Avicenna J Dent Res. 14(2):69-73.
doi: 10.34172/ajdr.2022.13
Original Article
Assessment of Frontal Sinus Morphology and Cervical Vertebral Maturation for Evaluation of Skeletal Maturity
Sanjay Prasad Gupta 1  , Samarika Dahal 2, *
, Samarika Dahal 2, *  , Shristi Rauniyar 3
, Shristi Rauniyar 3 
Author information:
1Department of Orthodontics and Dentofacial Orthopedics, Tribhuvan University Teaching Hospital, MMC, Institute of Medicine, Tribhuvan University, Kathmandu, Nepal
2Department of Oral Pathology and Forensic Dentistry, Tribhuvan University Teaching Hospital, MMC, Institute of Medicine, Tribhuvan University, Kathmandu, Nepal
3Dental Villa-Orthodontic Center and Speciality Dental Clinic, Kathmandu, Nepa
*
Corresponding author: Samarika Dahal, BDS (TU), MDS- Oral Pathology, Msc Forensic Odontology, Department of Oral Pathology and Forensic Dentistry, Tribhuvan University Teaching Hospital, MMC, Institute of Medicine, Tribhuvan University, Kathmandu, Nepal. Tel:+977- 9841363051, Email:
drsamarika@gmail.com
Abstract
Background: The growth prediction using reliable growth assessment methods is an invaluable tool during orthodontic treatment planning. This study aimed to examine the relationship between frontal sinus (FS) morphology and cervical vertebral maturation (CVM) to predict the skeletal maturity of an individual.
Methods: The present study consisted of 252 lateral cephalograms of orthodontic patients. CVM stages and FS parameters such as FS height, FS width, and FS index were assessed using the same lateral cephalogram. Statistical methods including t test, analysis of variance (ANOVA), and Pearson correlation (r) were used for the statistical analysis.
Results: FS height and width were greater in males (24.33±4.21; 10.08±3.20) compared to females (21.43±5.34; 8.12±2.19), indicating a statistical difference (P<0.05). However, FS index did not show a statistically significant difference (P=0.32) between males (2.59±0.74) and females (2.69±0.44). FS height and width increased significantly in a linear fashion from CVM stage 1 to stage 6. FS index, on the other hand, did not exhibit any statistically significant differences among CVM stages in both males and females. FS height and width showed a significant weak to moderate correlation with CVM stages in both males and females. However, FS index exhibited a mild and weak negative correlation with the CVM stages in both males and females.
Conclusions: FS height and width had a significant weak to moderate correlation with CVM stages in both the males and females, while FS index had a weak negative correlation with CVM stages in both males and females. Unlike the CVM method, the FS morphology cannot be reliably utilized to assess the skeletal maturity.
Keywords: Cervical vertebral maturation, Frontal sinus morphology, Growth assessment, Skeletal maturity
Copyright and License Information
© 2022 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Gupta SP, Dahal S, Rauniyar S. Assessment of frontal sinus morphology and cervical vertebral maturation for evaluation of skeletal maturity. Avicenna J Dent Res. 2022; 14(2):69-73. doi:10.34172/ajdr.2022.13
Introduction
For an orthodontist to plan effective therapy, including growth modification treatment in patients with skeletal malocclusions, it is vital to consider their current growth status. Growth modification treatment is performed during the peak growth period. However, orthognathic surgery is carried out after the cessation of growth to avoid the post-surgical relapse caused by growth.
The growth prediction using a reliable growth assessment method would be an invaluable tool during orthodontic treatment planning which in turn gives a good outcome and treatment stability (1,2). Various maturity indicators including chronological age, weight, height, sexual maturation features, dental development, and skeletal maturation have been used to assess the growth status (3). Growth assessment by chronological age is ineffective because it reveals the greatest difference in skeletal maturity among children of the same chronological age (4).
Skeletal maturity assessment using hand and wrist bone ossification is one of the most accurate methods, but it involves additional radiation exposure, which has ethical implications (5,6). Lamparski (7) used lateral cephalograms to examine the maturation of cervical vertebrae and found an association with the skeletal maturation.
Hassel and Farman developed a cervical vertebral maturation (CVM) index by utilizing three cervical vertebrae in lateral cephalograms and found it reliable and valid for determining skeletal age (8). Baccetti et al modified this method afterward (9). Despite several limitations, such as the complexity of categorizing third and fourth cervical vertebral bodies into various shapes, the CVM method is frequently used for determining growth status. However, the CVM approach will require longitudinal follow-up data for accuracy (8-10).
An innovative technique to identify a child’s developmental state is to examine the anatomy of the frontal sinus (FS) during the pubertal growth period. Ruf and Pancherz (11-13) investigated the anatomy of the FS using lateral cephalograms and reported that analogous to body height growth at puberty: FS enlargement exhibited a similar pattern with a well-defined peak.
The main advantage of the CVM method and FS morphology assessment methods is that they do not require additional radiation exposure as they utilize the same lateral cephalograms that are routinely used for orthodontic treatment planning.
Previous studies have shown inconsistent results. According to some studies, the FS can be utilized as an indication for predicting mandibular growth (9). However, some researchers have found that the FS is not the sole reliable criterion for the prediction of skeletal maturity (14). Furthermore, according to some studies, the FS index is unable to distinguish between different growth phases and hence cannot be utilized as a reliable maturity indicator (15). Additionally, no analogous study has been carried out among Nepalese population. The purpose of this study was to find the relationship between FS morphology and CVM for the skeletal maturity assessment.
Materials and Methods
Lateral cephalograms of 252 patients who visited Department of Orthodontics and Dentofacial Orthopedics, Tribhuvan University Teaching Hospital and Dental Villa-Orthodontic Center and Speciality Dental Clinic, Kathmandu, from January 2018 to December 2020 were included in this study.
The sample size was calculated based on a study conducted by Patil and Revankar (14). At different stages of skeletal maturation, the mean difference in the FS index was 0.25 ± 0.26. The power was set at 80%, while the alpha was set at 0.05. Accordingly, a sample of 42 subjects in each cervical stage was calculated. Hence, a total sample size of 252 was estimated for the study.
Before conducting this study, ethical approval was obtained from the Institutional Review Committee of the Institute of Medicine (Ref. 466 (6-11) E2 077/078).
The subjects with good-quality standardized pretreatment lateral cephalograms of ages between 8 and 21 years were included in the study. Subjects with a previous history of sinus pathology, syndromes, craniofacial deformity, trauma or surgery involving cervical vertebrae or FS, and any systemic disease that affects the growth and development were excluded from this study. The radiographs with artifacts that interfered with the location of the anatomical sites were not considered in the study.
All the lateral cephalograms obtained from the single source (Planmeca ProMax® 3D, Europe; exposure 66.0 kV, 8.0 mA, 15.8 s, 84.8 Gycm2) were separated into six groups based on CVM stages, with an equal number of males and females. Cephalometric tracing was done on acetate tracing paper of 0.004-inch thickness using a 4H pencil of 0.5 mm. The principal investigator manually evaluated and measured all the lateral cephalogram images for data collection. The FS height and width measurements were evaluated according to the method used by Ertürk (16). The sella-nasion line was orientated horizontally on the cephalogram. As indicated in Figure 1, the maximum FS height and width were measured. The ratio of each subject’s FS height and width was used to calculate the FS index.
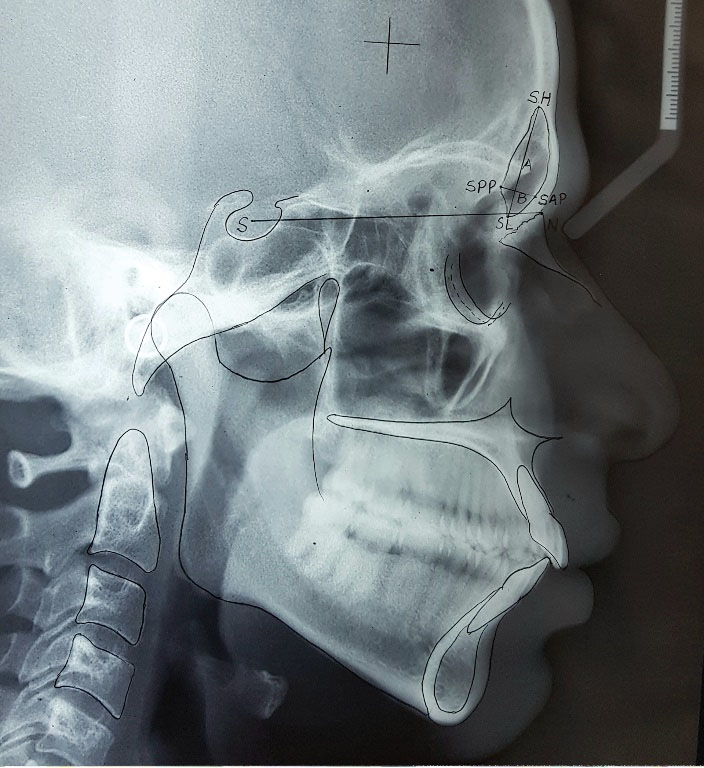
Figure 1.
FS Morphology Assessment on a Lateral Cephalogram. S represents the midpoint of sella turcica; N represents the most anterior point of the frontonasal suture in the midline; FS height (A) is the distance from SH (highest point on the FS) to SL (denotes the lowest point on the FS); Maximum FS width (B) is the distance from SPP (posterior point on the FS) and SAP (anterior point on the FS) perpendicular to A.
.
FS Morphology Assessment on a Lateral Cephalogram. S represents the midpoint of sella turcica; N represents the most anterior point of the frontonasal suture in the midline; FS height (A) is the distance from SH (highest point on the FS) to SL (denotes the lowest point on the FS); Maximum FS width (B) is the distance from SPP (posterior point on the FS) and SAP (anterior point on the FS) perpendicular to A.
The assessment of CVM stages was carried out on the same lateral cephalogram and classified into 6 stages using the methods used by Baccetti et al (9) (Figures 1 and 2).
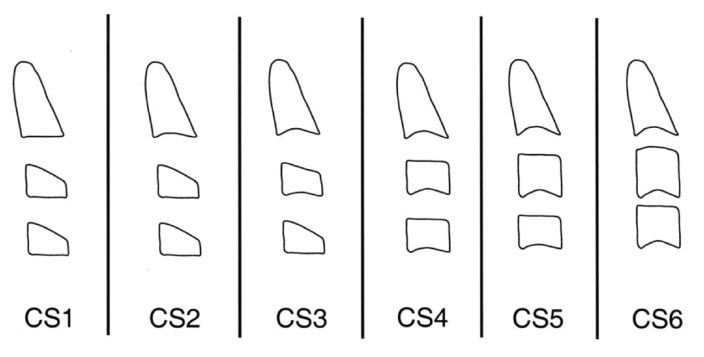
Figure 2.
Cervical Vertebral Maturation Stages.
.
Cervical Vertebral Maturation Stages.
These stages are as follows:
CS 1: Lower borders of all three cervical vertebrae are flat and bodies of both third and fourth cervical vertebrae are trapezoid in shape; the superior border is tapered from posterior to anterior.
CS 2: Concavity is present in the lower border of the second vertebrae and increases in the anterior vertical height of the bodies.
CS 3: Concavities are present at the inferior borders of both the second and third cervical vertebrae. The shape of the C3 and C4 bodies may be either trapezoid or rectangular horizontal.
CS 4: Concavities are present at the inferior borders of the second, third, and fourth cervical vertebrae. The shape of the third and fourth cervical vertebral bodies is rectangular horizontal.
CS 5: Concavities are present at the inferior borders of the second, third, and fourth cervical vertebrae. At least one of the bodies of the third and fourth cervical vertebrae is square in shape. If not square, the shape of other cervical vertebral bodies still is rectangular horizontal.
CS 6: Concavities are evident at the lower borders of the second, third, and fourth cervical vertebrae. The shape of at least one of the third and fourth cervical vertebral bodies is rectangular vertical. If not rectangular vertical, the shape of other cervical vertebral bodies is square.
The data were entered into a Microsoft Excel sheet. The data were evaluated and statistically analyzed using SPSS version 21.0 (Armonk, NY: IBM Corp.). The confidence level was set at 95% (P = 0.05). The FS parameters were compared between genders using a t-test, whereas the values of the FS parameters at different cervical stages were compared using an analysis of variance (ANOVA). The correlation between FS parameters and the CVM stage was evaluated using Pearson correlation (r).
Results
There were equal numbers of males (n = 126) and females (n = 126) among the 252 subjects. The mean age of all the participants was 15.3 ± 6.4 years. Table 1 shows a comparison of FS measurements between males and females. FS height and width in males were greater than in females, with a statistically significant difference. The FS index, on the other hand, did not demonstrate a statistically significant difference between the genders.
Table 1.
The Comparison of Frontal Sinus Measurements Among Genders
|
Parameters
|
Male (n=126)
|
Female (n=126)
|
P Valuea
|
| FS height |
24.33 ± 4.21 |
21.43 ± 5.34 |
0.04* |
| FS width |
10.08 ± 3.20 |
8.12 ± 2.19 |
0.019* |
| FS index |
2.59 ± 0.74 |
2.69 ± 0.44 |
0.32 |
FS, frontal sinus.
a t test; *P < 0.05: statistically significant.
A comparison of FS measurements among different CVM stages is shown in Table 2. From CVM stage 1 (CS1) to CVM 6 (CS6), FS height and width increased in a linear pattern, with a statistically significant difference. FS index, on the other hand, exhibited no significant differences among CVM stages in both genders.
Table 2.
The Comparison of Frontal Sinus Measurements at Different Cervical Vertebral Maturation Stages
|
Parameters
|
Gender
|
CVM Stages
|
P Valuea
|
|
CS-1
|
CS-2
|
CS-3
|
CS-4
|
CS-5
|
CS-6
|
| FS height |
Male |
16.58 ± 5.31 |
18.21 ± 4.23 |
19.42 ± 3.87 |
22.31 ± 5.23 |
23.12 ± 4.74 |
26.32 ± 3.41 |
0.03* |
| Female |
15.72 ± 4.82 |
16.61 ± 5.21 |
18.32 ± 3.73 |
19.21 ± 4.21 |
20.53 ± 4.21 |
23.71 ± 3.82 |
0.04* |
| FS width |
Male |
7.63 ± 1.21 |
7.48 ± 2.53 |
8.53 ± 2.28 |
9.24 ± 2.21 |
10.74 ± 2.84 |
12.56 ± 1.32 |
0.012* |
| Female |
6.41 ± 2.32 |
7.82 ± 1.34 |
7.43 ± 2.21 |
8.23 ± 1.87 |
9.82 ± 2.04 |
10.32 ± 3.21 |
0.017* |
| FS index |
Male |
2.24 ± 0.73 |
2.32 ± 0.43 |
2.81 ± 0.15 |
2.49 ± 0.32 |
2.18 ± 0.91 |
2.97 ± 0.72 |
0.21 |
| Female |
2.51 ± 0.32 |
2.87 ± 0.52 |
2.75 ± 0.73 |
2.37 ± 0.52 |
2.25 ± 0.32 |
2.92 ± 0.71 |
0.42 |
FS, frontal sinus; CVM, cervical vertebral maturation.
a ANOVA, *P < 0.05 = statistically significant
The correlation between FS measurements and CVM stages is depicted in Table 3. Both males and females had a moderate correlation between FS height and CVM stages. The FS width had a significant weak correlation with CVM stages in males, but it had a substantial moderate correlation in females. Furthermore, in both males and females, the FS index exhibited an insignificant and weak negative correlation with CVM stages.
Table 3.
Correlation Between Frontal Sinus Measurements and Cervical Vertebral Maturation Stages
|
Parameters
|
Gender
|
Correlation with CVM Stages
|
P Value
|
| FS height |
Male |
0.621 |
0.02* |
| Female |
0.542 |
0.03* |
| FS width |
Male |
0.484 |
0.02* |
| Female |
0.737 |
0.01* |
| FS index |
Male |
-0.412 |
0.421 |
| Female |
-0.097 |
0.732 |
FS, frontal sinus; CVM, cervical vertebral maturation.
*P < 0.05: statistically significant; weak correlation: r = ± 0.01-0.5, moderate correlation: ± 0.5-0.8, strong correlation: ± 0.8-1
Intra-examiner reliability showed a strong correlation for FS height (r = 0.93), FS width (r = 0.96) measurements, and CVM stages (r = 0.97).
Discussion
The distinctive properties of FS in terms of size, shape, and position makes frontal bone anatomically unique. Paranasal sinuses follow the same growth pattern as bone (17,18).
During the fourth week of intrauterine life, FS begins to develop. It continues to grow throughout childhood and reaches its maximum size and shape in early adulthood (19). At the age of eight years, the FS is visible on radiographs (18). Because the FS is resistant to trauma and is likely to survive mass disasters, it could be useful for human identification as well.
The expansion of the FS is dependent on the growth of the cranial vault (20), so its growth synchronizes with craniofacial growth. The FS enlargement occurs about 1.5 years after the adolescent growth spurt (12,21).
Gagliardi et al (22) studied Aboriginal Australians and discovered a strong link between hand-wrist ossification and FS growth, suggesting that FS enlargement might be utilized to predict the adolescent growth spurts. Valverde et al (21) conducted a study on Japanese young girls and discovered that FS enlargement is linked to the body height increase during puberty.
As there is a possibility of magnification error in cephalometry, FS index is recommended in this study rather than absolute height and breadth measurements. Another reason is that the height and width of the FS might vary depending on the patients’ physical size and gender (23,24). In both genders, the FS height increases in a linear fashion as they progressed through the CVM stages. Males had a higher FS height than females. The findings of Mahmood et al (15), Hanson and Owsley (25), and Ponde et al (26) are in agreement with this study.
Similarly, as CVM stages progressed, FS width increases in a linear fashion in both genders. The FS width of males was greater than that of females. Similar findings were obtained by Ruf and Pancherz (11,13) and Mahmood et al (15). The FS index, on the other hand, was unable to distinguish between the various stages of the growth spurt since it revealed no consistent pattern among the CVM stages. Mahmood et al (15) and Patil and Revankar (14) found similar results. This is due to a small but consistent increase in FS height and width, which results in a minimal change in FS index values.
Cervical vertebrae have long been utilized in forensics. Sexual dimorphism is based on their shapes and sizes, according to various studies (27). They have been used for stature estimation (28). Their correlation with age has attracted a lot of attention. Türkoz et al assessed the C3 and C4 vertebral body heights, using regression analysis to establish a formula, and discovered that they can be used to determine age in both legal and therapeutic situations (29). Numerous medico-legal issues such as the legal ages to consent to sex, drink alcohol, marry, and work as a minor require age assessment. Individuals who are illegal or have lost their legal status can be examined to estimate their chronological age using CVM. At around 15–16 years of age, the somatic pattern of cervical vertebral growth reaches its final maturation, with the greatest cervical vertebral growth rate occurring between 10 and 12 years (30,31). However, a few studies have shown that the use of a single variable, such as CVM, is unreliable in estimating age. The predictability increases as the number of variables, such as tooth eruption and mineralization of various teeth in the quadrant. To boost predictability, and reduce the variability, CVM should be combined with other information gathered.
Despite the fact that longitudinal studies are reliable methods for assessing a patient’s growth spurt status, the present study selected a cross-sectional study design to minimize unnecessary radiation exposure. Multicenter collaborative longitudinal studies in diverse population groups with greater sample sizes are recommended to make these findings more conclusive. Instead of two-dimensional cephalometric imaging, volumetric imaging is recommended for assessing the different growth spurt stages.
Conclusions
Although FS height and width are significantly associated with CVM stages in both males and females, the correlation is weak to moderate. The FS index, on the other hand, has an insignificant weak negative correlation with CVM stages in both males and females. Hence, unlike the CVM method, the FS morphology cannot be utilized reliably to assess the skeletal maturity of the patient.
Authors’ Contribution
SPG contributed to the design of this study, data collection, data analysis, and manuscript writing. SD contributed to the design of this study, result interpretation, and manuscript writing. SR contributed to data collection and manuscript preparation.
Conflict of Interest Disclosures
The authors declare no conflict of interests.
Ethical Statement
Ethical approval was obtained from the Institutional Review Committee of the Institute of Medicine (Ref. 466 (6-11) E2 077/078).
References
- Kolodziej RP, Southard TE, Southard KA, Casko JS, Jakobsen JR. Evaluation of antegonial notch depth for growth prediction. Am J Orthod Dentofacial Orthop 2002; 121(4):357-63. doi: 10.1067/mod.2002.121561 [Crossref] [ Google Scholar]
- Moore RN, Moyer BA, DuBois LM. Skeletal maturation and craniofacial growth. Am J Orthod Dentofacial Orthop 1990; 98(1):33-40. doi: 10.1016/0889-5406(90)70029-c [Crossref] [ Google Scholar]
- Negi KS, Sharma VP, Kapoor DN, Tandon P. Assessment of growth impetus using MP3 maturation and its correlation with CVMI and dental age. J Indian Orthod Soc 2003; 36(4):204-13. [ Google Scholar]
- Finkel D, Whitfield K, McGue M. Genetic and environmental influences on functional age: a twin study. J Gerontol B Psychol Sci Soc Sci 1995; 50(2):P104-13. doi: 10.1093/geronb/50b.2.p104 [Crossref] [ Google Scholar]
- Houston WJ, Miller JC, Tanner JM. Prediction of the timing of the adolescent growth spurt from ossification events in hand-wrist films. Br J Orthod 1979; 6(3):145-52. doi: 10.1179/bjo.6.3.145 [Crossref] [ Google Scholar]
- Houston WJ. Relationships between skeletal maturity estimated from hand-wrist radiographs and the timing of the adolescent growth spurt. Eur J Orthod 1980; 2(2):81-93. doi: 10.1093/ejo/2.2.81 [Crossref] [ Google Scholar]
- Lamparski D. Skeletal Age Assessment Utilizing Cervical Vertebrae [thesis]. Pittsburgh: University of Pittsburgh; 1972.
- Hassel B, Farman AG. Skeletal maturation evaluation using cervical vertebrae. Am J Orthod Dentofacial Orthop 1995; 107(1):58-66. doi: 10.1016/s0889-5406(95)70157-5 [Crossref] [ Google Scholar]
- Baccetti T, Franchi L, McNamara JA. The cervical vertebral maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod 2005; 11(3):119-29. doi: 10.1053/j.sodo.2005.04.005 [Crossref] [ Google Scholar]
- Franchi L, Baccetti T, McNamara JA Jr. Mandibular growth as related to cervical vertebral maturation and body height. Am J Orthod Dentofacial Orthop 2000; 118(3):335-40. doi: 10.1067/mod.2000.107009 [Crossref] [ Google Scholar]
- Ruf S, Pancherz H. Development of the frontal sinus in relation to somatic and skeletal maturity A cephalometric roentgenographic study at puberty. Eur J Orthod 1996; 18(5):491-7. doi: 10.1093/ejo/18.5.491 [Crossref] [ Google Scholar]
- Ruf S, Pancherz H. Frontal sinus development as an indicator for somatic maturity at puberty?. Am J Orthod Dentofacial Orthop 1996; 110(5):476-82. doi: 10.1016/s0889-5406(96)70053-7 [Crossref] [ Google Scholar]
- Ruf S, Pancherz H. Can frontal sinus development be used for the prediction of skeletal maturity at puberty?. Acta Odontol Scand 1996; 54(4):229-34. doi: 10.3109/00016359609003529 [Crossref] [ Google Scholar]
- Patil AA, Revankar AV. Reliability of the frontal sinus index as a maturity indicator. Indian J Dent Res 2013; 24(4):523. doi: 10.4103/0970-9290.118372 [Crossref] [ Google Scholar]
- Mahmood HT, Shaikh A, Fida M. Association between frontal sinus morphology and cervical vertebral maturation for the assessment of skeletal maturity. Am J Orthod Dentofacial Orthop 2016; 150(4):637-42. doi: 10.1016/j.ajodo.2016.03.022 [Crossref] [ Google Scholar]
- Ertürk N. [Teleroentgen studies on the development of the frontal sinus]. Fortschr Kieferorthop 1968; 29(2):245-8. doi: 10.1007/bf02166254 [Crossref] [ Google Scholar]
- Maresh MM. Paranasal sinuses from birth to late adolescence. Am J Dis Child 1940; 60(1):55-78. doi: 10.1001/archpedi.1940.02000010064005 [Crossref] [ Google Scholar]
- Dolan KD. Paranasal sinus radiology, part IA: introduction andthe frontal sinuses. Head Neck Surg 1982; 4(4):301-11. doi: 10.1002/hed.2890040407 [Crossref] [ Google Scholar]
- Duque CS, Casiano RR. Surgical anatomy and embryology of the frontal sinus. In: Kountakis SE, Senior BA, Draf W, eds. The Frontal Sinus. Berlin: Springer; 2005. p. 21-31. 10.1007/3-540-27607-6_3.
- Brown WA, Molleson TI, Chinn S. Enlargement of the frontal sinus. Ann Hum Biol 1984; 11(3):221-6. doi: 10.1080/03014468400007091 [Crossref] [ Google Scholar]
- Valverde Y, Watanabe N, Yamaki M, Saito I. The frontal sinus enlargement as an indicator of growth maturity in class III patients-a pilot study. Int J Med Sci Public Health 2013; 2(2):451-5. doi: 10.5455/ijmsph.2013.2.430-434 [Crossref] [ Google Scholar]
- Gagliardi A, Winning T, Kaidonis J, Hughes T, Townsend GC. Association of frontal sinus development with somatic and skeletal maturation in Aboriginal Australians: a longitudinal study. Homo 2004; 55(1-2):39-52. doi: 10.1016/j.jchb.2004.06.001 [Crossref] [ Google Scholar]
- Grummons DC, Kappeyne van de Coppello MA. A frontal asymmetry analysis. J Clin Orthod 1987; 21(7):448-65. [ Google Scholar]
- Shapiro R, Schorr S. A consideration of the systemic factors that influence frontal sinus pneumatization. Invest Radiol 1980; 15(3):191-202. doi: 10.1097/00004424-198005000-00004 [Crossref] [ Google Scholar]
- Hanson CL, Owsley DW. Frontal sinus size in Eskimo populations. Am J Phys Anthropol 1980; 53(2):251-5. doi: 10.1002/ajpa.1330530209 [Crossref] [ Google Scholar]
- Ponde JM, Andrade RN, Via JM, Metzger P, Teles AC. Anatomical variations of the frontal sinus. Int J Morphol 2008; 26(4):803-8. [ Google Scholar]
- Chatzigianni A, Halazonetis DJ. Geometric morphometric evaluation of cervical vertebrae shape and its relationship to skeletal maturation. Am J Orthod Dentofacial Orthop 2009;136(4):481.e1-481.e9. 10.1016/j.ajodo.2009.04.017.
- Saadat Mostafavi SR, Memarian A, Motamedi O, Khaleghi M, Pouromidi M. Height estimation based on second cervical vertebra measured using three-dimensional computed tomographic scanning in Iranian adults. BMC Res Notes 2019; 12(1):599. doi: 10.1186/s13104-019-4634-0 [Crossref] [ Google Scholar]
- Türkoz Ç, Kaygısız E, Ulusoy Ç, Ateş C. A practical formula for determining growth. Diagn Interv Radiol 2017; 23(3):194-8. doi: 10.5152/dir.2016.16334 [Crossref] [ Google Scholar]
- Banda TR, Komuravelli AK, Balla SB, Korrai BR, Alluri K, Kondapaneni J. Discriminatory ability of cervical vertebral maturation stages in predicting attainment of the legal age threshold of 14 years: a pilot study using lateral cephalograms. Imaging Sci Dent 2020; 50(3):209-16. doi: 10.5624/isd.2020.50.3.209 [Crossref] [ Google Scholar]
- Thevissen PW, Kaur J, Willems G. Human age estimation combining third molar and skeletal development. Int J Legal Med 2012; 126(2):285-92. doi: 10.1007/s00414-011-0639-5 [Crossref] [ Google Scholar]