Avicenna J Dent Res. 12(2):51-57.
doi: 10.34172/ajdr.2020.11
Original Article
Comparison of Preemptive Analgesic Effects of Intravenous Ketorolac and Oral Pregabalin in Patients Undergoing Mandibular Fracture Surgery: A Randomized Clinical Trial
Javad Yazdani 1  , Saeed Nezafati 1, Ali Mortazavi 1, Farrokh Farhadi 1, Milad Ghanizadeh 2, *
, Saeed Nezafati 1, Ali Mortazavi 1, Farrokh Farhadi 1, Milad Ghanizadeh 2, * 
Author information:
1Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Tabriz University of Medical Sciences, Tabriz, Iran.
2Postgraduate Student, Dental and Periodontal Research Center, Tabriz University of Medical Sciences, Tabriz, Iran.
Abstract
Background: Preemptive analgesia is one of the techniques to manage postoperative pain, which increases patient satisfaction and decreases the duration of hospitalization. The present study aimed to evaluate and compare the pain relief achieved by preoperative intravenous ketorolac and oral pregabalin in patients undergoing surgery for mandibular fractures.
Methods: In the present clinical trial, 60 patients with unilateral fractures of the mandible were randomly assigned to two groups. In group A, intravenous injections of ketorolac 30 mg and in group B, pregabalin 150 mg capsules were administrated one hour preoperatively. The severity of pain was determined using a visual analog scale (VAS) up to 24 hours postoperatively. Finally, the total doses of an opioid analgesic (pethidine) prescribed for each patient in mg during the first 24 hours and the time for the request of the first analgesic dose in minutes were recorded for each patient. Then, their means were compared between the two groups.
Results: Maximum pain severity was experienced immediately after surgery, which decreased gradually during the 24-hour postoperative period (P < 0.0001). The mean severity of pain immediately after regaining consciousness and the mean pain score during the 24-hour postoperative period were lower in the pregabalin group than in the ketorolac group (P < 0.0001). In the ketorolac group, a slightly higher dose of the opioid was administered; however, the difference was not significant (P > 0.05).
Conclusions: The oral administration of pregabalin 150 mg one hour preoperatively was more effective than the intravenous administration of ketorolac 30 mg in relieving postoperative pain.
Keywords: Ketorolac, Mandibular fracture, Pain, Preemptive, Pregabalin
Copyright and License Information
© 2020 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Yazdani J, Nezafati S, Mortazavi A, Farhadi F, Ghanizadeh M. Comparison of preemptive analgesic effects of intravenous ketorolac and oral pregabalin in patients undergoing mandibular fracture surgery: A Randomized Clinical Trial. Avicenna J Dent Res. 2020;12(2):51-57. doi: 10.34172/ajdr.2020.11.
Background
Highlights
-
The pain severity immediately after regaining consciousness was lower in the pregabalin group than in the ketorolac group.
-
The mean 24-hour pain score was lower in the pregabalin group than in the ketorolac group.
-
The dose of the opioid used in the ketorolac group was slightly higher, and the time for requesting an opioid dose was shorter compared to the pregabalin group. However, this finding was not statistically significant.
One of the most common concerns of patients is postoperative pain because millions of cells are injured during the surgery, leading to inflammation and the release of chemical mediators that cause pain (1,2). In recent years, the majority of surgeons and anesthesiologists have become interested in the use of more effective techniques and analgesics, or preemptive treatment modalities, to decrease postoperative pain (3-7). Non-steroidal anti-inflammatory drugs (NSAIDs) s are a group of medications that constitute a part of preemptive treatments in managing postoperative pain and are used alone or in combination with opioids (1,8). Ketorolac is an injectable NSAID with analgesic and anti-inflammatory properties (9). This medication belongs to the heterocyclic acetic acid family which induces analgesic and anti-inflammatory properties. It exerts its effects through the inhibition of the synthesis of prostaglandins by inhibiting cyclooxygenase. Similar to many NSAIDs, ketorolac is a non-selective COX inhibitor (2) which is used for the short-term management of moderate to severe postoperative pain. The most extended permissible duration of the use of ketorolac (in the form of tables) is five days, with two days for its injectable form (intravenous or intramuscular injection) (2). Previous studies have shown that intravenous injection of ketorolac 30 mg before surgery results in pain relief after impacted third molar surgeries (10). A study showed that the analgesic effect of ketorolac after surgery was higher than that of tramadol (11). However, the administration of these analgesic agents is associated with some complications. The use of NSAIDs is highly limited in patients with asthma, gastrointestinal problems, peptic ulcers, and coagulatory problems. Besides, reports are available on the incidence of hypersensitivity reactions in these patients (2,12-14).
Some studies have questioned the efficacy of the preoperative administration of ketorolac in pain relief after surgery. A study showed that the administration of ketorolac 30 mg before surgery did not relieve pain after orthopedic surgeries (15). However, some studies have reported no significant differences between administrating and not administrating ketorolac in the doses of narcotics prescribed postoperatively after impacted third molar surgeries (16). Moreover, no pain relief was reported after laparoscopic procedures when ketorolac was administrated preoperatively (17).
Pregabalin is an antiepileptic agent that was introduced in 2004 and is administrated to decrease epileptic attacks, resolve anxiety disorders, and relieve pain in patients with neuropathic disorders. Pregabalin is an analog of gamma-aminobutyric acid which has higher oral bioavailability and biocompatibility compared to gabapentin (18). Recent studies have shown that its preoperative administration decreases the dose of opioids prescribed and postoperative nausea and vomiting (3,19). One of the advantages of this medication is its effect on wound healing and the decrease of inflammation (20). Some studies have reported the efficacy of preoperative administration of oral pregabalin in decreasing postoperative pain after orthognathic (3), spinal (21), and abdominal surgeries as well as hysterectomy and myomectomy (22).
In contrast, some studies have reported that its preoperative administration in knee surgeries (23) and cosmetic procedures (24) was not effective. In addition to such discrepancies in the preoperative use of ketorolac and pregabalin in terms of postoperative pain relief, a search in scientific sources and databases, such as PubMed, Google Scholar, and Scopus, showed that no comprehensive study is available on the administration of injectable ketorolac and oral pregabalin in patients undergoing surgical procedures for maxillofacial fractures. Previous studies have advocated the use of pregabalin in comparison with the placebo in some surgical procedures. Therefore, the present study aimed to compare the analgesic effects of intravenous ketorolac and oral pregabalin in patients undergoing surgical procedures for mandibular fractures.
Materials and Methods
The present clinical trial was carried out from August 2019 to February 2020 in Imam Reza Educational and Treatment Center, Tabriz, Iran. A total of 60 patients with unilateral fractures of the body, angle, and symphysis of the mandible, who were indicated for open reduction using the intraoral approach, were selected using the random sampling technique and included in the study after signing an informed consent form.
Determining the Sample Size
The results of a study by Ahiskalioglu et al (3) were used to determine the sample size. To this end, the sample size was estimated to be 26 for each group, considering α=0.05 and a power of 80%. The sample size was increased by 10% to improve the accuracy, and 30 subjects were included in each group, totaling 60 subjects.
Inclusion Criteria
-
Willingness to be included in the study
-
Patients with a unilateral fracture of the body, angle, and symphysis of the mandible occurred within the previous 2 weeks
-
An age range of 20–60 years considering that such fractures are very common in this age range (25)
-
ASA I (healthy) and ASA II patients (mild systemic problems without functional limitations (26)
Exclusion Criteria
-
Surgery lasting for >2 hours due to a complicated procedure
-
Drug abuse
-
Psychopathic patients; all the patients taking psychotropic medicines were excluded due to their palliative effects
-
Allergic reactions to drugs
-
Systemic conditions that might be exacerbated by side effects of the drugs
-
A history of seizures and use of anticonvulsive agents
-
More than one incision site
-
Pregnancy and breastfeeding
-
Use of more than two plates
-
Edentulous patients due to the difference in surgical procedures such as Circum-mandibular wire
Description of Study Groups
The patients were randomly assigned to two groups by a person blinded to the study objectives using the RandList software. In group 1, a 30-mg dose of intravenous ketorolac (Caspian Pharmaceutical Co., Iran) was administered one hour before the induction of general anesthesia. In group 2, a 15-mg dose of oral Pregabalin (Jalinous Pharmaceutical Co., Iran) was administered one hour before the induction of general anesthesia. After surgery, the subjects in both groups received an intravenous dose of Apotel every 6 hours. After transferring each patient to the recovery room, and after the patient regained consciousness, the severity of pain was determined (baseline/hour 0) using VAS (visual analog scale). A checklist was submitted to each patient for the determination of the severity of pain using VAS. The patient was asked to rate their pain severity on a scale of 0 to 10. The pain scores were then determined at 2-, 4-, 6-, 8-, 12-, and 24-hour postoperative intervals (3).
Evaluation of the Study Outcomes
The postoperative pain relief constituted the primary outcome in this study. After the patients regained consciousness, the pain intensity was determined based on VAS for 48 hours at baseline (hour 0) and 2-, 4-, 6-, 12-, 24-hour postoperative intervals. The patients determined their pain severity as a number ranging from 0 (without pain) to 10 (excruciating pain). The mean pain score of each subject in both groups and at different time intervals was recorded and compared. After surgery, the physician prescribed intravenous Apotel 1 g every 6 hours and intravenous pethidine 25 mg upon patients’ requests (PRN). Finally, the total opioid dose (pethidine) for each patient was recorded in mg during the first 24 hours. Additionally, the time for the first request for analgesics was recorded in minutes, and the means of the groups were compared.
Before the study, each nurse was given the necessary instructions by the researcher on how to fill the checklist. The study procedures and the pain scoring technique were explained to the patients. All the patients completed the study, and none was excluded. The surgeon and nurses recording the prescribed doses of opioids and the first request for analgesics were blinded to the study procedures. All the surgeries were carried out by a team of maxillofacial surgeons.
Statistical Analysis
The data were analyzed using descriptive statistics (frequencies, percentages, means, and standard deviations), independent samples t test, chi-square test, and repeated measures ANOVA in SPSS 19.0. The normal distribution of data was evaluated using the Kolmogorov-Smirnov test. Statistical significance was defined as P < 0.05.
Results
In this study, 60 patients with a mean age of 36.21±9.36 years were evaluated (Table 1, Figure 1).
Table 1.
The Mean Age of the Subjects and the Frequencies (Percentages) of the Participants in Terms of Gender and Fracture Type
|
|
|
Group 1 (Ketorolac)
|
Group 2 (Pregabalin)
|
Total
|
P
Value
|
| Gender |
Female |
16 (53.3%) |
17 (56.7%) |
33 (55%) |
0.795 |
| Male |
14 (46.7%) |
13 (43.3%) |
27 (45%) |
|
Mean ± SD of age |
35.23±8.82 |
37.2±9.92 |
36.21±9.36 |
0.421 |
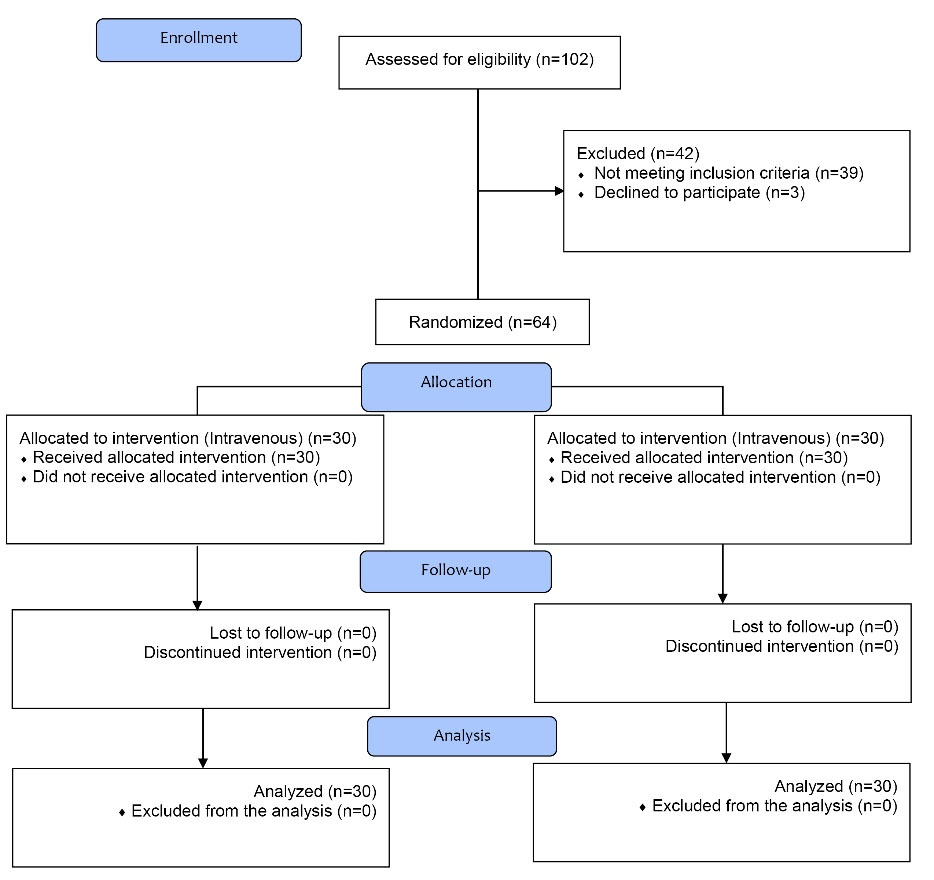
Figure 1.
The CONSORT Flow Diagram of Study.
.
The CONSORT Flow Diagram of Study.
The results of the chi-square test on the gender of the subjects and t test for independent groups on the mean age of subjects showed no significant differences between the two groups (P > 0.05). In other words, gender distribution and mean age were similar in the two groups.
Table 2 and Figure 2 present the mean scores of the pain severity in the study groups at different time intervals. As shown by the data, the pain severity was similar between the two groups preoperatively. After surgery, the pain was most severe immediately after the patients regained consciousness; however, it decreased gradually in two hours and increased in severity up to 6 hours postoperatively, reaching the maximum pain intensity. Then, the pain severity decreased up to 24 hours postoperatively. Repeated measures of ANOVA showed that these variations in pain severity were statistically significant (P < 0.0001). T-test for independent groups was used for two-by-two comparisons of the different time intervals in terms of the pain severity, with the results presented in Table 2.
Table 2.
The Means and Standard Deviations of Pain Severity Scores at Different Time Intervals of the Study
|
Intervals
|
Study Groups
|
Mean
|
SD
|
95% Confidence Interval for Mean
|
Min
|
Max
|
P
Value
*
|
|
Lower Bound
|
Upper Bound
|
| 2 hours before surgery |
Ketorolac |
1.6000 |
0.67466 |
0.12318 |
1.3481 |
1.8519 |
1.00 |
0.842 |
| Pregabalin |
1.6333 |
0.61495 |
0.11227 |
1.4037 |
1.8630 |
1.00 |
| Total |
1.6167 |
0.64022 |
0.08265 |
1.4513 |
1.7821 |
1.00 |
| Immediately after regaining consciousness |
Ketorolac |
3.9667 |
0.85029 |
3.6492 |
4.2842 |
3.00 |
5.00 |
0.000 |
| Pregabalin |
3.1000 |
0.88474 |
2.7696 |
3.4304 |
2.00 |
5.00 |
| Total |
3.5333 |
0.96492 |
3.2841 |
3.7826 |
2.00 |
5.00 |
| 2 hours later |
Ketorolac |
2.1333 |
0.97320 |
1.7699 |
2.4967 |
1.00 |
4.00 |
0.414 |
| Pregabalin |
1.9333 |
0.90719 |
1.5946 |
2.2721 |
0.00 |
4.00 |
| Total |
2.0333 |
0.93820 |
1.7910 |
2.2757 |
0.00 |
4.00 |
| 4 hours later |
Ketorolac |
3.3667 |
0.96431 |
3.0066 |
3.7267 |
2.00 |
5.00 |
0.697 |
| Pregabalin |
3.2667 |
1.01483 |
2.8877 |
3.6456 |
1.00 |
5.00 |
| Total |
3.3167 |
0.98276 |
3.0628 |
3.5705 |
1.00 |
5.00 |
| 6 hours later |
Ketorolac |
3.9333 |
0.86834 |
3.6091 |
4.2576 |
1.00 |
5.00 |
0.470 |
| Pregabalin |
3.7333 |
1.22990 |
3.2741 |
4.1926 |
1.00 |
6.00 |
| Total |
3.8333 |
1.06033 |
3.5594 |
4.1072 |
1.00 |
6.00 |
| 12 hours later |
Ketorolac |
0.1667 |
0.37905 |
0.0251 |
0.3082 |
0.00 |
1.00 |
0.527 |
| Pregabalin |
0.2333 |
0.43018 |
0.0727 |
0.3940 |
0.00 |
1.00 |
| Total |
0.2000 |
0.40338 |
0.0958 |
0.3042 |
0.00 |
1.00 |
| 24 hours later |
Ketorolac |
0.1333 |
0.34575 |
0.0042 |
0.2624 |
0.00 |
1.00 |
0.694 |
| Pregabalin |
0.1000 |
0.30513 |
0.0139 |
0.2139 |
0.00 |
1.00 |
| Total |
0.1167 |
0.32373 |
0.0330 |
0.2003 |
0.00 |
1.00 |
| Total 24-hour score |
Ketorolac |
2.2833 |
0.36919 |
2.1455 |
2.4212 |
1.50 |
3.17 |
0.035 |
| Pregabalin |
2.0611 |
0.42769 |
1.9014 |
2.2208 |
1.17 |
3.00 |
| Total |
2.1722 |
0.41166 |
2.0659 |
2.2786 |
1.17 |
3.17 |
*Independent samples ttest
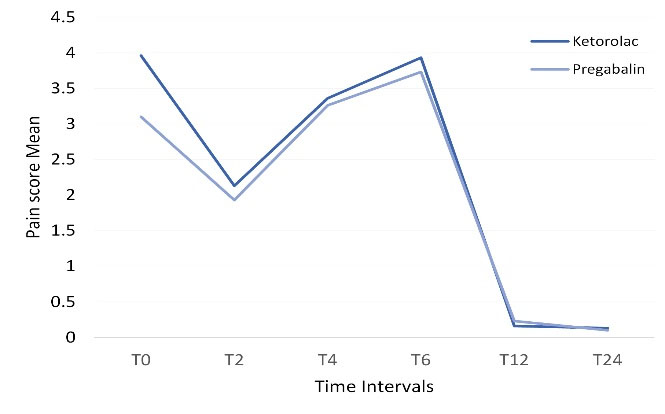
Figure 2.
The Linear Graph of Pain Severity in the Study Groups.
.
The Linear Graph of Pain Severity in the Study Groups.
Student’s t test for independent groups was used to evaluate the effect of medication type on the mean pain severity at each time interval of the study. This test showed that the mean pain severity in the pregabalin group immediately after regaining consciousness was lower compared to the ketorolac group (P < 0.0001). At other time intervals, the pain severity was similar in the two groups. The mean 24-hour pain score was lower in the pregabalin group than in the ketorolac group (P < 0.05).
Table 3 presents the doses of the opioid prescribed during the 24-hour period after surgery and the time of the first request for an opioid separately in each group. The results showed that the dose of the opioid used in the ketorolac group was slightly higher, and the time for requesting an opioid dose was shorter compared to the pregabalin group. However, the independent samples t-test showed that this finding was not statistically significant (P > 0.05).
Table 3.
The Mean Doses of the Opioid Agent Used (in mg) and the Time for Requesting the First Dose of the Opioid Agent (in Minutes) in the Study Groups
|
|
Group
|
Min
|
Max
|
Mean ± SD
|
P
value
|
| The mean doses of the opioid prescribed |
Ketorolac |
0 |
50 |
34.16±13.9 |
0.152 |
| Pregabalin |
0 |
50 |
28.33±17.06 |
| The time of request for the first dose of the opioid |
Ketorolac |
30 |
75 |
45.51±12.34 |
0.338 |
| Pregabalin |
30 |
75 |
48.60±10.85 |
Discussion
Pain is an unpleasant feeling due to tissue destruction. One of the major concerns in patients is the postoperative pain because millions of cells are destroyed during surgery, inducing pain due to the inflammatory process and the release of chemical mediators of pain perception (1,2). The analgesic efficacy after surgery gives rise to an increase in patient satisfaction, a decrease in hospitalization duration, and a decrease in patient costs (3,27).
Preemptive analgesia is one of the techniques to manage pain after surgery, in which the administration of analgesic agents is undertaken before an encounter with the pain stimulus. Clonidine, ketorolac, ibuprofen, gabapentin, and pregabalin are systemic medications used in this technique (3). The results of the present study showed that the highest mean scores of the pain severity of the patients were reported immediately after regaining consciousness. However, the pain was less severe in the pregabalin group than in the ketorolac group, indicating that pregabalin was more effective in relieving postoperative pain than ketorolac. Two hours after regaining consciousness, the severity of pain decreased in both groups. To justify this, we should consider that approximately 45 minutes after regaining consciousness in both groups, the patients requested an analgesic agent. Then, pethidine 25 mg was administered intravenously to each patient. Although the mean dose of the analgesic agent prescribed in the pregabalin group was lower compared to the ketorolac group, the difference was not significant. Four and six hours after regaining consciousness and after the analgesic effect of the injected pethidine wore off, the pain increased in severity, reaching the maximum pain intensity 6 hours after regaining consciousness. Over time and after the intravenous injection of 1-g Apotel (analgesic agent) every 6 hours, the severity of pain decreased 12 and 24 hours after regaining consciousness, reaching the minimum pain intensity. Finally, the 24-hour mean pain score in the pregabalin group was lower than that in the ketorolac group.
Ahishkalioglu et al (3) assigned 40 patients who were candidates for bimaxillary orthognathic surgery to two equal groups. In group 1, pregabalin 150 mg was prescribed one hour before the bimaxillary orthognathic surgery, and in group 2, a placebo was administered. The results showed that the preoperative administration of pregabalin decreased preoperative pain and the need for opioid analgesics after surgery compared to the placebo, which is consistent with the results of the present study. However, in the present study, the patients in the other group received intravenous ketorolac instead of a placebo.
Sagit et al (28) assigned 143 patients who were candidates for septoplasty procedure to three groups. In group 1, pregabalin 75 mg and in group 2, pregabalin 150 mg were administered one hour before the surgical procedure orally. The results showed that preoperative administration of pregabalin decreased postoperative pain severity and the need for the prescription of analgesic agents compared to the control group (the third group). Besides, the mean 24-hour pain scores in groups 1 and 2 were lower compared to the control group, which is consistent with the present study.
Cillo and Dattilo (29) assigned 12 patients who were candidates for maxillomandibular advancement to treat sleep apnea to two groups. In group 1, pregabalin 150 mg was prescribed in combination with celecoxib 400 mg, and in group 2, a placebo was administered one hour preoperatively. The results showed that the severity of pain and the need for the use of opioid analgesics postoperatively were lower in the case group than in the control group. Although the sample size in that study was small and celecoxib was administered in combination with pregabalin, the results were consistent with the present study.
In spinal surgeries (21), abdominal hysterectomy, and myomectomy (22), preoperative administration of pregabalin has also been reported to be effective in decreasing postoperative pain.
Previous studies have shown that oral pregabalin is adsorbed rapidly, reaching its maximum plasma concentration in 80 minutes. Its bioavailability is approximately 90%, and its 150-mg dose has been recommended (3,30). In addition to analgesic effects, preoperative administration of pregabalin decreases the use of opioids, nausea, and vomiting postoperatively (3,19). Furthermore, it helps the wound healing process and decreases inflammation (20). On the other hand, the use of NSAIDs, such as ketorolac, in patients with asthma, gastrointestinal problems, peptic ulcers, and coagulatory problems is strictly limited. In addition, reports are available on the incidence of hypersensitivity reactions after using NSAIDs (2,12-14). Therefore, considering: (1) the advantages of pregabalin and the results of the present study, (2) the disadvantages of ketorolac, and (3) similarity of the half-life of pregabalin (5-6.5 hours) (31) and ketorolac (4-6 hours) (32), it appears that the preoperative administration of pregabalin is more useful than ketorolac to decrease postoperative pain. However, in some studies, the preemptive use of pregabalin did not significantly decrease patients’ postoperative pain after knee (23) and cosmetic surgeries (24). Therefore, further studies are necessary to substantiate these findings, considering limitations of the present study.
Limitations and Suggestions
There was no control group in the present study. Therefore, an accurate and valid comparison was a real challenge, especially in terms of the amount of the opioid analgesics prescribed and the duration of the pain relief induced separately for each analgesic agent. Although one maxillofacial surgeon carried out all the surgeries, it was not possible to provide similar conditions for all the patients, including the duration of surgery, the trauma inflicted on the surgical site during surgery, the type of fracture, and the psychological conditions of the patients, which might have affected the results of the study. On the other hand, blinding was not possible for patients because some received capsules, and some received injections. Another limitation of the present study was the small sample size. It is suggested that larger sample sizes should be evaluated. The administration of pregabalin and ketorolac at different doses compared to the placebo might lead to more valid results. Besides, in the present study, only the intravenous form of ketorolac was used, whereas some studies have reported that its intramuscular administration is more effective.
Conclusions
The oral administration of pregabalin 150 mg, one hour preoperatively, was more effective than the intravenous administration of ketorolac 30 mg in relieving postoperative pain.
Conflict of Interest Disclosures
The authors declare no competing interest.
Acknowledgments
The authors would like to thank all the staff of Tabriz University of Medical Sciences, who contributed to this study.
Ethical Statement
All the patients underwent routine diagnostic procedures and treatment planning, and none was deprived of care. The Ethics Committee of Tabriz University of Medical Sciences approved all the ethical aspects of this study (IR.TBZMED.REC.1396.1270). The study was registered in the Iranian Clinical Trial Registration Center (identifier: IRCT20150628022951N10; https://www.irct.ir/trial/40840). Before the study, an informed consent form was prepared and explained to the subjects so that those with reading problems would understand it.
Authors’ Contribution
JY and MG were responsible for the design and concept of the study as well as the revision of the prepared manuscript. MG, JY, and SN analyzed the data, carried out the literature search and drafted the manuscript. AM, FF, and MG performed clinical evaluations. All the authors have read and approved the final manuscript.
Funding
The study was self-funded by the authors and their institution.
References
- Shoar S, Esmaeili S, Safari S. Pain management after surgery: a brief review. Anesth Pain Med 2012; 1(3):184-6. doi: 10.5812/kowsar.22287523.3443 [Crossref] [ Google Scholar]
- Shankariah M, Mishra M, Kamath RA. Tramadol versus ketorolac in the treatment of postoperative pain following maxillofacial surgery. J Maxillofac Oral Surg 2012; 11(3):264-70. doi: 10.1007/s12663-011-0321-y [Crossref] [ Google Scholar]
- Ahiskalioglu A, İnce İ, Aksoy M, Yalcin E, Ahiskalioglu EO, Kilinc A. Effects of a single-dose of pre-emptive pregabalin on postoperative pain and opioid consumption after double-jaw surgery: a randomized controlled trial. J Oral Maxillofac Surg 2016; 74(1):53.e1-7. doi: 10.1016/j.joms.2015.09.008 [Crossref] [ Google Scholar]
- Farhadi F, Eslami H, Majidi A, Fakhrzadeh V, Ghanizadeh M, Khadem Neghad S. Evaluation of adjunctive effect of low-level laser therapy on pain, swelling and trismus after surgical removal of impacted lower third molar: a double blind randomized clinical trial. Laser Ther 2017; 26(3):181-7. doi: 10.5978/islsm.17-OR-13 [Crossref] [ Google Scholar]
- Kashefimehr A, Babaloo A, Ghanizadeh M, Ghasemi SH, Mollazadeh H. Effect of prophylactic administration of Novafen for periodontal surgery on postoperative pain relief. J Med Life 2017; 10(2):127-30. [ Google Scholar]
- Nezafati S, Khorshidi Khiavi R, Mirinejhad SS, Aghamohammadi D, Ghanizadeh M. Comparison of pain relief from different intravenous doses of ketorolac after reduction of mandibular fractures. J Clin Diagn Res 2017; 11(9):PC06-PC10. doi: 10.7860/jcdr/2017/30946.10558 [Crossref] [ Google Scholar]
- Yazdani J, Khorshidi Khiavi R, Nezafati S, Mortazavi A, Farhadi F, Nojan F. Comparison of analgesic effects of intravenous and intranasal ketorolac in patients with mandibular fracture-a randomized clinical trial. J Clin Exp Dent 2019; 11(9):e768-e75. doi: 10.4317/jced.55753 [Crossref] [ Google Scholar]
- Allen SC, Ravindran D. Perioperative use of nonsteroidal anti-inflammatory drugs: results of a UK regional audit. Clin Drug Investig 2009; 29(11):703-11. doi: 10.2165/11319610-000000000-00000 [Crossref] [ Google Scholar]
- De Oliveira GS Jr, Agarwal D, Benzon HT. Perioperative single dose ketorolac to prevent postoperative pain: a meta-analysis of randomized trials. Anesth Analg 2012; 114(2):424-33. doi: 10.1213/ANE.0b013e3182334d68 [Crossref] [ Google Scholar]
- Ong KS, Seymour RA, Chen FG, Ho VC. Preoperative ketorolac has a preemptive effect for postoperative third molar surgical pain. Int J Oral Maxillofac Surg 2004; 33(8):771-6. doi: 10.1016/j.ijom.2004.01.020 [Crossref] [ Google Scholar]
- Gopalraju P, Lalitha RM, Prasad K, Ranganath K. Comparative study of intravenous Tramadol versus Ketorolac for preventing postoperative pain after third molar surgery--a prospective randomized study. J Craniomaxillofac Surg 2014; 42(5):629-33. doi: 10.1016/j.jcms.2013.09.004 [Crossref] [ Google Scholar]
- Stevenson DD, Szczeklik A. Clinical and pathologic perspectives on aspirin sensitivity and asthma. J Allergy Clin Immunol 2006; 118(4):773-86. doi: 10.1016/j.jaci.2006.07.024 [Crossref] [ Google Scholar]
- Cawthorn TR, Phelan R, Davidson JS, Turner KE. Retrospective analysis of perioperative ketorolac and postoperative bleeding in reduction mammoplasty. Can J Anaesth 2012; 59(5):466-72. doi: 10.1007/s12630-012-9682-z [Crossref] [ Google Scholar]
- Kotagal M, Hakkarainen TW, Simianu VV, Beck SJ, Alfonso-Cristancho R, Flum DR. Ketorolac use and postoperative complications in gastrointestinal surgery. Ann Surg 2016; 263(1):71-5. doi: 10.1097/sla.0000000000001260 [Crossref] [ Google Scholar]
- Vanlersberghe C, Lauwers MH, Camu F. Preoperative ketorolac administration has no preemptive analgesic effect for minor orthopaedic surgery. Acta Anaesthesiol Scand 1996; 40(8 Pt 1):948-52. doi: 10.1111/j.1399-6576.1996.tb04565.x [Crossref] [ Google Scholar]
- Gutta R, Koehn CR, James LE. Does ketorolac have a preemptive analgesic effect? a randomized, double-blind, control study. J Oral Maxillofac Surg 2013; 71(12):2029-34. doi: 10.1016/j.joms.2013.06.220 [Crossref] [ Google Scholar]
- Cabell CA. Does ketorolac produce preemptive analgesic effects in laparoscopic ambulatory surgery patients?. AANA J 2000; 68(4):343-9. [ Google Scholar]
- Bockbrader HN, Wesche D, Miller R, Chapel S, Janiczek N, Burger P. A comparison of the pharmacokinetics and pharmacodynamics of pregabalin and gabapentin. Clin Pharmacokinet 2010; 49(10):661-9. doi: 10.2165/11536200-000000000-00000 [Crossref] [ Google Scholar]
- Engelman E, Cateloy F. Efficacy and safety of perioperative pregabalin for post-operative pain: a meta-analysis of randomized-controlled trials. Acta Anaesthesiol Scand 2011; 55(8):927-43. doi: 10.1111/j.1399-6576.2011.02471.x [Crossref] [ Google Scholar]
- Sarıtaş TB, Korkmaz M, Sevimli A, Sarıtaş ZK. Comparison of the effects of gabapentin and pregabalin on wound healing in rats. Int Wound J 2016; 13(5):748-53. doi: 10.1111/iwj.12364 [Crossref] [ Google Scholar]
- Gianesello L, Pavoni V, Barboni E, Galeotti I, Nella A. Perioperative pregabalin for postoperative pain control and quality of life after major spinal surgery. J Neurosurg Anesthesiol 2012; 24(2):121-6. doi: 10.1097/ANA.0b013e31823a885b [Crossref] [ Google Scholar]
- Fassoulaki A, Melemeni A, Tsaroucha A, Paraskeva A. Perioperative pregabalin for acute and chronic pain after abdominal hysterectomy or myomectomy: a randomised controlled trial. Eur J Anaesthesiol 2012; 29(11):531-6. doi: 10.1097/EJA.0b013e32835800e0 [Crossref] [ Google Scholar]
- Yadeau JT, Paroli L, Kahn RL, Jules-Elysee KM, Lasala VR, Liu SS. Addition of pregabalin to multimodal analgesic therapy following ankle surgery: a randomized double-blind, placebo-controlled trial. Reg Anesth Pain Med 2012; 37(3):302-7. doi: 10.1097/AAP.0b013e31824c6846 [Crossref] [ Google Scholar]
- Chaparro LE, Clarke H, Valdes PA, Mira M, Duque L, Mitsakakis N. Adding pregabalin to a multimodal analgesic regimen does not reduce pain scores following cosmetic surgery: a randomized trial. J Anesth 2012; 26(6):829-35. doi: 10.1007/s00540-012-1447-x [Crossref] [ Google Scholar]
- Agarwal A, Gautam S, Gupta D, Agarwal S, Singh PK, Singh U. Evaluation of a single preoperative dose of pregabalin for attenuation of postoperative pain after laparoscopic cholecystectomy. Br J Anaesth 2008; 101(5):700-4. doi: 10.1093/bja/aen244 [Crossref] [ Google Scholar]
- Akhtar MI, Saleem M, Zaheer J. Wound infiltration with Bupivacaine versus Ketorolac for postoperative pain relief in minor to moderate surgeries. J Pak Med Assoc 2009; 59(6):385-8. [ Google Scholar]
- Wu CL, Raja SN. Treatment of acute postoperative pain. Lancet 2011; 377(9784):2215-25. doi: 10.1016/s0140-6736(11)60245-6 [Crossref] [ Google Scholar]
- Sagit M, Yalcin S, Polat H, Korkmaz F, Cetinkaya S, Somdas MA. Efficacy of a single preoperative dose of pregabalin for postoperative pain after septoplasty. J Craniofac Surg 2013; 24(2):373-5. doi: 10.1097/SCS.0b013e31827fece5 [Crossref] [ Google Scholar]
- Cillo JE Jr, Dattilo DJ. Pre-emptive analgesia with pregabalin and celecoxib decreases postsurgical pain following maxillomandibular advancement surgery: a randomized controlled clinical trial. J Oral Maxillofac Surg 2014; 72(10):1909-14. doi: 10.1016/j.joms.2014.05.014 [Crossref] [ Google Scholar]
- Ahn S, Byun SH, Park K, Ha JL, Kwon B, Kim JC. Analgesic efficacy of preemptive pregabalin administration in arthroscopic shoulder surgery: a randomized controlled trial. Can J Anaesth 2016; 63(3):283-9. doi: 10.1007/s12630-015-0510-0 [Crossref] [ Google Scholar]
- Ghumman SA, Bashir S, Noreen S, Khan AM, Malik MZ. Taro-corms mucilage-alginate microspheres for the sustained release of pregabalin: in vitro & in vivo evaluation. Int J Biol Macromol 2019; 139:1191-202. doi: 10.1016/j.ijbiomac.2019.08.100 [Crossref] [ Google Scholar]
- Ali AA, Sayed OM. Development and characterization of ketorolac tromethamine osmotic pump tablets. J Drug Deliv Sci Technol 2013; 23(3):275-81. doi: 10.1016/s1773-2247(13)50041-4 [Crossref] [ Google Scholar]