Avicenna J Dent Res. 15(2):42-46.
doi: 10.34172/ajdr.2023.1657
Original Article
Amount of Residual Cement at the Margin of Implant-Supported Crowns Cemented Using the Polytetrafluoroethylene Tape, Replica Technique, and Conventional Cementation Technique
Fareiborz Vafaee 1  , Zahra Bagheri 1, *
, Zahra Bagheri 1, *  , Saeed Nikanjam 1, Fahimeh Daneshyar 2
, Saeed Nikanjam 1, Fahimeh Daneshyar 2  , Behnaz Alafchi 3
, Behnaz Alafchi 3 
Author information:
1Department of Prosthodontics, Faculty of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran
2Department of Pediatricdentistry, Faculty of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran
3Biostatistics, Hamadan University of Medical Sciences, Hamadan, Iran
Abstract
Background: This study compared the amount of residual cement at the margin of implant-supported crowns cemented using the polytetrafluoroethylene (PTFE) tape, replica technique, and conventional cementation technique.
Methods: In this in vitro experimental study, a mandibular model underwent full-arch scanning. The right first molar tooth was eliminated on the scan using Exocad software, and a regular implant analog was modelled using the Exocad model creator. The designed abutment was then printed. The implant analog was fixed in place with acrylic resin and scanned using a scan body. A full-zirconia custom abutment was then designed by Exocad. Abutments were fabricated using zirconia and sintered. Twenty-seven resin crowns were fabricated for the abutments, and their fit was assessed. Nine crowns were conventionally cemented by filling half of the crown space with cement, 9 crowns were cemented using PTFE tape, and the remaining 9 were first placed on a resin replica and then cemented on the abutments. The residual cement was weighed using a digital scale, and the groups were compared by one-way ANOVA and LSD test (α=0.05).
Results: The amount of residual cement was significantly different among the three groups, indicating that the amount of residual cement was the highest in conventional cementation, and the lowest in the replica group (P < 0.05). Pairwise comparisons showed significant differences between all groups (P < 0.05).
Conclusions: The replica technique followed by the PTFE tape resulted in the minimum amount of residual cement at the margin of implant-supported cement-retained crowns and are preferred for use in the clinical setting.
Keywords: Dental cements, Crowns, Dental prosthesis, Implant-supported, Polytetrafluoroethylene
Copyright and License Information
© 2023 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Vafaee F, Bagheri Z, Nikanjam S, Daneshyar F, Alafchi B. Amount of residual cement at the margin of implant-supported crowns cemented using the polytetrafluoroethylene tape, replica technique, and conventional cementation technique. Avicenna J Dent Res. 2023; 15(2):42-46. doi:10.34172/ajdr.2023.1657
Background
Dental implants are often the treatment of choice for oral rehabilitation of fully or partially edentulous patients (1). Implant-supported prosthetic crowns can be screw-retained or cement-retained; both types have favorable long-term success rates but have shortcomings as well (2). The advantages of cement-retained restorations, compared with screw-retained types, include higher esthetics, easier application, simpler fabrication process, the potential to correct angulation, higher passive fit, lower cost, and easier accessibility in posterior parts of the ridge (3,4). However, the removal of excess cement is the main problem associated with the use of cement-retained restorations. The margin of implant-supported restorations is often placed deeper than tooth abutments, especially in the esthetic zone. Therefore, in order to improve the emergence profile, it is recommended that the implant should be placed 3-4 mm apical to the cementoenamel junction or buccal gingival margin of the adjacent tooth. Accordingly, the restoration margin is placed > 3 mm subgingivally (5). Removal of excess cement at the subgingival margins is highly difficult (6,7). Residual cement is a major drawback of implant-supported cement-retained restorations (2,8). It can initiate an inflammatory process at the site and lead to peri-implant diseases (9).
Detection and removal of subgingival cement by dental instruments are difficult due to the circular orientation of gingival fibers around the implant-abutment-crown complex (7). Unfortunately, the majority of dental cements do not have adequate radiopacity to be detected on conventional radiographs, and more advanced imaging modalities that may be used for this purpose are not widely accessible (10-12).
In the process of seating of implant-supported cement-retained crowns, the generated hydraulic pressure pushes the cement in the path with the lowest resistance, which is along the gingival sulcus (13). In natural teeth, gingival attachments in the dentogingival complex can resist this process (14). However, flexible gingival attachments are absent in implant abutments, and consequently, excess cement flows subgingivally. On the other hand, attempts to remove excess cement can damage the implant, abutment, or prosthesis. Both the residual cement and the scratched implant or abutment surfaces can lead to plaque accumulation, subsequent development of an inflammatory process around dental implant, soft tissue edema, bleeding on probing, exudation, and even implant failure (15).
The application of retraction cords to prevent cement flow subgingivally is not generally successful, and it can increase the sulcus width and further enhance the cement flow into the subgingival area (16). Polytetrafluoroethylene (PTFE) or Teflon tape has a thickness of < 50 µm and does not increase the sulcus width. Moreover, the surface of PTFE tapes, unlike the retraction cords, does not contain fiber, and therefore, does not entrap the cement (17).
Extraoral cementation of crowns on implant analog is another suggested technique to decrease the residual cement around dental implants (18). The main advantage of extraoral cementation is that the cementation process is performed on the analog. Accordingly, the emergence contours can be ideally formed, and the residual cement can be minimized. Therefore, ideal soft tissue conditions and contour may be achieved, and inflammation, plaque retention, bone loss, and bacterial proliferation are minimized (19). Considering all the above, this study aimed to compare the amount of residual cement at the margin of implant-supported crowns cemented using PTFE tape, replica technique, and conventional cementation technique.
Materials and Methods
This in vitro experimental study was conducted on 27 temporary resin crowns and 27 zirconia abutments in three groups (n = 9) for comparison of three different cementation techniques.
The sample size was calculated to be 9 in each group according to a previous study (8), assuming an alpha of 0.01 and a power of 90% using PWR statistical package in R.3.6.1 software.
A mandibular model (Has Ban Mandegar, Iran) underwent full-arch scanning by a scanner (Amann Girrbach Map 400; Amann Girrbach AG, Koblach, Austria). Next, the right first molar tooth was eliminated on the scan using Exocad software (Exocad GmbH, Darmstadt, Germany), and a regular implant analog (DIO laboratory fixture analog, Dio Implant System Co. Ltd., South Korea) was modelled using Exocad model creator. The designed abutment was then printed. Then, the implant analog was fixed in place with acrylic resin. The fixed analog in the model was scanned using a scan body (Arum, Doowonid). A full-zirconia custom abutment was then designed by Exocad software version 3. The abutments were fabricated using Sirona TZI zirconia (Sirona Dental Systems GmbH, Bensheim, Germany). A4 shade was used for higher contrast. They were then sintered at 1500°C according to the manufacturer’s instructions and placed on the model (Figures 1 and 2). A new scan was obtained and crowns were designed for the abutments using Exocad software. Accordingly, 27 temporary resin crowns were fabricated. The crowns were designed with a hole so that the hole could be closed during cementation and it could be opened to access the screw for retrieval (Figure 3). The fit of the crowns was then assessed. Of all crowns, 9 were conventionally cemented. For this purpose, an equal amount of cement was used in all 9 crowns. Temporary cement (Temp-Bond NE, Kerr; Orange, CA, USA) was injected into each crown to the extent that half of the crown was filled with cement. The crowns were then fixed in place. PTFE tape was used for the cementation of 9 other crowns as described by Hess (17). Accordingly, the tape was used on the abutment without covering the margins, and then the crown, with cement applied on its internal surface, was placed over it. The remaining 9 crowns were first placed on a resin replica and were then cemented on the main abutment (15). The resin replica was fabricated by injecting light-cured resin into the zirconia crowns. The internal surface of the crowns was first lubricated with petroleum jelly, and brass pins were used as a handle for the replicas. The replicas were then removed from the crowns and light-cured (20).

Figure 1.
Zirconia Abutments
.
Zirconia Abutments
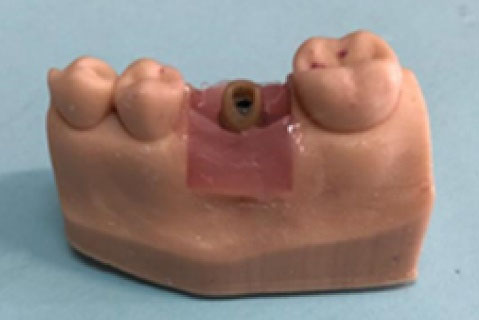
Figure 2.
Zirconia Abutment on Implant Analog
.
Zirconia Abutment on Implant Analog

Figure 3.
Temporary Resin Crowns
.
Temporary Resin Crowns
Prior to each placement of crowns on the abutment, the screw access hole was filled with wax, and excess cement was removed by an explorer as much as possible. Finally, the screw access hole was opened, the crown and abutment were simultaneously removed, and excess cement was measured using a digital scale.
Data were analyzed using SPSS version 24.0. The normal distribution of data was evaluated using the Kolmogorov-Smirnov test and Shapiro-Wilk test. One-way ANOVA and LSD tests were applied for the comparisons at 0.05 level of significance.
Results
Table 1 presents the measures of central dispersion for the residual cement in the three groups. As shown, the highest amount of residual cement was found in the conventional cementation group and the lowest in the replica group. One-way ANOVA showed a significant difference in the amount of residual cement among the three groups (P < 0.001). Pairwise comparisons using the LSD test (Table 2) showed significant differences between all groups (P < 0.05).
Table 1.
Measures of Central Dispersion for the Residual Cement in the Three Groups (n = 9)
|
|
Mean
|
Standard Deviation
|
95% Confidence Interval for Mean
|
Minimum
|
Maximum
|
|
Lower Bound
|
Upper Bound
|
| Conventional |
0.0211000 |
0.00334830 |
0.0187048 |
0.0234952 |
0.01600 |
0.02600 |
| PTFE |
0.0164000 |
0.00518973 |
0.0126875 |
0.0201125 |
0.01000 |
0.02600 |
| Replica |
0.0046000 |
0.00340588 |
0.0021636 |
0.0070364 |
0.00000 |
0.01000 |
| Total |
0.0140333 |
0.00807928 |
0.0110165 |
0.0170502 |
0.00000 |
0.02600 |
Table 2.
Pairwise Comparisons of the Residual Cement between the Groups using the LSD Test
|
Group (I)
|
Group (J)
|
Mean difference (I-J)
|
Standard Error
|
P Value
|
95% Confidence Interval
|
|
Lower Bound
|
Upper Bound
|
| Conventional |
PTFE |
0.00470000* |
0.00182107 |
0.016 |
0.0009635 |
0.0084365 |
| Replica |
0.01650000* |
0.00182107 |
0.000 |
0.0127635 |
0.0202365 |
| PTFE |
Conventional |
-0.00470000* |
0.00182107 |
0.016 |
-0.0084365 |
-0.0009635 |
| Replica |
0.01180000* |
0.00182107 |
0.000 |
0.0080635 |
0.0155365 |
| Replica |
Conventional |
-0.01650000* |
0.00182107 |
0.000 |
-0.0202365 |
-0.0127635 |
| PTFE |
-0.01180000* |
0.00182107 |
0.000 |
-0.0155365 |
-0.0080635 |
*The mean difference is significant at the 0.05 level.
Discussion
This study compared the amount of residual cement at the margin of implant-supported crowns cemented using the PTFE tape, replica technique, and conventional cementation technique. The results showed that the replica technique yielded a significantly lower amount of residual cement than the other two groups. The PTFE tape ranked second and resulted in a significantly lower amount of residual cement than the conventional intraoral cementation technique.
Jagathpal et al (21) compared the amount of residual cement around implant-supported crowns cemented using three different extraoral cementation techniques. They showed the minimum amount of residual cement using printed resin replica. Additionally, the use of replica in general yielded a lower amount of residual cement than the conventional cementation technique (control group). Their results were in agreement with the present findings. Wang et al (22) compared the amount of residual cement using the replica fabricated from cobalt-chromium by the computer-aided design/computer-aided manufacturing technique in different sizes, with the conventional cementation technique. They reported a significantly lower amount of residual cement using replica, especially when the replica had a smaller diameter (by 50 µm) than the main abutment. Despite the use of a different type of replica, their results were in line with the present findings. The use of resin replica, which is fabricated by injection of resin into the crown prior to its cementation, is easier, faster, and cheaper. Kıran et al (23) compared bone loss, microbiological conditions, and biomarkers around implant-supported crowns cemented extraorally and intraorally. They found that the level of crestal bone loss after implant loading was similar in metal-ceramic crowns cemented intraorally and extraorally at the 6-month follow-up. However, the results regarding the microbiological conditions and biomarkers were significantly different in the two groups and were more favorable in the extraoral cementation group. Their results cannot be compared with the present findings due to the in vivo design and different methodologies. However, it appears that the 6-month follow-up may not be long enough for the assessment of microbiological conditions. The present results showed a significantly higher amount of residual cement in conventional cementation, which can result in peri-implant inflammation, edema, pain, increased pocket depth, bleeding or exudation on probing, and radiographic bone loss. Removal of residual cement is difficult and its complete elimination can only be ensured by an exploratory flap surgery or using a dental endoscope (24).
The method used for the fabrication of the replica in the present study was adopted from the study by Rayyan and Makarem (20) who fabricated the replica using thermoplastic materials with high melting points. They injected the material into the crowns and used a dowel pin as a handle to enhance the removal of the replica. This replica was used prior to the cementation of the crown on the main abutment for maximum removal of excess cement. Liang et al (25) compared three different cementation techniques. They injected two different volumes of cement into the crowns according to the conventional cementation method and used a resin replica prior to crown cementation on the main abutment. Consistent with the present study, they concluded that using a resin replica prior to cementation decreased the residual cement, resulted in higher passive fit, and decreased the risk of peri-implantitis. Hess (17) presented a method for the reduction of residual subgingival cement using a PTFE tape. The tape was used on the abutment without covering the margins, and then the crown, with cement applied on its internal surface, was placed over it. Finally, the excess cement was wiped off, and the tape was gently removed. The present results revealed that the method suggested by Hess (17) resulted in a significantly lower amount of residual cement around the implant, compared with the conventional cementation technique. Similar to the present study, Begum et al (15) compared three different cementation protocols, including half filling, use of replica, and venting, regarding the residual cement around implant-supported crowns. They reported that venting of the crown and the use of replica were both effective in decreasing the amount of the residual cement volume, which was in accordance with the present results. Chee et al (3) evaluated different cementation techniques, including application of cement only at the crown margins, application of cement on the apical half of the axial walls of the crown, and covering the entire axial walls of the crown with the cement. In another method, the crowns were first placed on a putty replica. They concluded that the replica method resulted in significantly lower amount of residual cement. Although they used a putty replica, their results were in agreement with the present findings.
This study had an in vitro design and could not simulate the intraoral conditions with respect to the presence of saliva. Therefore, the results may be generalized to the clinical setting with caution. Future in vivo studies are required to obtain more reliable results. Moreover, only one type of temporary cement was evaluated in the present study. Other cement types should be investigated in future studies.
Conclusions
The replica technique followed by the PTFE tape resulted in the minimum amount of residual cement at the margin of implant-supported cement-retained crowns and is preferred for use in the clinical setting.
Authors’ Contribution
Conceptualization: Fariborz Vafaee.
Data curation: Fahimeh Daneshyar.
Formal analysis: Behnaz Alafchi.
Funding acquisition: Zahra Bagheri.
Investigation: Zahra Bagheri.
Methodology: Zahra Bagheri.
Project administration: Zahra Bagheri.
Resources: Zahra Bagheri.
Supervision: Fariborz Vafaee.
Validation: Fariborz Vafaee.
Visualization: Saeed Nik Anjam.
Writing–original draft: Zahra Bagheri.
Writing–review & editing: Zahra Bagheri.
Competing Interests
The authors declare that they have no conflict of interests.
Ethical Approval
This study was approved by Hamadan University of Medical Sciences (Ethics No. IR.UMSHA.REC.1400.762).
References
- Goh EXJ, Lim LP. Implant maintenance for the prevention of biological complications: are you ready for the next challenge?. J Investig Clin Dent 2017; 8(4):e12251. doi: 10.1111/jicd.12251 [Crossref] [ Google Scholar]
- Lee A, Okayasu K, Wang HL. Screw- versus cement-retained implant restorations: current concepts. Implant Dent 2010; 19(1):8-15. doi: 10.1097/ID.0b013e3181bb9033 [Crossref] [ Google Scholar]
- Chee WW, Duncan J, Afshar M, Moshaverinia A. Evaluation of the amount of excess cement around the margins of cement-retained dental implant restorations: the effect of the cement application method. J Prosthet Dent 2013; 109(4):216-21. doi: 10.1016/s0022-3913(13)60047-5 [Crossref] [ Google Scholar]
- Nissan J, Narobai D, Gross O, Ghelfan O, Chaushu G. Long-term outcome of cemented versus screw-retained implant-supported partial restorations. Int J Oral Maxillofac Implants 2011; 26(5):1102-7. [ Google Scholar]
- Shadid R, Sadaqa N. A comparison between screw- and cement-retained implant prostheses. A literature review. J Oral Implantol 2012; 38(3):298-307. doi: 10.1563/aaid-joi-d-10-00146 [Crossref] [ Google Scholar]
- Linkevicius T, Vindasiute E, Puisys A, Peciuliene V. The influence of margin location on the amount of undetected cement excess after delivery of cement-retained implant restorations. Clin Oral Implants Res 2011; 22(12):1379-84. doi: 10.1111/j.1600-0501.2010.02119.x [Crossref] [ Google Scholar]
- Agar JR, Cameron SM, Hughbanks JC, Parker MH. Cement removal from restorations luted to titanium abutments with simulated subgingival margins. J Prosthet Dent 1997; 78(1):43-7. doi: 10.1016/s0022-3913(97)70086-6 [Crossref] [ Google Scholar]
- Quirynen M, De Soete M, van Steenberghe D. Infectious risks for oral implants: a review of the literature. Clin Oral Implants Res 2002; 13(1):1-19. doi: 10.1034/j.1600-0501.2002.130101.x [Crossref] [ Google Scholar]
- Pauletto N, Lahiffe BJ, Walton JN. Complications associated with excess cement around crowns on osseointegrated implants: a clinical report. Int J Oral Maxillofac Implants 1999; 14(6):865-8. [ Google Scholar]
- Wadhwani C, Hess T, Faber T, Piñeyro A, Chen CS. A descriptive study of the radiographic density of implant restorative cements. J Prosthet Dent 2010; 103(5):295-302. doi: 10.1016/s0022-3913(10)60062-5 [Crossref] [ Google Scholar]
- Liu KZ, Xiang XM, Man A, Sowa MG, Cholakis A, Ghiabi E. In vivo determination of multiple indices of periodontal inflammation by optical spectroscopy. J Periodontal Res 2009; 44(1):117-24. doi: 10.1111/j.1600-0765.2008.01112.x [Crossref] [ Google Scholar]
- Pette GA, Ganeles J, Norkin FJ. Radiographic appearance of commonly used cements in implant dentistry. Int J Periodontics Restorative Dent 2013; 33(1):61-8. doi: 10.11607/prd.1466 [Crossref] [ Google Scholar]
- Linkevicius T, Vindasiute E, Puisys A, Linkeviciene L, Maslova N, Puriene A. The influence of the cementation margin position on the amount of undetected cement A prospective clinical study. Clin Oral Implants Res 2013; 24(1):71-6. doi: 10.1111/j.1600-0501.2012.02453.x [Crossref] [ Google Scholar]
- Wadhwani CP. Cementation in Dental Implantology: An Evidence-Based Guide. Springer; 2014. p. 214.
- Begum Z, Sonika R, Pratik C. Effect of different cementation techniques on retained excess cement and uniaxial retention of the implant-supported prosthesis: an in vitro study. Int J Oral Maxillofac Implants 2014; 29(6):1333-7. doi: 10.11607/jomi.3724 [Crossref] [ Google Scholar]
- Bennani V, Schwass D, Chandler N. Gingival retraction techniques for implants versus teeth: current status. J Am Dent Assoc 2008; 139(10):1354-63. doi: 10.14219/jada.archive.2008.0047 [Crossref] [ Google Scholar]
- Hess TA. A technique to eliminate subgingival cement adhesion to implant abutments by using polytetrafluoroethylene tape. J Prosthet Dent 2014; 112(2):365-8. doi: 10.1016/j.prosdent.2013.06.026 [Crossref] [ Google Scholar]
- Dumbrigue HB, Abanomi AA, Cheng LL. Techniques to minimize excess luting agent in cement-retained implant restorations. J Prosthet Dent 2002; 87(1):112-4. doi: 10.1067/mpr.2002.119418 [Crossref] [ Google Scholar]
- Singh R, Mahesh L, Shukla S. Extra oral cementation of implant prosthesis: a case report. J Indian Prosthodont Soc 2013; 13(4):627-30. doi: 10.1007/s13191-013-0319-x [Crossref] [ Google Scholar]
- Rayyan MM, Makarem HA. A modified technique for preventing excess cement around implant supported restoration margins. J Prosthet Dent 2016; 116(6):840-2. doi: 10.1016/j.prosdent.2016.04.007 [Crossref] [ Google Scholar]
- Jagathpal AJ, Vally ZI, Sykes LM, du Toit J. Comparison of excess cement around implant crown margins by using 3 extraoral cementation techniques. J Prosthet Dent 2021; 126(1):95-101. doi: 10.1016/j.prosdent.2020.04.016 [Crossref] [ Google Scholar]
- Wang W, Chang J, Wang HM, Gu XH. Effects of precementation on minimizing residual cement around the marginal area of dental implants. J Prosthet Dent 2020; 123(4):622-9. doi: 10.1016/j.prosdent.2019.04.010 [Crossref] [ Google Scholar]
- Kıran B, Toman M, Buduneli N, Lappin DF, Toksavul S, Nizam N. Intraoral versus extraoral cementation of implant-supported single crowns: clinical, biomarker, and microbiological comparisons. Clin Implant Dent Relat Res 2018; 20(2):170-9. doi: 10.1111/cid.12567 [Crossref] [ Google Scholar]
- Wilson TG Jr. The positive relationship between excess cement and peri-implant disease: a prospective clinical endoscopic study. J Periodontol 2009; 80(9):1388-92. doi: 10.1902/jop.2009.090115 [Crossref] [ Google Scholar]
- Liang T, Hu X, Zhu L, Pan X, Zhou Y, Liu J. Comparative in vitro study of cementing techniques for implant-supported restorations. J Prosthet Dent 2016; 116(1):59-66. doi: 10.1016/j.prosdent.2016.01.014 [Crossref] [ Google Scholar]