Avicenna J Dent Res. 12(2):46-50.
doi: 10.34172/ajdr.2020.10
Original Article
Laboratory Evaluation of Torque Loss in Titanium, One-Piece and Two-Piece Zirconia Abutments Under Cyclic Loading
Hamed Amraei 1  , Bijan Heidari 2, Sara Khazaei 3, Payam Amini 4, Farnaz Firouz 3, *
, Bijan Heidari 2, Sara Khazaei 3, Payam Amini 4, Farnaz Firouz 3, * 
Author information:
1Assistant Professor, Department of Prosthodontics, Dental Research Center, Faculty of Dentistry, Lorestan University of Medical Sciences, Lorestan, Iran.
2Assistant Professor, Prosthodontist, Tehran, Iran.
3Assistant Professor, Department of Prosthodontics, Dental Research Center, Faculty of Dentistry, Hamadan University of Medical Sciences, Hamadan, Iran.
4Assistant Professor, Department of Biostatistics and Epidemiology, School of public health, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
Abstract
Background: Screw loosening is one of the most common problems associated with implant-supported prostheses. The type and material of the abutment play an important role in the esthetic appearance of implant-supported restorations. Metal abutments create an unaesthetic grayish halo in the gingival margin of the implant due to the reflection of light from the surface of titanium abutment. Zirconia is highly popular for the fabrication of abutments due to its optimal color, along with the quality of light transmission and its resistance. The present study aimed to evaluate the torque loss in titanium and one- and two-piece zirconia abutments under cyclic loading.
Methods: In general, 24 abutments in three groups (n=8) of one- and two-piece zirconia abutments, and titanium abutments were evaluated in this experimental study. The abutments were attached to the analog of fixtures with 30 N/cm torque and the samples were subjected to loads applied to the center of abutments at 30° angle. After cyclic loading, the removal torque value was measured for each abutment and its numerical mean was calculated as well. Finally, the groups were compared using SPSS16 via ANOVA and Games-Howell tests at a 0.05 level of significance.
Results: The mean removal torque value was 23.925, 23.913, and 22.538 N/cm in titanium and two- and one-piece zirconia abutments, respectively, with no statistically significant difference in between (P>0.05).
Conclusions: The highest mean removal torque value belonged to prefabricated titanium abutments while the lowest value was related to one-piece zirconia abutments.
Keywords: Zirconia abutment, Torque loss, Cyclic loading, Titanium abutment
Copyright and License Information
© 2020 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Citation: Amraei H, Heidari B, Khazaei S, Amini P, Firouz F. Laboratory evaluation of torque loss in titanium, one-piece and two-piece zirconia abutments under cyclic loading. Avicenna J Dent Res. 2020;12(2):46-50. doi: 10.34172/ajdr.2020.10.
Background
Highlights
-
Our findings showed that the highest mean removal torque value belonged to prefabricated titanium abutments
-
Our findings showed that the lowest mean removal torque value was related to one-piece zirconia abutments
The increasing use of dental implants and the high success rate of osseointegration have triggered attempts to respond to patient needs for designing and fabricating high-quality restorations such as full-ceramic abutments and crowns (1,2). Ceramic abutments have gained increasing popularity due to optimal properties such as favorable color match, optimal texture, no toxicity, and biocompatibility (3).
The type and material of the abutment play an important role in the esthetic appearance of implant-supported restorations. Metal abutments create an unaesthetic grayish halo in the gingival margin of the implant due to the reflection of light from the surface of the titanium abutment. Alumina and zirconia are highly popular for the fabrication of abutments due to their optimal color, the quality of light transmission, and their resistance. In addition, alumina abutments that support single-unit crowns have 90%-100% durability in anterior and premolar areas. Zirconia abutments supporting single-unit crowns in anterior and premolar regions have shown 100% durability (4). Recently, the use of zirconia abutments has increased due to their higher resistance compared to alumina and other types of available ceramics, as well as the aforementioned advantages. The zirconium oxide products have high resistance and long durability. They further have the highest level of esthetics and biocompatibility, and no report is available regarding allergic reactions to these materials. Thus, they are suitable for use in patients who are allergic to alloys (5).
Two-piece zirconia abutments consist of a metal framework with a ceramic portion on the top. The full-ceramic portion of zirconia is designed with the computer-aided design/computer-aided manufacturing (CAD/CAM) technique. Following air abrasion, the full-ceramic portion is bonded to the metal framework using the resin cement. Components are typically bonded by a technician in a laboratory. Evidence shows that two-piece zirconia abutments are stronger than one-piece abutments (5). In one-piece abutments, all parts are made of zirconia and connected to the implant by a metal screw. This type of abutment is designed and manufactured by the CAD/CAM system.
Despite all the favorable characteristics of these abutments, the precision of their machining and alignment remains questionable. Ceramic abutments have limitations as well. For instance, the metal-ceramic interface is prone to wear. Moreover, the degradation of the implant-abutment contact between the external connection and the zirconia abutment can decrease mechanical properties and compromise the fit between the implant and abutment (1). On the other hand, the optimal fit between the fixture and its components is an important factor in stress transmission and the biological response of the host tissue around the implant, and the occurrence of mechanical problems in implant restoration. Some studies have shown that full-ceramic abutments cannot be designed as precise as metal abutments; therefore, the mismatch can cause mechanical problems such as screw loosening or biological problems including bone resorption due to microbial accumulations (6). Any mismatch at the implant-abutment interface can eventually result in torque loss and abutment screw loosening (7).
The screw stretches along its length upon torque application. The screw tension is called the “preload”. Because of its elastic properties, the screw tends to return to its normal state, creating a force that holds the abutment and implant together. Screw loosening occurs when forces tending to separate the pieces exceed the forces that keep them together, as well as the preload inside the screw (8,9). The abutment screw loosening is one of the most common post-treatment complications in implant-supported restorations (7). Theoretically, the external hex connection type is susceptible to loosening while the abutment screw must withstand the loads. On the other hand, the internal hex connection distributes the load at the fixture level, which decreases the risk of screw loosening (10). Therefore, most implants are recently used with internal hex abutments. Nowadays, with the use of internal hex abutments and abutment-implant coupling mechanism, some mechanical problems (e.g., screw loosening) may occur when applying excessive occlusal loads. This occurs due to creeping at the abutment-implant interface (11). Therefore, the present study used internal hex zirconia abutments and aimed to evaluate the screw loosening of one- and two-piece zirconia abutments under the force of fatigue or cyclic loading.
Materials and Methods
In general, 24 analogs of fixtures with internal taper hexagon were used in this in vitro experimental study. The fixtures were divided into 3 groups (n=8) for the use of one- and two-piece zirconia abetments and prefabricated titanium abutments. The sample size for each group was calculated based on a similar study (9), assuming an alpha level of 5% and the statistical power of 0.95.
Three groups of abutments (n=8) were used, including one-piece zirconia abutments, two-piece zirconia abutments with metal connection, and prefabricated titanium abutments (Figure 1). One- and two-piece zirconia abutments with the same dimensions and characteristics of the prefabricated titanium abutments (i.e., 11-degree taper, Ø 4.5 mm * 5.5 mm L, DIO UF, Korea) were designed using the CAD/CAM technology (ARUM 5X-200).

Figure 1.
Study Groups Including Two-Piece Zirconia (Left), Titanium (Middle), And One-Piece Zirconia (Right).
.
Study Groups Including Two-Piece Zirconia (Left), Titanium (Middle), And One-Piece Zirconia (Right).
Each fixture analog was mounted in a cylindrical mold fabricated from the brass and measured 20 mm in height and 25 mm in diameter. The upper surfaces of the mold were cut so that this surface had a 30° angle relative to the horizontal plane. A hole perpendicular to the surface was drilled in the upper surface (the inclined surface) of the mold for the fixture analog (Figure 2). This design allowed the fatigue tester to apply force at a 30° angle relative to the longitudinal axis of the abutment.
A surveyor was used to mount the analogs in the hole created in the mold perpendicular to the inclined surface. A hand-made wooden jig was used for the correct positioning of the mold on the surveyor. This jig, in fact, was a ramp with a 60° angle relative to the horizontal plane. A hole was created perpendicular to the surface for the accurate placement of the brass mold (Figure 3). Therefore, by assembling the mold on the jig, the upper surface of the mold was positioned parallel to the horizon. Next, analogs were placed inside the hole filled with auto-polymerizing acrylic resin in the dough phase using a survivor.
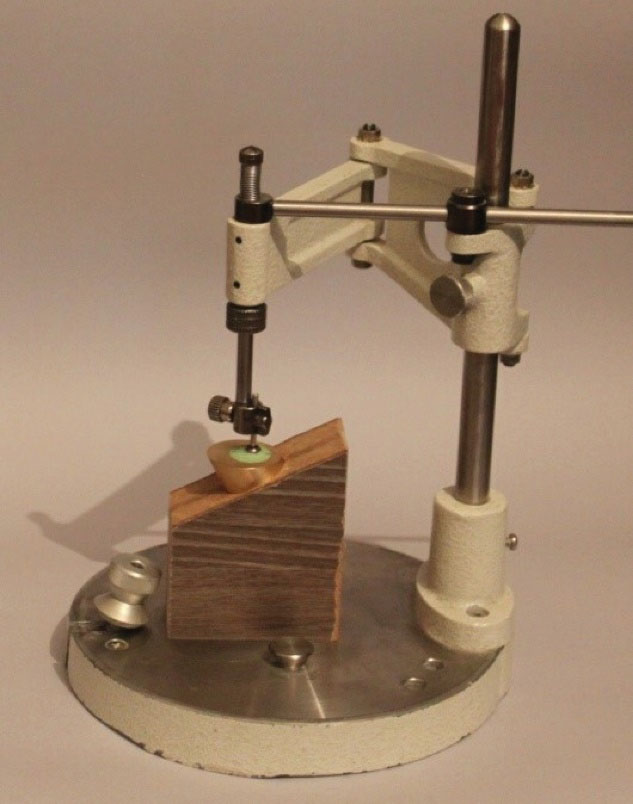
Figure 3.
Analog Positioning in Brass Mold Using a Surveyor.
.
Analog Positioning in Brass Mold Using a Surveyor.
After the placement of analogs, abutments were connected to the analogs with a 30 N/cm torque. A digital torque meter (TQ-8800, Lurton electronic, Taiwan) with an accuracy of 0.1 N/cm was used to calculate the tightening and removal torques, and then was attached to the upper part of the torque delivery device (Sao Paulo, SP, Brazil) and the cylinder-analog-abutment assembly was fixed at the bottom of the device (12).
After 10 minutes, the abutments were retightened with the same torque to compensate for the preload loss due to the settling effect of the interface. The torque level was precisely calculated as well.
To simulate the oral environment, first, the samples were thermo cycled (TC/300, Vafaei Industrial Factory, Iran), then each mold-analog-abutment assembly was mounted and fixed to the fatigue testing machine (CS-4, SDM mechatronic, Germany) as a chewing simulator.
Before starting each test, the fatigue tester was calibrated such that lever arms applied 120 000 load cycles at 1 Hz (60 rpm) frequency and 100±5 N force at 30° angle relative to the longitudinal axis of the abutment. At the end of each test, the samples were transferred to the base of the torque delivery device, and the removal torque value was measured and recorded as well. The following formula was used to calculate the percentage of torque loss (per tl):
The data were analyzed using SPSS (version 21) and compared by ANOVA at the 0.05 level of significance.
Results
In our study, none of the tested samples showed abutment or screw fracture. Table 1 presents the mean and standard deviation of per tl in all study groups.
Table 1.
Mean and Standard Deviation of Per tl for All Groups (n=8)
|
Groups
|
N
|
Mean ± Standard Deviation
|
| Titanium abutment |
8 |
20.24±6.02 |
| One-piece zirconia abutment |
8 |
24.87±7.92 |
| Two-piece zirconia abutment |
8 |
20.62±2.59 |
All abutments in the 3 groups demonstrated a reduction in the removal torque value compared to the insertion torque. The titanium abutment group represented the lowest torque loss. Conversely, the highest torque loss was observed in the one-piece zirconia abutment group. However, there was no statistically significant difference between these groups in this regard (Table 2).
Table 2.
Comparison of the Groups Using ANOVA
|
|
Sum of Square
|
df
|
Mean Square
|
F
|
P
Value
|
| Between groups |
85.015 |
5 |
16.6 |
0.194 |
0.939 |
| Inter groups |
170.94 |
2 |
85.472 |
|
|
| Total |
253.95 |
7 |
|
|
|
Note. ANOVA: Analysis of variance.
Discussion
The use of zirconium dioxide in implant abutments has recently increased due to its higher resistance compared to alumina and other dental ceramics (12). These abutments have met the required international standards. Gehrke et al investigated the effect of cyclic loading on the screw loosening of zirconia abutments and found that zirconium oxide was suitable for the fabrication of abutments, and the fabricated abutments met the international standards (13).
Several factors can cause screw loosening. For example, Binon showed that the risk of mechanical problems such as screw loosening was higher in poorly-fitted abutments (14). Additionally, Byrne et al studied the fit of prefabricated abutments and concluded that the adaptation and contact area of prefabricated abutments and the implant platform were significantly better than those in cast abutments, and this better fit decreased the frequency of mechanical problems such as screw loosening (15).
Similarly, Alikhasi et al evaluated the rate of torque loss in MAD/MAM zirconia and prefabricated titanium abutments and found no difference between the detorque level of MAD/MAM ceramic and titanium abutments (16), which is consistent with the results of the present study. It should be noted that the manufacturing process of the samples in their study differed from that of the present study. Other studies also reported similar results in this respect. For instance, Tsumita et al examined the effect of fatigue loading on the screw joint durability of zirconia abutments and concluded that zirconia abutments had similar durability to titanium abutments (17), which is in line with our findings.
Some other studies evaluated the screw loosening of zirconia abutments. For example, Nguyen et al investigated the effect of fatigue on ceramic abutments and found that the cyclic loading of zirconia abutments relied on the abutment diameter while the type of failure in these abutments was based on their design and system (18). The current study did not examine these parameters, and the samples had similar diameters and systems thus our results could not be compared with those of the above-mentioned study.
Some other studies also compared screw loosening in one- and two-piece zirconia abutments. For example, Ghanbarzadeh et al examined and compared screw loosening in one- and two-piece zirconia abutments (19) and observed no significant difference in this regard between one- and two-piece abutments, which corroborates with our findings.
In the present study, no statistically significant difference was found between zirconia and titanium abutments. In contrast, Cid et al evaluated screw loosening in titanium and zirconia abutments (20) and reported that titanium abutments had higher resistance to screw loosening. In our study, although titanium abutments were more resistant, this difference was not statistically significant, which could be due to the differences in the design and manufacturing process of abutments in the two studies.
In another study, Gehrke et al investigated the fatigue and fracture of two- and one-piece zirconia abutments subjected to cyclic loading and thermal cycling. Two-piece zirconia abutments had higher fracture and fatigue resistance compared to one-piece zirconia abutments (12). The results of Michael et al are quite consistent with those of the present study, although, in their study, the applied force was higher than that of the present study (100 ± 5). Their results are in line with ours although the methodology of the two studies was different. Despite the observation of similar results of the current study, differences in the methods as well as the lack of the effect of the number of samples and the amount of the applied force on the results are considered the strengths of the study.
Another study also discussed that titanium-titanium interface in two-piece zirconia abutment implants is superior to the zirconia-titanium interface in one-piece zirconia abutments, which somehow justifies the results of the present study regarding the higher mean value of removal torque in two-piece compared to one-piece zirconia abutments (21).
According to Brodbeck significant abrasion was observed in zirconia and alumina ceramic hex in comparison with the metal hex (22). These findings explain the results of the present study regarding higher mean values of removal torque in prefabricated abutments compared to two-piece zirconia abutments. Moreover, full-ceramic one-piece zirconia abutments are not made as precisely as metal abutments. Recent studies have represented that one-piece zirconia abutments have marginal misalignments with implants that may cause the screw loosening and micromotion of an implant-abutment interface, which can cause abrasion. In addition, a large marginal gap enhances bacterial colonization (22-24). This explains the difference in the marginal fit of prefabricated abutments compared to CAD/CAM manufactured abutments. For example, Hamilton stated that CAD/CAM abutments had lower marginal fit compared to prefabricated abutments although this difference was not statistically significant (25).
Conclusions
In general, the highest mean removal torque belonged to prefabricated titanium abutments while the lowest value was noted in one-piece zirconia abutments. However, there was no statistically significant difference between these two groups in this regard.
Conflict of Interest Disclosures
The authors declare that they have no conflict of interests.
Acknowledgments
Hereby, we thank the Research Center of Tehran University of Medical Sciences for conducting laboratory tests.
Authors’ Contribution
HA: experimental procedures, study concept,study design, editing and review, BH: study concept,study design, editing and review
Sk: Scientific advisor, editing and review, PA: Statistical analysis, editing and review, FF: Corresponding Author, study concept, manuscript preparation, editing and review
Funding
This paper has been retrieved from thesis No. 957274285 in Hamadan University of Medical Science and the funding was provided by this university.
References
- Kohal RJ, Att W, Bächle M, Butz F. Ceramic abutments and ceramic oral implants An update. Periodontol 2000 2008; 47:224-43. doi: 10.1111/j.1600-0757.2007.00243.x [Crossref] [ Google Scholar]
- Gomes AL, Montero J. Zirconia implant abutments: a review. Med Oral Patol Oral Cir Bucal 2011; 16(1):e50-5. doi: 10.4317/medoral.16.e50 [Crossref] [ Google Scholar]
- Prestipino V, Ingber A. Esthetic high-strength implant abutments Part I. J Esthet Dent 1993; 5(1):29-36. doi: 10.1111/j.1708-8240.1993.tb00741.x [Crossref] [ Google Scholar]
- Monzavi A, Shabanpoor R, Alikhasi M, Omati Shabestari G. Comparison of fracture resistance and failure mode of different zirconia abutments with titanium abutment. J Dent Med 2013; 25(4):232-9. [ Google Scholar]
- Kim S, Kim HI, Brewer JD, Monaco EA Jr. Comparison of fracture resistance of pressable metal ceramic custom implant abutments with CAD/CAM commercially fabricated zirconia implant abutments. J Prosthet Dent 2009; 101(4):226-30. doi: 10.1016/s0022-3913(09)60043-3 [Crossref] [ Google Scholar]
- Jemt T, Lekholm U, Gröndahl K. 3-year followup study of early single implant restorations ad modum Brånemark. Int J Periodontics Restorative Dent 1990; 10(5):340-9. [ Google Scholar]
- Tsuge T, Hagiwara Y. Influence of lateral-oblique cyclic loading on abutment screw loosening of internal and external hexagon implants. Dent Mater J 2009; 28(4):373-81. doi: 10.4012/dmj.28.373 [Crossref] [ Google Scholar]
- Winkler S, Ring K, Ring JD, Boberick KG. Implant screw mechanics and the settling effect: overview. J Oral Implantol 2003; 29(5):242-5. doi: 10.1563/1548-1336(2003)029<0242:ismats>2.3.co;2. [Crossref] [ Google Scholar]
- Lee JH, Frias V, Lee KW, Wright RF. Effect of implant size and shape on implant success rates: a literature review. J Prosthet Dent 2005; 94(4):377-81. doi: 10.1016/j.prosdent.2005.04.018 [Crossref] [ Google Scholar]
- Erneklint C, Odman P, Ortengren U, Karlsson S. An in vitro load evaluation of a conical implant system with 2 abutment designs and 3 different retaining-screw alloys. Int J Oral Maxillofac Implants 2006; 21(5):733-7. [ Google Scholar]
- Nigro F, Sendyk CL, Francischone CE, Jr Jr. , Francischone CE Removal torque of zirconia abutment screws under dry and wet conditions. Braz Dent J 2010; 21(3):225-8. doi: 10.1590/s0103-64402010000300009 [Crossref] [ Google Scholar]
- Gehrke P, Johannson D, Fischer C, Stawarczyk B, Beuer F. In vitro fatigue and fracture resistance of one- and two-piece CAD/CAM zirconia implant abutments. Int J Oral Maxillofac Implants 2015; 30(3):546-54. doi: 10.11607/jomi.3942 [Crossref] [ Google Scholar]
- Gehrke P, Dhom G, Brunner J, Wolf D, Degidi M, Piattelli A. Zirconium implant abutments: fracture strength and influence of cyclic loading on retaining-screw loosening. Quintessence Int 2006; 37(1):19-26. [ Google Scholar]
- Binon PP. Implants and components: entering the new millennium. Int J Oral Maxillofac Implants 2000; 15(1):76-94. [ Google Scholar]
- Byrne D, Houston F, Cleary R, Claffey N. The fit of cast and premachined implant abutments. J Prosthet Dent 1998; 80(2):184-92. doi: 10.1016/s0022-3913(98)70108-8 [Crossref] [ Google Scholar]
- Alikhasi M, Baghaie R, khosronejad N, Aslani P. Evaluation of torque loss value of MAD/MAM zirconia abutments with prefabricated titanium abutments. J Dent Med 2013; 26(1):48-54. [ Google Scholar]
- Tsumita M, Kokubo Y, Kano T, Sasaki K. Effect of fatigue loading on the screw joint stability of zirconium abutment. J Prosthodont Res 2013; 57(3):219-23. doi: 10.1016/j.jpor.2013.02.004 [Crossref] [ Google Scholar]
- Nguyen HQ, Tan KB, Nicholls JI. Load fatigue performance of implant-ceramic abutment combinations. Int J Oral Maxillofac Implants 2009; 24(4):636-46. [ Google Scholar]
- Ghanbarzadeh J, Rajabzadeh M, Nakhaei M, Rajatihaghi H, Tayarani Najjaran N. Torque removal evaluation of screw in one-piece and two-piece abutments tightened with a handheld screwdriver. J Dent Mater Tech 2013; 3(1):11-5. doi: 10.22038/jdmt.2013.2051 [Crossref] [ Google Scholar]
- Cid RN, Lahr GJG, Stanley K, Siqueira AAG, Cardoso AC. Comparative analysis of screw loosening in titanium and zirconia abutments-an in vitro study. EC Dent Sci 2015; 1(2):83-9. [ Google Scholar]
- Almeida PJ, Silva CL, Alves JL, Silva FS, Martins RC, Sampaio Fernandes J. Comparative analysis of the wear of titanium/titanium and titanium/zirconia interfaces in implant/abutment assemblies after thermocycling and mechanical loading. Rev Port Estomatol Cir Maxilofac 2016; 57(4):207-14. doi: 10.1016/j.rpemd.2016.07.002 [Crossref] [ Google Scholar]
- Brodbeck U. The ZiReal Post: a new ceramic implant abutment. J Esthet Restor Dent 2003; 15(1):10-23. doi: 10.1111/j.1708-8240.2003.tb00278.x [Crossref] [ Google Scholar]
- Nakamura K, Kanno T, Milleding P, Ortengren U. Zirconia as a dental implant abutment material: a systematic review. Int J Prosthodont 2010; 23(4):299-309. [ Google Scholar]
- Att W, Kurun S, Gerds T, Strub JR. Fracture resistance of single-tooth implant-supported all-ceramic restorations: an in vitro study. J Prosthet Dent 2006; 95(2):111-6. doi: 10.1016/j.prosdent.2005.12.003 [Crossref] [ Google Scholar]
- Hamilton A, Judge RB, Palamara JE, Evans C. Evaluation of the fit of CAD/CAM abutments. Int J Prosthodont 2013; 26(4):370-80. doi: 10.11607/ijp.3501 [Crossref] [ Google Scholar]