Avicenna J Dent Res. 14(2):92-95.
doi: 10.34172/ajdr.2022.18
Case Report
Reconstruction of Scalp Basal Cell Carcinoma Using Pinwheel Flap: A Case Report
Omid Soltaninia 1  , Arsalan Ebrahimifard 2, *
, Arsalan Ebrahimifard 2, *  , Keihan Soleimani 3
, Keihan Soleimani 3
Author information:
1Assistant Professor, Department of Oral and Maxillofacial Surgery, Dentistry School, Hamadan University of Medical Sciences, Hamadan, Iran
2Resident of Oral and Maxillofacial Surgery, Dentistry School, Hamadan University of Medical Sciences, Hamadan, Iran
3Department of Oral and Maxillofacial Surgery, Dentistry School, Hamadan University of Medical Sciences, Hamadan, Iran
Abstract
Ideal reconstruction of the scalp should ensure adequate coverage and protection of the underlying areas of the reconstruction site, include an adequate volume of soft and hard tissue, and contour the reconstruction of the area to accelerate wound healing, acceptable beauty, and proper function and reduce complications after the operation. This study aimed to present our experience regarding basal cell carcinoma (BCC) in the scalp and show the reconstructive option for BCC cancer in the scalp. A 69-year-old man was admitted due to the recurrence of the lesions in the forehead and scalp area, and he underwent surgery again one year ago. On initial examination, a lesion sized 5 cm× 5cm with an indistinct margin was visible in the frontal region. The lesion had bleeding, itching, and purulent discharge. Computed tomography scan results indicated skull bone resorption, and pathologic report showed active ulcer BCC with infiltrative growth pattern widely disseminated in deep portion. Tumor size was 4.5 cm × 4.3 cm × 1.5 cm and was negative for lymphovascular invasion. The patient was organized for wide local excision of the lesion. Following the tumor resection, the remaining oval defect was reconstructed using the pinwheel flap under general anesthesia in the operating room. It seems that the pinwheel flap design is an effective approach for the reconstruction of extensive lesions of the scalp.
Keywords: Basal cell carcinoma, Pinwheel flap, Reconstruction, Scalp lesion
Copyright and License Information
© 2022 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Soltaninia O, Ebrahimifard A, Soleimani K. Reconstruction of scalp basal cell carcinoma using pinwheel flap: a case report. Avicenna J Dent Res. 2022; 14(2):92-95. doi:10.34172/ajdr.2022.18.
Introduction
The scalp consists of different layers including skin, subcutaneous tissue, galea aponeurotica, loose areolar tissue, and pericranium (1,2). The first three layers are attached as a single unit that can move along the loose areolar tissue over the pericranium, which adheres to the calvaria bone. Nerves, blood vessels, and lymph are located between the subcutaneous tissue and galea aponeurotica. Nerve branches of either the trigeminal nerve or the cervical nerve supply the scalp. The scalp in the forehead area receives its blood supply from the supracellular (medial) and supraorbital (lateral) arteries (1,3). Having an approximate thickness of 3 to 8 mm, the scalp is considered the thickest skin on the body (3).
The scalp can be harmed for a variety of reasons such as trauma, burns, as well as benign and malignant tumors (1,4,5). Basal cell carcinoma (BCC) constitutes approximately 75% of nonmelanoma skin cancers. It usually occurs in older patients, specifically in those regularly and intensively exposed to ultraviolet radiation during their lives (6). The risk of developing BCC during life varies between 29% and 55% (7). BCC is a tumor with gradual growth and a low probability of metastasis. However, this tumor is locally invasive and can strongly affect the underlying organs (8).
The main goal of BCC treatment is to completely remove the lesion and reconstruct the defect created acceptably in terms of beauty and anatomy (5). Giant BCC refers to BCCs that are more than 5 mm in diameter. This carcinoma often requires the removal of soft and hard tissue of the skull and dura (9). The prognosis of the lesion depends on factors such as the number of recurrences, immunohistochemistry of the lesion, involvement of the underlying structures, tumor location, tumor size, gender, and depth of the lesion. This lesion requires at least 5 years of follow-up (10). Factors such as low scalp elasticity, thick skin, bony convexities, large defect size, history of local radiotherapy, and difficulty in delivering blood to large blockages make the reconstruction of the defective area even more challenging (4,5,11). Therefore, an ideal reconstruction should ensure adequate coverage and protection of the underlying areas of the reconstruction site, include an adequate volume of soft and hard tissue, contour reconstruction of the area to accelerate wound healing, acceptable beauty, proper function, and reduce complications after the operation (4,5,12,13). The present study aimed to present our experience regarding BCC in the scalp and to show our reconstructive option for this type of cancer in the scalp.
Case Presentation
A 69-year-old man was admitted to our clinic with the chief complaint of a wound on his forehead. The patient was a nomad treated for multiple lesions in the scalp, behind the ears, and neck approximately three years ago. Due to the recurrence of the lesions in the frontal area, he underwent surgery again one year ago. The scalp lesions recurred for the second time after 4 months, and since the patient’s symptoms worsened, he was finally admitted for surgery.
On initial examination, a lesion sized 5 cm×5 cm with an indistinct margin was visible in the frontal region. The lesion had bleeding, itching, and purulent discharge (Figure 1).
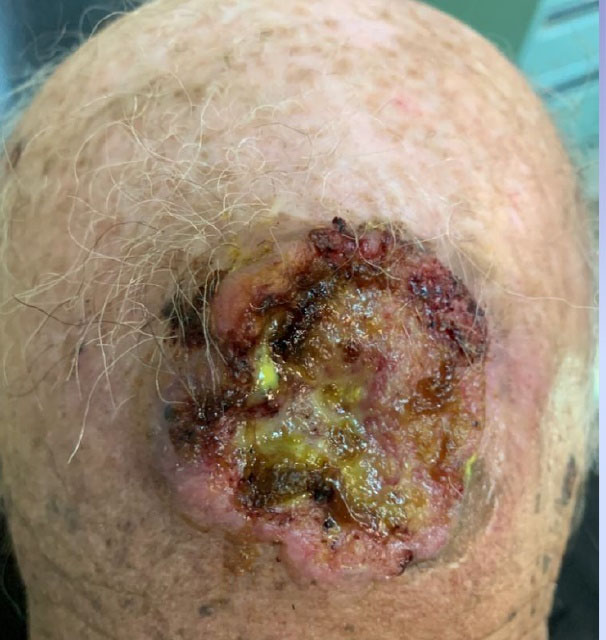
Figure 1.
The Appearance of the Wound in the Studied Patient.
.
The Appearance of the Wound in the Studied Patient.
There was no pain or tenderness on touching the lesion. During the examination, there was no paraesthesia, paralysis, or anesthesia. Further, lymphadenopathy was not seen on examination of cervical lymph nodes, and there was no clear evidence of intracerebral invasion. Computed tomography scan results indicated skull bone resorption (Figure 2).

Figure 2.
Skull Bone Resorption of the Patient.
.
Skull Bone Resorption of the Patient.
Routine laboratory findings revealed mild anemia (red blood cell = 4.14 million/mm3 and hemoglobin = 12.5 g/dL). Further, the erythrocyte sedimentation rate was high (53%) and C-reactive protein was 1+. Moreover, the blood sugar was lower than the normal range (blood sugar = 59 mg/dL). In addition, pathologic report showed active ulcer BCC with infiltrative growth pattern and widely disseminated in deep portion. Tumor size was 4.5 cm × 4.3 cm × 1.5 cm and was negative for lymphovascular invasion.
The patient was organized for wide local excision of the lesion. Following the tumor resection, the remaining oval defect was reconstructed using the pinwheel flap under general anesthesia in the operating room. This technique involves raising four small rotation flaps which are 90° apart from each other and join into a defect in their center (Figure 3). When the central circle was excised to create a defect, four pinwheel flaps with a 16-mm base length were created at the four points of the compass. The flaps were incised along the margins and then were sutured such that they met in the defect center after being rotated and advanced. At this time, negligible excess triangles were formed at the inner edges of the flaps, which were excised through their base by beveling of flap edges to facilitate formal tension-free primary closure (Figure 4).

Figure 3.
Design of the Local Flap Before Wide Local Excision.
.
Design of the Local Flap Before Wide Local Excision.

Figure 4.
Immediate Postoperative Result.
.
Immediate Postoperative Result.
Discussion
Scalp injuries and their management have always been challenging. Closed skin with poor design and high stress over time causes a large, atrophic, and unpleasant wound. In the scalp area, the size and location of the defect are the two most essential factors in deciding the appropriate corrective approach along with the patient’s age and comorbidities (14,15).
Several flaps have been designated for closing moderate-sized circular skin defects on the scalp and region (16,17). Most of these flaps necessitate wide-field dissection of the adjacent normal tissues, frequently imposing a degree of distortion on the subunits tissue (18,19). In less elastic regions (i.e., the scalp), transposition and rotation flaps are either inadequate for closure or lead to secondary defects requiring grafting or reconstruction with a flap (20). However, a pinwheel flap design effectively recruits all the tissue to the adjacent defect. As a result, the destruction of uninvolved and subunit tissues is minimized.
Vecchione and Griffith first described pinwheel flaps in 1978 for large defects (21). Since the flap evenly distributes skin tension, the pinwheel design minimizes scarring and protects hair follicles, all in one operation without the need for a gap thickness graft to cover the donor site.In addition, if reoperation is required in that area, the defect may be repaired by simplifying the flaps, thereby minimizing additional scarring. Likewise, small to large defects in the scalp area should be the preferred option. The main limitation of the pinwheel flap is that it may only be used on areas inside the hairline. The explanation is that using it on the frontal region and forehead area, by design, can cause significant scarring. In addition, it can be complicated by ischemia when applied to larger defects such as those presented. The scalp needs a rich blood supply. In addition, due to the skin’s lack of elasticity in the area, high stresses in the soft tissue lead to a high probability of ischemic complications. Therefore, the option of postoperative tissue edema can be prevented by proper attenuation for tight tension closure and proper suture placement (22,23).
Conclusions
It seems that the pinwheel flap design is the effective approach for the reconstruction of extensive lesions of the scalp.
Conflict of Interest Disclosures
The authors declare that they have no conflict of interests.
Ethical Statement
Informed consent was obtained from the patient for the publication of this report.
References
- Sokoya M, Inman J, Ducic Y. Scalp and forehead reconstruction. Semin Plast Surg 2018; 32(2):90-4. doi: 10.1055/s-0038-1642638 [Crossref] [ Google Scholar]
- Steiner D, Horch RE, Eyüpoglu I, Buchfelder M, Arkudas A, Schmitz M. Reconstruction of composite defects of the scalp and neurocranium-a treatment algorithm from local flaps to combined AV loop free flap reconstruction. World J Surg Oncol 2018; 16(1):217. doi: 10.1186/s12957-018-1517-0 [Crossref] [ Google Scholar]
- Snell RS. Clinical Anatomy for Medical Students. Little, Brown and Company; 1995.
- Lembo F, Cecchino LR, Parisi D, Portincasa A. Utility of a new artificial dermis as a successful tool in face and scalp reconstruction for skin cancer: analysis of the efficacy, safety, and aesthetic outcomes. Dermatol Res Pract 2020; 2020:4874035. doi: 10.1155/2020/4874035 [Crossref] [ Google Scholar]
- Goldman A, Wollina U. Defect closure after successful skin cancer surgery of the nose: a report of 52 cases. Acta Dermatovenerol Alp Pannonica Adriat 2020; 29(4):209-14. [ Google Scholar]
- Nakayama M, Tabuchi K, Nakamura Y, Hara A. Basal cell carcinoma of the head and neck. J Skin Cancer 2011; 2011:496910. doi: 10.1155/2011/496910 [Crossref] [ Google Scholar]
- Miller DL, Weinstock MA. Nonmelanoma skin cancer in the United States: incidence. J Am Acad Dermatol 1994; 30(5 Pt 1):774-8. doi: 10.1016/s0190-9622(08)81509-5 [Crossref] [ Google Scholar]
- Martins PC, Filipe RV, Barbosa R, Julião I, Azevedo R, Ribeiro M. Basal cell carcinoma: multimodal treatment and the role of neoadjuvant vismodegib. Autops Case Rep 2019; 9(4):e2019116. doi: 10.4322/acr.2019.116 [Crossref] [ Google Scholar]
- Kwon CS, Awar OA, Ripa V, Said G, Rocka S. Basal cell carcinoma of the scalp with destruction and invasion into the calvarium and dura mater: report of 7 cases and review of literature. J Clin Neurosci 2018; 47:190-7. doi: 10.1016/j.jocn.2017.09.028 [Crossref] [ Google Scholar]
- Florescu IP, Turcu EG, Carantino AM, Cocoşilă LC, Enache V, Neagu TP. The curious case of a forehead metatypical basal cell carcinoma. Rom J Morphol Embryol 2018; 59(1):345-52. [ Google Scholar]
- Cho GJ, Wang F, Garcia SM, Viner J, Hoffman WY, McDermott MW. Recalcitrant invasive skin cancer of the scalp: combined extirpation and microsurgical reconstruction without cranioplasty. J Craniofac Surg 2017; 28(2):325-30. doi: 10.1097/scs.0000000000003384 [Crossref] [ Google Scholar]
- Puviani M, Curci M. The “Batman flap”: a novel technique to repair a large central glabellar defect. Int J Dermatol 2018; 57(4):477-9. doi: 10.1111/ijd.13844 [Crossref] [ Google Scholar]
- Rysz M, Grzelecki D, Mazurek M, Starościak S, Krajewski R. Surgical techniques for closure of a scalp defect after resection of skin malignancy. Dermatol Surg 2017; 43(5):715-23. doi: 10.1097/dss.0000000000001067 [Crossref] [ Google Scholar]
- Simsek T, Eroglu L. Versatility of the pinwheel flap to reconstruct circular defects in the temporal and scalp region. J Plast Surg Hand Surg 2013; 47(2):97-101. doi: 10.3109/2000656x.2012.736387 [Crossref] [ Google Scholar]
- Wong CH, Wei FC. Anterolateral thigh flap. Head Neck 2010; 32(4):529-40. doi: 10.1002/hed.21204 [Crossref] [ Google Scholar]
- Alvarado A. Reciprocal incisions for closure of circular skin defects. Plast Reconstr Surg 1981; 67(4):482-91. doi: 10.1097/00006534-198104000-00009 [Crossref] [ Google Scholar]
- Keser A, Sensöz O, Mengi AS. Double opposing semicircular flap: a modification of opposing Z-plasty for closing circular defects. Plast Reconstr Surg 1998; 102(4):1001-7. doi: 10.1097/00006534-199809040-00011 [Crossref] [ Google Scholar]
- Yap L, Langstein H. Reconstruction of the scalp, calvarium, and forehead. In: Grabb and Smith’s Plastic Surgery. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2007. p. 358-66.
- Misirlioglu A, Karaca M, Akoz T. Primary cutis verticis gyrata and scalp reduction in one stage with multiple pinwheel flaps (revisited). Dermatol Surg 2008; 34(7):935-8. doi: 10.1111/j.1524-4725.2008.34180.x [Crossref] [ Google Scholar]
- Summers BK, Siegle RJ. Facial cutaneous reconstructive surgery: general aesthetic principles. J Am Acad Dermatol 1993; 29(5 Pt 1):669-81. doi: 10.1016/0190-9622(93)70230-q [Crossref] [ Google Scholar]
- Vecchione TR, Griffith L. Closure of scalp defects by using multiple flaps in a pinwheel design. Plast Reconstr Surg 1978; 62(1):74-7. doi: 10.1097/00006534-197807000-00009 [Crossref] [ Google Scholar]
- Varnalidis I, Mantelakis A, Spiers HVM, Papadopoulou AN. Application of the pinwheel flap for closure of a large defect of the scalp. BMJ Case Rep 2019; 12(8):e229420. doi: 10.1136/bcr-2019-229420 [Crossref] [ Google Scholar]
- Woodard CR. Complications in facial flap surgery. Facial Plast Surg Clin North Am 2013; 21(4):599-604. doi: 10.1016/j.fsc.2013.07.009 [Crossref] [ Google Scholar]