestation might appear even as the first sign of the disease before or concurrent with digestive signs, which might include recurrent oral aphthous-like ulcers (the most common), erythematous and erosive areas, cheilitis, atrophic mucositis, and fungal infections (20). To diagnose inflammatory bowel diseases, it is necessary to refer the patient to a specialist for endoscopy and colonoscopy for a definitive diagnosis, in addition to the evaluation of alimentary tract signs (e.g., weakness, fatigue, long-term diarrhea, and the like) and laboratory tests, especially Ca+2, occult blood, and occult parasites (21).
-
Celiac disease/gluten-sensitive enteropathy:It is an autoimmune disease in genetically susceptible individuals, with two groups of intestinal and extra-intestinal clinical manifestations, in which the small intestine mucosa is traumatized in response to dietary gluten and other environmental stimuli. Tooth enamel defects, delayed development, and maturation of teeth are among the oral manifestations of recurrent aphthous stomatitis, which is a disease risk indicator (22).
-
Sweet syndrome/acute febrile neutrophilic dermatosis: It is a rare disease characterized by red-brown tender nodules and plaques with cutaneous neutrophilic infiltration associated with fever, weakness, or arthralgia. Although oral involvement is unusual, oral manifestations, especially aphthous-like ulcers of the buccal mucosa or tongue, have been reported in these patients (23).
-
Diabetes mellitus: The condition is a multifactorial metabolic syndrome due to insulin deficiency (type 1 diabetes) or insulin resistance (type 2 diabetes). The presence of oral mucosal lesions, such as recurrent aphthous-like ulcers, in most diabetic patients might be directly related to their blood sugar control (24). Therefore, if diabetes is suspected based on the patient’s history and clinical symptoms and signs, laboratory tests (fasting blood sugar and hemoglobin A1C) are necessary.
-
Reiter’s syndrome: It is characterized by arthritis, nongonococcal urethritis, conjunctival involvement, and mucocutaneous lesions. Oral lesions are present in 20‒40% of cases in the form of papules and ulcers (sometimes major aphthous-like ulcers) on the buccal mucosa, gingiva, and lips. Tongue lesions are similar to geographic tongue lesions (25).
-
Human immunodeficiency virus infection: Oral lesions, including oral candidiasis, hairy leukoplakia, and aphthous ulcers, might be one of the first clinical manifestations of this infection and help reach an early diagnosis (26).
-
Coronavirus disease 19 or severe acute respiratory syndrome-coronavirus 2 infection: It is a highly transmissible viral disease with clinical symptoms and signs similar to other influenza-like viral infections (e.g., fever, dry coughs, shortness of breath, and the like). The most commonly reported signs are xerostomia, recurrent aphthous ulcers, dysphagia, and an oral burning sensation (27).
Important note: HIV, coronavirus disease 19, and Sweet syndrome are seldom associated with aphthous-like oral ulcers and are not included in the routine differential diagnosis list unless there is evidence of suspected medical history and clinical symptoms and signs.
Δ Recurrent herpetic infection (herpes simplex virus): It is a common viral infection that remains latent in the nerve ganglia for a long time after the initial infection and, if re-activated, causes recurrent infections in the two forms of recurrent herpes labialis (the most common form, also called canker sore) and initial oral HSV. The recurrent infection is usually less severe than the initial infection. Recurrent herpes labialis begins with 24-hour prodromal symptoms, including tingling, burning, and itching of the ulcer site, and then clusters of vesicles and ulcers appear at the vermilion border or the lip surface (28). Intraoral recurrent herpetic lesions of HSV in healthy individuals appear as vesicles and clusters of ulcers, respectively, (that normally coalesce with a map-like irregular view) in the keratinized mucosa of the palate and gingiva. However, in patients with immune system deficiency (HIV infection, organ transplant patients, and the like), ulcers can occur in all parts of the oral cavity (keratinized and non-keratinized gingiva) (29). Sometimes, the ulcers are solitary and less numerous and should be differentiated from aphthous ulcers. In this regard, several actions might be helpful, including attention to the location of ulcers in healthy individuals (involvement of the keratinized mucosa in recurrent HSV versus the involvement of non-keratinized mucosa in aphthous) and the number of ulcers (several cluster lesions, sometimes associated with small satellite lesions in recurrent herpes versus solitary lesions with a round or oval periphery in aphthous). In addition, individuals with immune deficiency can be questioned about the history of herpetic ulcers and the history of diseases (history of organ transplants, and the like) (2,30).
Δ Herpes zoster infection: The etiologic agent is a varicella zoster virus (VZV) that remains latent in nerve ganglia after the initial infection (chicken pox) and might become activated to cause a recurrent infection (shingles or zona). The oral manifestations are mainly in the form of vesicles and clusters of unilateral ulcers relative to the midline of the oral cavity (in the pathway of the affected nerve) on the keratinized or non-keratinized mucosa. The sensory V2 nerve is involved in most cases, affecting the gingiva and hard palate. The most important conditions on the differential diagnosis list are initial and recurrent HSV and herpetiform recurrent aphthous stomatitis. However, VZV ulcers are more widespread and painful than HSV ulcers and have a unilateral pattern. In addition, a history of chicken pox in childhood or recent contact with an infected individual helps reach a diagnosis (31). On the other hand, unlike HSV, VZV is mostly associated with severe skin involvement, and conditions only affecting the oral cavity are rare (32).
Non-recurring Ulcers
This group of ulcers is divided into two groups, namely, those with and without a history of prodromal signs.
Ulcers With a History of Prodromal Signs
-
Primary herpes infection: This self-limiting condition is mostly asymptomatic and mainly occurs in childhood. However, in symptomatic cases, it is mostly accompanied by prodromal signs, including fever, headache, malaise, nausea, vomiting, and lymphadenopathy, and affects all oral areas, from the keratinized to non-keratinized mucosa. The most common manifestations in children are gingival involvement in the form of gingivostomatitis (red hot gingiva), which leads to pain and dysphagia. Oral and lip lesions appear as painful clustered vesicles with a scalloped border on an erythematous base that convert to pustules, erosions, and ulcers (mostly coalesced and map-like and less aphthous-like), respectively, and finally resolve gradually by creating a crust (28). Therefore, posing questions about a history of prodromal signs before the appearance of oral lesions and more widespread involvement of most oral areas, especially the gingiva, can be highly helpful in reaching a diagnosis.
-
Varicella zoster infection: Initial varicella zoster infection (chicken pox) is a highly contagious disease with the highest incidence in childhood in spring and winter, which is characterized by the appearance of skin rashes (erythematous macules) that are itchy and centrotropic (mainly on the trunk and back) after a short period of prodromal symptoms (they include mild fever, malaise, and lack of appetite in children and high fever, headache, myalgia, or vomiting in adults). The skin rashes are converted to vesicles filled with a clear fluid that finally become ulcerated (mostly map-like, less frequently aphthous-like) and then become crusted. Oral lesions have a similar course and are always found along with skin lesions (33).
-
Coxsackievirus infections: These infections include three diseases of hand, foot, and mouth (HFMD), herpangina (HA), and lymphonodular pharyngitis, which mostly affect young children, with the highest incidence in late summer and early spring. In all these three conditions, first, there is a period of prodromal symptoms (fever, malaise, fatigue, and the like), followed by usual clinical symptoms and signs, including blisters and maculopapular lesions in the oral mucosa and skin (mostly on the palms and soles and the buttocks) in HFMD. Moreover, symptoms of sore throat with blisters and ulcers in the pharynx and oropharynx in HA, and nodules in the pharynx and oropharynx (instead of blisters and ulcers) in lymphonodular pharyngitis are detectable (34). In addition, a much lower rate of gingival involvement in these diseases (unlike HSV infections), the highest involvement of the posterior areas of the oral cavity and pharynx in HA, and the involvement of the palms and soles in HFMD might help discriminate them from initial HSV infections (35).
No History of Prodromal Symptoms and Signs
Trauma: Traumatic ulcers secondary to thermal, mechanical (predominantly in patients with convulsions or mental disorders, or healthy individuals, accidentally and mostly with a history of trauma such as mucosal biting, and the like) or chemical (e.g., ulcers secondary to medications such as NSAIDs, and the like) are highly common in the oral cavity and can appear in different forms, including aphthous-like (in local traumas), map-like, and even crater-like forms (36).
Map-Like Ulcers
These ulcers have irregular shapes and borders and are divided into acute and chronic subgroups. Acute ulcers are categorized into subgroups based on the presence or absence of recurrence. Chronic ulcers are classified into subgroups based on the presence or absence of keratosis in the oral mucosa.
Acute Map-Like Ulcers
Recurrent ulcers
This group is itself subdivided into two groups based on the presence or absence of constitutional symptoms (fever, weight loss, fatigue, and lymphadenopathy).
The Presence of Constitutional Symptoms
Erythema Multiforme: An acute mucocutaneous hypersensitivity is in two minor (minor EM) and severe (severe EM) forms, with characteristic target-like skin lesions. EM mostly affects young adults for different reasons, such as infectious agents (especially HSV infections), medications, and the like. In most cases, there are prodromal symptoms (e.g., fever, lymphadenopathy, malaise, and the like) before the lesions arise, and then skin lesions, with or without oral lesions, appear. Involvement of the oral cavity alone in EM is rare. First, oral lesions appear in the form of erythematous macules, mostly on the lips and the buccal mucosa, and gradually convert to blisters and then ulcers with irregular shapes with an erythematous rim (halo). The labial mucosa is covered with bleeding crusts in most cases, and depending on the disease severity, there are varying degrees of pain and discomfort (36,37). Attention to the acute nature of the disease course, the skin lesions, and mucosal lesions other than that of the oral cavity, history of patients, and questions about the presence of prodromal symptoms are highly helpful in diagnosing this condition.
Important note: Steven-Johnson syndrome and toxic epidermal necrolysis are two diseases with etiologies different from EM despise clinical and histopathological similarities to EM. The severity and extent of lesions in these two diseases are higher than in EM (38).
Absence of Constitutional Symptoms
Recurrent HSV Infection: When map-like ulcers are present without prodromal symptoms, asking questions about the history of canker sores (recurrent HSV infection) will be extremely helpful. As mentioned previously, ulcers resulting from this infection are predominantly map-like.
None-recurring Ulcers
A History of chemotherapy and radiotherapy: During the chemotherapy (CT), radiotherapy (RT), and hematologic stem cell transplant procedures to destroy malignant cells when treating tumors, cancers, and hematologic disorders, usually the oral mucosa is also affected due to its high mitotic activity, causing many complications in the oral cavity. Oral mucositis (mostly in the form of irregular coalesced, map-like ulcers) is one of the common complications of CT and RT, with severe pain, severely debilitating the patient and increasing the susceptibility to hemorrhage and secondary infections (14). Generally, RT and CT can mainly cause acute map-like ulcers and less chronic ulcers (39-41). Therefore, asking questions about a history of cancer, hematologic disorders, or hospitalization for CT or RT is one of the essential questions in evaluating the history of patients with map-like ulcers.
Important note: The presence of several ulcers, gingival hyperplasia, petechiae, and ecchymosis on the oral mucosa and spontaneous gingival bleeding without a local etiologic factor, and frequent infections might be signs of leukemia (14).
-
Initial herpetic infection: As explained previously, most ulcers of the initial HSV infection are associated with the aggregation and coalescing of map-like ulcers with scalloped borders (28).
-
Trauma; Ulcers resulting from chemical burns: Oral traumatic injuries can appear in any form.
-
Allergy: Oral mucosal hypersensitivity reactions or oral mucosal allergy are primarily related to different products (e.g., food, drink, orodental hygiene products, dental materials, and the like) and appear in different forms, including ulcers (mostly map-like), lichenoid reactions, lip swelling, and the like (36). In addition, the appearance of erythematous macular areas with the highest involvement of the gingiva is observed several days after contacting the stimulus (e.g., chewing gum and the like), and crustation of the epithelium is sometimes detected in association with ulcers in plasma cell stomatitis (42). Taking a precise history in the face of different oral lesions, especially acute map-like ulcers, is highly important to reach a correct diagnosis.
Chronic Map-Like Ulcers
They are divided into two groups based on the presence or absence of keratosis around the ulcer or other oral mucosal areas.
The Presence of Keratosis (Around the Ulcer or Other Oral Mucosal areas)
-
Oral Lichen planus: Lichen planus is a relatively common, chronic, mucocutaneous, immunologic disease that mainly affects middle-aged adults (30–60 years) with a female predilection. The oral cavity mucosa is the most commonly affected mucosa and can be found alone or in association with skin involvement characterized by 5 Ps (i.e., purple, polygonal, pruritic, papules, and plaques) and other mucosal membranes of the body. The oral manifestations of this condition consist of six clinical views, including reticular (the most common form, with white, keratotic, reticular lines, called the Wickham striae), popular (white keratotic papules), plaque-like, atrophic/erosive, ulcerative, and bullous. The most commonly affected area is the buccal mucosa (mostly bilaterally), followed by the tongue, gingiva, palate, and the vermillion border of the lip. The presence of white keratotic components in all six clinical forms of Oral lichen planus (OLP) is one of the diagnostic criteria (36).
-
Lichenoid reactions (Lichenoid contact reaction, drug-induced lichenoid reaction, and graft versus host disease): The clinical and histopathological characteristics of these conditions are similar to those of OLP. However, they have a different etiopathogenesis. Their clinical manifestations might appear in each of the six clinical views of OLP. In all these cases, if ulcers are formed, they are map-like, along with white keratotic areas. However, unlike OLP, which has an unknown etiology, lichenoid contact reaction (LCR) appears in response to dental materials (mostly amalgam restorations and metallic materials). Drug-induced liver injury (DILR) is a reaction to medications and foreign agents such as flavoring agents, and GvHD is a reaction to hematopoietic cell transplantation. In addition, OLP lesions are usually symmetrical, bilateral, and multiple, while LCP lesions tend to be unilateral and localized. On the other hand, GvHD lesions are more widespread (mostly on the palate) and mostly associated with cutaneous, digestive, and similar signs and symptoms, though oral lichenoid reactions might be the first sign of chronic GvHD. A history of a disease leading to hematocrit (e.g., leukemia) might be helpful in such cases. Further, in DILR, the extent of the lesions is more limited than that of OLP, and usually, uncommon sites for OLP involvement (e.g., the palate) become involved, and a history of medications is also essential (43).
-
ΔSystemic lupus erythematosus: As mentioned previously, oral lesions of SLE mostly appear as centric ulcers (usually aphthous-like and sometimes map-like) with white radiant striae and an erythematous halo around ulcers.
* Absence of keratosis: These ulcers are divided into two groups based on the presence or absence of skin insolvent.
The Presence of Skin Involvement
-
Pemphigus vulgaris (PV): It is an autoimmune, vesiculobullous, mucocutaneous condition that mostly affects adults (in the fourth to sixth decades of life). Oral involvement occurs in 80–90% of the patients, as the first disease sign in over 50% of cases. In the clinical view of oral lesions, most blisters (with a non-inflamed base) rapidly burst due to mechanical traumas resulting from mastication and are found as erosions and irregular, extensive surface ulcers and erosions (map-like) in association with tissue tags. These ulcers are painful and have a widespread and progressive nature in most oral areas, especially in the buccal mucosa and pharyngeal areas, resulting in dysphagia and progressive debility in the patient. Secondary infection of oral ulcers might mask the usual characteristics of PV ulcers. Therefore, biopsies and histopathological evaluations of the samples (and preferably direct immunofluorescence and differential item functioning tests) are necessary for the definitive diagnosis of PV (36,44).
-
Linear immunoglobulin a disease/chronic bullous disease of childhood (LAD/CBCDC): LAD is a rare autoimmune subepithelial vesiculobullous disease with a linear precipitation of IgA along the basement membrane, primarily affecting adults (in the sixth and seventh decades of life) with a female predilection. It is known as the CBCDC in children or herpetiform dermatitis in adolescents (36). The skin involvement in this disease appears as sudden itchy blisters with a “jewel cluster” (41,45). Oral involvement in LAD has been reported in 5%–70% of cases in the form of painful vesicles, erosions, or ulcers (especially the involvement of hard and soft palates and gingival involvement in the form of desquamative gingivitis). A definitive diagnosis can be reached through biopsies and direct immunofluorescence (DIF) evaluations (36,46).
-
Epidermolysis bullosa: EB is a diverse group of hereditary cutaneous disorders, with four simplex, junctional, dystrophic, and Kindler (47) forms. Oral manifestations have different forms and severities, depending on the disease phenotype, and angular cheilitis and oral ulcers/blisters are observed in most patients (48). In these patients, the complications after recurrent blisters include decreased growth of the maxilla and mandible, disorders in lip and tongue movements, limited mouth opening (microstomia), and the like, depending on the severity of scar formation (49,50).
-
Acquired epidermolysis bullosa: It is a rare, acquired, autoimmune vesiculobullous disorder (51). The most common clinical forms of this disorder are the classical/mechanical (non-inflammatory blisters and erosions/scars are areas susceptible to trauma) and non-classical/inflammatory (inflammatory blisters, skin rashes with erythemas similar to other vesiculobullous lesions such as BP) ones. In addition, these patients suffer from cutaneous and mucous blisters and scars. Some of the oral manifestations of EBA include erythematous gingiva and oral ulcers. A definitive diagnosis is reached based on clinical manifestations, biopsies, and DIF evaluations (51-53).
-
Bullous pemphigoid: BP is the most common autoimmune blister-forming condition with tense blisters, which are mostly itchy and erythematous (predominantly on the skin of the trunk and extremities), with or without mucous membrane involvement, affecting individuals 60–80 years of age (54). The manifestations of BP are mostly cutaneous, and oral mucous membrane involvement is less common (10–20%) and less severe than MMP. Moreover, these manifestations appear predominantly as blisters, erosions, and irregular map-like ulcers with an inflammatory base. They do not lead to scar formation, contrary to MMP (55,56). Desquamative gingivitis is one of the most common oral manifestations of BP (56). The diagnosis of BP is based on clinical examinations, biopsies, and laboratory tests, including DIF and indirect immunofluorescence (55).
-
Herpetiform dermatitis: DH, or Duhring disease, is a rare condition due to an allergy to gluten, with the hallmark feature of the asymmetrical distribution of blistering rashes that are highly itchy and appear on extensor surfaces such as the elbow and the dorsal aspect of the forearm. Oral involvement is rare and might be visible as vesicles/ulcers, macules, and erosions throughout the oral mucosa. Diagnosis mainly relies on clinical and serologic (antibodies against TG3 and TG2 [epidermal transglutominase]) and histopathological evaluations, especially DIF, as the gold standard for the diagnosis of DH (57).
No Cutaneous Involvement
Mucous membrane pemphigoid: MMP, or cicatricial pemphigoid, is a rare autoimmune subepithelial vesiculobullous disorder primarily affecting the oral and ocular mucosa, with a predilection for middle-aged and old individuals. Scar formation after the healing of conjunctival lesions might lead to blindness. In most patients, the oral mucosa is the site for the onset and the most common site of involvement (85%), with predominantly clinical manifestations of desquamative gingivitis in the gingiva. Other oral lesions appear as erythematous macules, blisters, or erosions/ulcers (map-like ulcers with an inflammatory base) in different areas of the oral cavity that cannot be distinguished from other blistering disease ulcers, such as PV, concerning their appearance. The disease severity in MMP is lower than that of PV, and the involvement of the conjunctiva (eye redness and the like) might help initially distinguish it from PV. On the other hand, unlike BP, MMP mainly affects the mucosa, and the skin is rarely affected. Unlike MMP, which is a gradually progressive condition, BP is mostly self-limiting and less severe. The diagnosis of MMP is based on clinical, histological, and immunopathological findings (58).
-
History of Chemotherapy and Radiotherapy: As discussed earlier, RT and CT can cause acute or chronic map-like ulcers in the oral cavity.
-
Trauma: In addition to creating different forms of ulcers, trauma can cause acute or chronic ulcers (36). Therefore, posing questions about the history of trauma is highly important in all ulcer types.
Crater-Like Ulcers
These ulcers are in the form of volcanic craters (with a depressed center and elevated borders) and are divided into acute and chronic ulcer groups. Each group is also classified based on the absence or presence of respiratory signs and pulmonary involvement.
Acute Ulcers
With Pulmonary Involvement and Respiratory Symptoms and Signs
-
Tuberculosis infection
-
Deep fungal infections
Without Pulmonary Involvement and Respiratory Symptoms and Signs
-
Trauma/eosinophilic ulcer of the tongue (ulcerated granuloma of the tongue, oral traumatic granuloma, or traumatic ulceration): We previously discussed different forms of traumatic injuries. The eosinophilic ulcer of the tongue is a self-limiting reactive lesion with unknown pathogenesis. It primarily affects the lateral borders of the tongue; however, it can affect the gingiva and other mucosal surfaces of the oral cavity. This crater-like ulcer appears as an acute or mostly chronic ulcer with a punched-out form with sharp borders that are usually elevated and are sometimes associated with a history of trauma. This ulcer appears in young children during primary tooth eruption, especially on the ventral aspect of the tongue (due to dental traumas), and is called Riga-Fede disease (7,59,60). In cases where malignancies are on the differential diagnosis list (e.g., squamous cell carcinoma), a biopsy of the ulcer is recommended for the initial diagnosis of this lesion (59).
-
Necrotising sialometaplasia: It is a benign inflammatory disorder of the salivary glands that mainly affects the hard palate. However, it might affect any oral area with a salivary gland. NS usually influences males, mostly in the fourth decade of life (61). The ischemia of the vessels perfusing salivary glands is the best-known factor leading to NS, which occurs due to several possible factors, including local trauma (resulting from blunt forces), infiltration of dental anesthetic agents, and the like. In clinical examinations, NS is characterized by a deep acute or chronic crater-like ulcer with varying sizes and clearly visible borders, mostly surrounded by an erythematous halo (61). Diagnosis is mainly based on clinical characteristics, history (especially a history of dental injection), and histopathological evaluation. This lesion is self-limiting (with a recovery period of 6–8 weeks) and does not require any specific treatment. However, due to clinical similarity to squamous-cell carcinoma (SCC) and mucoepidermoid carcinoma, when these ulcers are present, biopsy and histopathological evaluations of the lesions are necessary to reach a correct diagnosis (62).
-
Chronic/cyclic neutropenia: This systemic hematologic disorder is characterized by periodic decreases in the absolute counts of neutrophils, with oral ulcers, fever, lymphadenopathy, and severe infections. It might also be associated with thrombocytopenia and anemia. In more severe forms of chronic neutropenia, oral manifestations might appear, including painful and hemorrhagic crater-like ulcers in the oral mucosa and gingivitis in the form of painful, hemorrhagic, erosive lesions. Secondary infections and periodontitis are also common in these patients (15). As mentioned previously, cyclic neutropenia ulcers are predominantly in the form of aphthous-like ulcers; however, the ulcers of chronic neutropenia are mostly crater-like.
-
Major aphthous or Sutton’s disease or periadenitis mucosa necrotica recurrens: It is the uncommon form of aphthous ulcers, with a predilection for females, which appears clinically in the form of deep crater-like ulcers, mostly round and sometimes irregular, with slightly elevated borders and an erythematous halo, measuring > 10 mm (predominantly on the lips, tongue, and the soft palate), which might sustain several weeks or months. The ulcers are highly painful, heal with scar formation, and might sometimes be associated with fever, dysphagia, and malaise. Patients with HIV exhibit the most severe major aphthous ulcers (6). The diagnosis of RAS is based on history and clinical examinations. However, when the ulcers first appear, especially during adulthood, or are extremely severe with high frequency, it is necessary to evaluate the systemic background etiologic factors and rule them out (63).
Chronic Ulcers
With Pulmonary Involvement and Respiratory Symptoms and Signs
-
Tuberculosis: TB is a chronic multi-system infection, with Mycobacterium tuberculosis as the most important etiologic agent. Oral lesions are rare in TB and might be initial or secondary (more common) to pulmonary tuberculosis. Acute crater-like ulcers, or mainly chronic ulcers, are the most common oral lesions of tuberculosis. These ulcers are mostly irregular and deep with indurated, undermined, and slightly raised periphery, which are covered with a yellow granular layer, and predominantly insensitive (in primary tuberculosis, which is uncommon and mostly in children) or painful (in secondary tuberculosis, and mostly in middle-aged and older adults, in association with pulmonary tuberculosis). Unlike oral involvement in primary tuberculosis, which mostly occurs in children and predominantly on the gingiva in the form of nodular or papillary lesions, the most common site for oral involvement in secondary tuberculosis is the tongue in the form of chronic, persistent ulcers. Attention to patient history and the presence of pulmonary involvement and respiratory symptoms and signs, clinical findings, and, if necessary, proper tests and chest x-rays are extremely helpful (46).
-
Deep fungal infections: These infections cause severe complications and significant mortality, mainly in individuals with immune deficiency, and can cause oral ulcers as well (64). Aspergillosis ulcers appear as dark or yellow necrotic lesions, mainly on the palate or posterior tongue (65). Diffuse blastomycosis, in addition to pulmonary involvement, might produce oral lesions characterized by irregular crater-like ulcers with indurated, raised borders, which are mostly painless (e.g., SCC) in all areas of the oral cavity (3,65). Histoplasmosis creates oral ulcers that are usually painful and persistent and have indurated round borders, mostly on the tongue, gingiva, or palate, with cutaneous and pulmonary involvement in most cases. These ulcers begin in the form of erythema and are then converted to papules, and finally ulcerate with a granulomatous appearance (3,66). Cryptococcosis is an invasive fungal infection and has an important role in the oral infections of patients with immune deficiency; however, it can also affect healthy individuals. Its oral ulcers might have indurated borders such as SCC, mostly on the palate, gingiva, or tonsillar pillars (3,67). The rare infection of coccidioidomycosis might also cause oral ulcers. The mucocutaneous form of paracoccidioidomycosis might initiate as small vesicles with raised borders that become painful over time (3). Invasive, acute mucormycosis infections mostly affect individuals with immune deficiency and diabetic individuals with poor control. Oral mucormycosis normally affects the paranasal sinuses or nasal areas. In intraoral involvement, it usually leads to necrosis and ulceration of the palate (65).
Without Pulmonary Involvement and Pulmonary Symptoms and Signs
-
Trauma/eosinophilic ulcers
-
Necrotizing sialometaplasia
-
Syphilis: It is a highly transmissible bacterial infection caused by the spirochete Treponema pallidum and has initial, secondary, latent, and tertiary stages. The oral cavity is the most common extra-genital location of involvement. Chancre is the first sign of initial syphilis, as a small, painless papule associated with insensitive lymphadenopathy, finally leading to a deep ulcer (mostly crater-like) with a violet, red, or brown base and raised borders, which heals spontaneously (67). Two main characteristics of secondary syphilis are the appearance of mucous patches and maculopapular lesions, especially in hand palms and foot soles, which are mostly associated with a wide range of systemic symptoms such as fever, myalgia, and the like. In addition, oral ulcers (mostly in the form of map-like ulcers) might rarely become one of the main manifestations of this stage. The other oral manifestations of this stage include keratosis, plaque, or condyloma lata (67,68). Gumma is one of the oral manifestations of tertiary syphilis that first appears as a painless swelling, mainly in the hard palate and tongue, and finally creates an ulcer, which is mostly create-like (68). The diagnosis of syphilis mostly relies on taking a precise history (including high-risk behaviors), clinical examinations, serologic tests (e.g., a venereal disease research laboratory test), and, sometimes, histopathological examinations. The duration of ulcers, the recurrence pattern, clinical view, the location of the lesion, the presence and absence of systemic symptoms and signs, and history in particular, are helpful in correctly diagnosing the etiologic agent for ulcers in this disease (67).
Important note: The most common lesions of the Epstein-Barr virus include infectious mononucleosis, nasopharyngeal carcinoma, and Burkitt lymphoma. Ulcers due to the Epstein-Barr virus are rare but might be one of the characteristics of infectious mononucleosis. In the oral mucosa, ulcers are typically small and shallow (1).
The algorithm in Figure 1 illustrates the classification of oral ulcers based on clinical shapes (Figure 1).
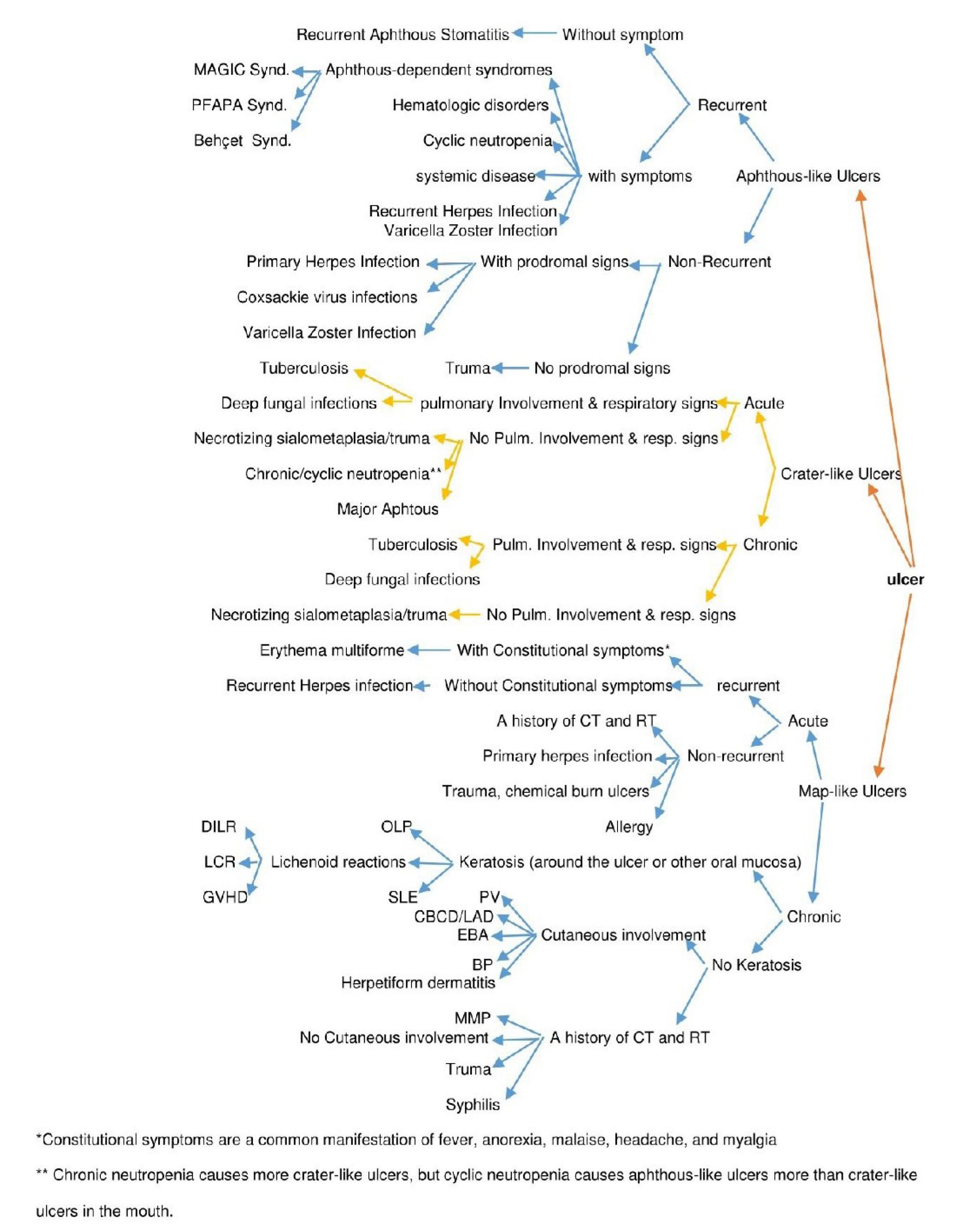
Figure 1.
The Algorithm of oral ulcers classification based on clinical shapes.
.
The Algorithm of oral ulcers classification based on clinical shapes.
Conclusion
Due to the wide array of etiologic agents for oral ulcers, pinpointing the etiologic agent can be highly challenging. In the present study, in addition to briefly reviewing the common clinical manifestations of oral ulcers, we proposed a proper and comprehensive diagnostic guide through a simple algorithm to facilitate the classification and diagnosis of different oral ulcers.
Authors’ Contribution
Conceptualization: Fatemeh Ahmadi-Motamayel
Data curation: Parya Atapour, Deniz Safabakhsh
Investigation: Fereshteh Najar-Karimi
Methodology: Deniz Safabakhsh, Fatemeh Abbasi
Project administration: Laleh Shahabi
Supervision: Fatemeh Ahmadi-Motamayel
Validation: Laleh Shahabi, Parya Atapour
Visualization: Fatemeh Abbasi
Writing–original draft: Fereshteh Najar-Karimi.
Writing–review & editing: Fatemeh Ahmadi-Motamayel, Fereshteh Najar-Karimi, Deniz Safabakhsh, Fatemeh Abbasi, Parya Atapour, Laleh Shahabi.
Competing Interests
The authors declare that they have no conflict of interests.
Ethical Approval
Not applicable.
Funding
No external funding was available for this study.
References
- Minhas S, Sajjad A, Kashif M, Taj F, Waddani HA, Khurshid Z. Oral ulcers presentation in systemic diseases: an update. Open Access Maced J Med Sci 2019; 7(19):3341-7. doi: 10.3889/oamjms.2019.689 [Crossref] [ Google Scholar]
- Glick M, Greenberg MS, Lockhart PB, Challacombe SJ. Introduction to oral medicine and oral diagnosis: patient evaluation. In: Burket’s Oral Medicine. John Wiley & Sons; 2021. p. 1-18.
- Fitzpatrick SG, Cohen DM, Clark AN. Ulcerated lesions of the oral mucosa: clinical and histologic review. Head Neck Pathol 2019; 13(1):91-102. doi: 10.1007/s12105-018-0981-8 [Crossref] [ Google Scholar]
- Lehman JS, Rogers RS 3rd. Acute oral ulcers. Clin Dermatol 2016; 34(4):470-4. doi: 10.1016/j.clindermatol.2016.02.019 [Crossref] [ Google Scholar]
- Siu A, Landon K, Ramos DM. Differential diagnosis and management of oral ulcers. Semin Cutan Med Surg 2015; 34(4):171-7. doi: 10.12788/j.sder.2015.0170 [Crossref] [ Google Scholar]
- Kadir A, Islam A, Ruhan M, Mowla A, Nipun JN. Recurrent aphthous stomatitis: an overview. Int J Oral Health Dent 2018; 4(1):6-11. doi: 10.18231/2395-499x.2018.0002 [Crossref] [ Google Scholar]
- Légeret C, Furlano R. Oral ulcers in children- a clinical narrative overview. Ital J Pediatr 2021; 47(1):144. doi: 10.1186/s13052-021-01097-2 [Crossref] [ Google Scholar]
- Ambrose NL, Haskard DO. Differential diagnosis and management of Behçet syndrome. Nat Rev Rheumatol 2013; 9(2):79-89. doi: 10.1038/nrrheum.2012.156 [Crossref] [ Google Scholar]
- Bulur I, Onder M. Behçet disease: new aspects. Clin Dermatol 2017; 35(5):421-34. doi: 10.1016/j.clindermatol.2017.06.004 [Crossref] [ Google Scholar]
- Soriano A, Soriano M, Espinosa G, Manna R, Emmi G, Cantarini L. Current therapeutic options for the main monogenic autoinflammatory diseases and PFAPA syndrome: evidence-based approach and proposal of a practical guide. Front Immunol 2020; 11:865. doi: 10.3389/fimmu.2020.00865 [Crossref] [ Google Scholar]
- Wang A, Manthiram K, Dedeoglu F, Licameli GR. Periodic fever, aphthous stomatitis, pharyngitis, and adenitis (PFAPA) syndrome: a review. World J Otorhinolaryngol Head Neck Surg 2021; 7(3):166-73. doi: 10.1016/j.wjorl.2021.05.004 [Crossref] [ Google Scholar]
- Luo Y, Bolek EC, Quinn KA, Wells K, Rose E, Sikora K. A prospective observational cohort study and systematic review of 40 patients with mouth and genital ulcers with inflamed cartilage (MAGIC) syndrome. Semin Arthritis Rheum 2022; 52:151924. doi: 10.1016/j.semarthrit.2021.10.007 [Crossref] [ Google Scholar]
- Chen H, Sui Q, Chen Y, Ge L, Lin M. Impact of haematologic deficiencies on recurrent aphthous ulceration: a meta-analysis. Br Dent J 2015; 218(4):E8. doi: 10.1038/sj.bdj.2015.100 [Crossref] [ Google Scholar]
- Gomes AO, Silva Junior A, Noce CW, Ferreira M, Maiolino A, Torres SR. The frequency of oral conditions detected in hematology inpatients. Hematol Transfus Cell Ther 2018; 40(3):240-4. doi: 10.1016/j.htct.2018.02.006 [Crossref] [ Google Scholar]
- Farina GA, Perotto ST, Munerato MC. Oral manifestations in chronic neutropenia in adults: a case report. Oral Health Care 2018; 3(2):1-4. doi: 10.15761/ohc.1000142 [Crossref] [ Google Scholar]
- Zergham AS, Acharya U. Cyclic Neutropenia. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022.
- Sankar V, Villa A. Hematologic diseases. In: Burket’s Oral Medicine. John Wiley & Sons; 2021. p. 627-64.
- Solomou EE, Salamaliki C, Lagadinou M. How to make the right diagnosis in neutropenia. Clin Hematol Int 2021; 3(2):41-6. doi: 10.2991/chi.k.210216.001 [Crossref] [ Google Scholar]
- Capodiferro S, Limongelli L, Favia G. Oral and maxillo-facial manifestations of systemic diseases: an overview. Medicina (Kaunas) 2021; 57(3):271. doi: 10.3390/medicina57030271 [Crossref] [ Google Scholar]
- Klichowska-Palonka M, Komsta A, Pac-Kożuchowska E. The condition of the oral cavity at the time of diagnosis of inflammatory bowel disease in pediatric patients. Sci Rep 2021; 11(1):21898. doi: 10.1038/s41598-021-01370-8 [Crossref] [ Google Scholar]
- Seyedian SS, Nokhostin F, Dargahi Malamir M. A review of the diagnosis, prevention, and treatment methods of inflammatory bowel disease. J Med Life 2019; 12(2):113-22. doi: 10.25122/jml-2018-0075 [Crossref] [ Google Scholar]
- Alsadat FA, Alamoudi NM, El-Housseiny AA, Felemban OM, Dardeer FM, Saadah OI. Oral and dental manifestations of celiac disease in children: a case-control study. BMC Oral Health 2021; 21(1):669. doi: 10.1186/s12903-021-01976-4 [Crossref] [ Google Scholar]
- Cohen PR. Sweet’s syndrome--a comprehensive review of an acute febrile neutrophilic dermatosis. Orphanet J Rare Dis 2007; 2:34. doi: 10.1186/1750-1172-2-34 [Crossref] [ Google Scholar]
- Silva MF, Barbosa KG, Pereira JV, Bento PM, Godoy GP, de Castro Gomes DQ. Prevalence of oral mucosal lesions among patients with diabetes mellitus types 1 and 2. An Bras Dermatol 2015; 90(1):49-53. doi: 10.1590/abd1806-4841.20153089 [Crossref] [ Google Scholar]
- Keogan MT. Clinical Immunology Review Series: an approach to the patient with recurrent orogenital ulceration, including Behçet’s syndrome. Clin Exp Immunol 2009; 156(1):1-11. doi: 10.1111/j.1365-2249.2008.03857.x [Crossref] [ Google Scholar]
- Pakfetrat A, Falaki F, Delavarian Z, Dalirsani Z, Sanatkhani M, Zabihi Marani M. Oral manifestations of human immunodeficiency virus-infected patients. Iran J Otorhinolaryngol 2015; 27(78):43-54. [ Google Scholar]
- Muthyam AK, Reddy MP, Kulkarni S, Srilatha A, Sahithi K, Satyanarayana D. Oral manifestations in COVID-19 patients: an observational study. J Family Med Prim Care 2022; 11(3):1000-5. doi: 10.4103/jfmpc.jfmpc_1264_21 [Crossref] [ Google Scholar]
- Saleh D, Yarrarapu SN, Sharma S. Herpes simplex type 1. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2021.
- Santosh ABR, Muddana K. Viral infections of oral cavity. J Family Med Prim Care 2020; 9(1):36-42. doi: 10.4103/jfmpc.jfmpc_807_19 [Crossref] [ Google Scholar]
- Chiang YT, Hwang MJ, Lee YP, Chiang CP. Differential diagnosis between herpetic gingivostomatitis and herpetiform aphthous ulcerations. J Dent Sci 2020; 15(3):386-7. doi: 10.1016/j.jds.2020.06.001 [Crossref] [ Google Scholar]
- Tsai YC, Lee YP, Hwang MJ, Chiang CP. Oral herpes zoster - case report. J Dent Sci 2021; 16(1):563-4. doi: 10.1016/j.jds.2020.10.001 [Crossref] [ Google Scholar]
- Iwanaga J, Fukuoka H, Fukuoka N, Yutori H, Ibaragi S, Tubbs RS. A narrative review and clinical anatomy of herpes zoster infection following COVID-19 vaccination. Clin Anat 2022; 35(1):45-51. doi: 10.1002/ca.23790 [Crossref] [ Google Scholar]
- Bansod NV, Chopkar SH, Shinde P, Waghmare R. Overview of chickenpox in children. Int Res J Mod Eng Technol Sci 2021; 3(2):222-3. [ Google Scholar]
- Andrés C, Guasch E, Piñana M, Fernandes P, Gimferrer L, Esso DV. Recombinant CV-A6 strains related to hand-foot-mouth disease and herpangina at primary care centers (Barcelona, Spain). Future Microbiol 2019; 14:499-507. doi: 10.2217/fmb-2018-0336 [Crossref] [ Google Scholar]
- Dhalech AH, Fuller TD, Robinson CM. Specific bacterial cell wall components influence the stability of coxsackievirus B3. J Virol 2021; 95(22):e0142421. doi: 10.1128/jvi.01424-21 [Crossref] [ Google Scholar]
- Mortazavi H, Safi Y, Baharvand M, Rahmani S. Diagnostic features of common oral ulcerative lesions: an updated decision tree. Int J Dent 2016; 2016:7278925. doi: 10.1155/2016/7278925 [Crossref] [ Google Scholar]
- Dalipi ZS, Dragidella F, Dragidella DK. Oral manifestations of exudative erythema multiforme in a patient with COVID-19. Case Rep Dent 2021; 2021:1148945. doi: 10.1155/2021/1148945 [Crossref] [ Google Scholar]
- Newkirk RE, Fomin DA, Braden MM. Erythema multiforme versus Stevens-Johnson syndrome/toxic epidermal necrolysis: subtle difference in presentation, major difference in management. Mil Med 2020; 185(9-10):e1847-50. doi: 10.1093/milmed/usaa029 [Crossref] [ Google Scholar]
- Elad S, Zadik Y. Chronic oral mucositis after radiotherapy to the head and neck: a new insight. Support Care Cancer 2016; 24(11):4825-30. doi: 10.1007/s00520-016-3337-5 [Crossref] [ Google Scholar]
- Lalla RV, Brennan MT, Gordon SM, Sonis ST, Rosenthal DI, Keefe DM. Oral mucositis due to high-dose chemotherapy and/or head and neck radiation therapy. J Natl Cancer Inst Monogr 2019; 2019(53):lgz011. doi: 10.1093/jncimonographs/lgz011 [Crossref] [ Google Scholar]
- Kothiwala S, Vashisht KR. Oral mucosa. In: Atlas of Clinical Dermatology in Coloured Skin. CRC Press; 2023. p. 365-402.
- Navya MK, Sujatha GP, Lingappa A. Acute multiple ulcers involving oral mucosa. J Pearldent 2017; 8(2):33-7. doi: 10.5958/2229-4457.2017.00009.5 [Crossref] [ Google Scholar]
- Agha-Hosseini F, Samami M, Tavakol F, Ghasemzadeh Hoseini E. Oral lichen planus or oral lichenoid reaction? A literature review. J Iran Dent Assoc 2019; 31(1):40-57. doi: 10.30699/jidai.31.1.7 [Crossref] [ Google Scholar]
- Batistella E, Sabino da Silva R, Rivero ER, Silva CA. Prevalence of oral mucosal lesions in patients with pemphigus vulgaris: a systematic review and meta-analysis. J Oral Pathol Med 2021; 50(8):750-7. doi: 10.1111/jop.13167 [Crossref] [ Google Scholar]
- Khare S. Unusual oral manifestations of autoimmune disorders. J Orofac Res 2023; 12(2):13-21. [ Google Scholar]
- Patra PC, Choudhury P, Hasan S, Saeed S. Orofacial tuberculosis: an uncommon manifestation of a common disease-a narrative review. Indian J Forensic Med Toxicol 2021; 15(1):1806-18. [ Google Scholar]
- Has C, Bauer JW, Bodemer C, Bolling MC, Bruckner-Tuderman L, Diem A. Consensus reclassification of inherited epidermolysis bullosa and other disorders with skin fragility. Br J Dermatol 2020; 183(4):614-27. doi: 10.1111/bjd.18921 [Crossref] [ Google Scholar]
- Fine JD, Eady RA, Bauer EA, Bauer JW, Bruckner-Tuderman L, Heagerty A. The classification of inherited epidermolysis bullosa (EB): report of the Third International Consensus Meeting on Diagnosis and Classification of EB. J Am Acad Dermatol 2008; 58(6):931-50. doi: 10.1016/j.jaad.2008.02.004 [Crossref] [ Google Scholar]
- Wright JT. Oral manifestations in the epidermolysis bullosa spectrum. Dermatol Clin 2010; 28(1):159-64. doi: 10.1016/j.det.2009.10.022 [Crossref] [ Google Scholar]
- de Azevedo BL, Roni GM, Dettogni RS, Torrelio RM, Leal LF, da Gama-de-Souza LN. Epidermolysis bullosa in oral health: clinical manifestations and salivary alterations. Clin Oral Investig 2023; 27(6):3117-24. doi: 10.1007/s00784-023-04917-3 [Crossref] [ Google Scholar]
- Hignett E, Sami N. Pediatric epidermolysis bullosa acquisita: a review. Pediatr Dermatol 2021; 38(5):1047-50. doi: 10.1111/pde.14722 [Crossref] [ Google Scholar]
- Kridin K, Kneiber D, Kowalski EH, Valdebran M, Amber KT. Epidermolysis bullosa acquisita: a comprehensive review. Autoimmun Rev 2019; 18(8):786-95. doi: 10.1016/j.autrev.2019.06.007 [Crossref] [ Google Scholar]
- Mulder Yan Staden S, Negi M, Holmes H, Jeftha A. Oral Medicine Case Book: epidermolysis bullosa acquisita. SADJ 2018;73(4):249-52. 10.10520/EJC-100b19b86b.
- Ramcke T, Vicari E, Bolduan V, Enk A, Hadaschik E. Bullous pemphigoid (BP) patients with selective IgG autoreactivity against BP230: review of a rare but valuable cohort with impact on the comprehension of the pathogenesis of BP. J Dermatol Sci 2022; 105(2):72-9. doi: 10.1016/j.jdermsci.2021.11.011 [Crossref] [ Google Scholar]
- Chen X, Zhao W, Jin H, Li L. Risk factors for mucosal involvement in bullous pemphigoid and the possible mechanism: a review. Front Med (Lausanne) 2021; 8:680871. doi: 10.3389/fmed.2021.680871 [Crossref] [ Google Scholar]
- Manek S, Saravanan SP, Rahul R. Bullous pemphigoid a rare autoimmune disease: a case report. Int J Dent Sci Res 2022; 10(1):1-3. doi: 10.12691/ijdsr-10-1-1 [Crossref] [ Google Scholar]
- Nguyen CN, Kim SJ. Dermatitis herpetiformis: an update on diagnosis, disease monitoring, and management. Medicina (Kaunas) 2021; 57(8):843. doi: 10.3390/medicina57080843 [Crossref] [ Google Scholar]
- Carey B, Setterfield J. Mucous membrane pemphigoid and oral blistering diseases. Clin Exp Dermatol 2019; 44(7):732-9. doi: 10.1111/ced.13996 [Crossref] [ Google Scholar]
- Hamie L, Hamie M, Kurban M, Abbas O. Eosinophilic ulcer of the oral mucosa: an update on clinicopathologic features, pathogenesis, and management. Int J Dermatol 2022; 61(11):1359-63. doi: 10.1111/ijd.15986 [Crossref] [ Google Scholar]
- Khandelwal J, Bargale S, Dave B, Dharmatti S. Novel management of Riga-Fede disease associated with early infancy tooth in 4-month-old infant. Int J Med Dent Case Rep 2021; 12(5):1-3. doi: 10.15713/ins.ijmdcr.171 [Crossref] [ Google Scholar]
- Gupta A, Priyadarshinee A, Rao LN, Redhu A, Jha KS. Necrotizing sialometaplasia-a self-limiting condition which poses a diagnostic dilemma. Clin Case Rep 2021; 9(4):2019-22. doi: 10.1002/ccr3.3931 [Crossref] [ Google Scholar]
- Joshi SA, Halli R, Koranne V, Singh S. Necrotizing sialometaplasia: a diagnostic dilemma!. J Oral Maxillofac Pathol 2014; 18(3):420-2. doi: 10.4103/0973-029x.151336 [Crossref] [ Google Scholar]
- Sánchez-Bernal J, Conejero C, Conejero R. Recurrent aphthous stomatitis. Actas Dermosifiliogr (Engl Ed) 2020; 111(6):471-80. doi: 10.1016/j.ad.2019.09.004 [Crossref] [ Google Scholar]
- Kwizera R, Bongomin F, Lukande R. Deep fungal infections diagnosed by histology in Uganda: a 70-year retrospective study. Med Mycol 2020; 58(8):1044-52. doi: 10.1093/mmy/myaa018 [Crossref] [ Google Scholar]
- Rajendra Santosh AB, Muddana K, Bakki SR. Fungal
infections of oral cavity: diagnosis, management, and association with COVID-19. SN Compr Clin Med 2021; 3(6):1373-84. doi: 10.1007/s42399-021-00873-9 [Crossref] [ Google Scholar]
- Durkin MJ, Seoudi N, Nair R. Infectious diseases. In:
Burket’s Oral Medicine. John Wiley & Sons; 2021. p. 785-816.
- Deng F, Thompson LDR, Lai J. Unexpected reason for non-healing oral ulcers: syphilis. Head Neck Pathol 2022; 16(2):544-9. doi: 10.1007/s12105-021-01348-y [Crossref] [ Google Scholar]
- Hariharan R, Babu NA, Masthan K, Anitha N. Oral
manifestations of syphilis-a review. Eur J Mol Clin Med 2020; 7(10):815-9. [ Google Scholar]