Avicenna J Dent Res. 15(3):122-133.
doi: 10.34172/ajdr.1601
Review Article
Treatment Options for Oral Rehabilitation of the Atrophic Maxilla: A Literature Review
Shaqayeq Ramezanzade 1  , Mahsa Aeinehvand 2
, Mahsa Aeinehvand 2  , Zohaib Khurshid 3, *
, Zohaib Khurshid 3, *  , Seied Omid Keyhan 4, 5, 6
, Seied Omid Keyhan 4, 5, 6  , Hamid Reza Fallahi 7
, Hamid Reza Fallahi 7  , Arash Abbasi 8
, Arash Abbasi 8
Author information:
1PhD Candidate, Department of Cariology and Endodontics, Section for Clinical Oral Microbiology, Faculty of Health and Medical Sciences, Department of Odontology, University of Copenhagen, Copenhagen, Denmark
2MSc, Private Practice, Maxillofacial Surgery & Implantology & Biomaterial Research Foundation, Tehran, Iran
3B.D.S, MRes, FHEA, MDTFEd, MFDS RCPS (Glasgow)/ Department of Prosthodontics and Dental Implantology, King Faisal University, Hofuf, KSA
4DDS, OMFS, Adjunct Honorary Professor, College of Dentistry, Gangneung-Wonju National University, Gangneung, South Korea
5Co-investigator, Department of Oral & Maxillofacial Surgery, University of Florida, College of Medicine, Jaksonville, FL, USA
6Founder & Director of Maxillofacial Surgery & Implantology & Biomaterial Research Foundation, Tehran, Iran
7DDS, OMFS, Private Practice, Founder & Director, Maxillofacial Surgery & Implantology & Biomaterial Research Foundation, Ahvaz, Iran
8DDS, Private Practice, Isfahan University of Medical Sciences, Isfahan, Iran
Abstract
Background: The aim of this narrative literature review was clinical indications as well as common complications of the most common treatment options for oral rehabilitation of the upper jaw. The paper also introduced a novel decision-making tool for guiding the selection of the most appropriate treatment for oral rehabilitation based on patients’ residual bone height, width, and quality.
Methods: This study is a review article based on PubMed and Scopus that was done by reviewing articles from 2000 to 2022. Treatment choices for edentulous maxillae with the insufficient bone for implant placement comprise two broad classifications: bone defect compensation by bone augmentation techniques and modified implant designs for specific situations to utilize the remaining bone. The following factors have to be taken into consideration: the residual bony anatomy, remaining bone volume and quality, skeletal maxillomandibular relationship, scientific evidence, the experience of the clinicians, and, the patients’ increasing demands and expectations.
Results: Grafting techniques are often demanding for both patients and surgeons. Likewise, they are associated with a prolonged treatment time, increased financial cost, and higher complication risks, especially in medically compromised patients. Several non-grafting alternative options have been reported such as zygomatic implants (ZIs), short implants, tilted implants, and the like.
Conclusions: Oral rehabilitation in the upper jaw should follow a comprehensive assessment and examination of the patient’s quality and dimensions of residual bone. The clinical decision between grafting versus non-grafting options is associated with several factors.
Keywords: Maxilla, Mandible, Alveolar bone grafting, Dental implants
Copyright and License Information
© 2023 The Author(s); Published by Hamadan University of Medical Sciences.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.
Please cite this article as follows: Ramezanzade S, Aeinehvand M, Khurshid S, Keyhan SO, Fallahi HR, Abbasi A.Treatmeant options for oral rehabilitation of the atrophic maxilla: A literature review. Avicenna J Dent Res. 2023; 15(3):122-133. doi:10.34172/ajdr.1601
Background
One of the prerequisites for successful implant placement is the presence of sufficient bone in terms of both quantity and quality. Treatment protocols for rehabilitation of the atrophic maxilla have evolved over the last decades, and various treatment options have been developed over time. Previously, in cases where residual bone height/width did not permit placement of conventional dental implants in the maxilla, bone grafting techniques were considered the gold standard (1). Nevertheless, bone grafting techniques are subject to several major shortcomings, including inherent failure rates, inability to simultaneously place and restore implants, donor site, patient morbidity, repeated surgery, and high costs, which often necessitate considering alternative treatments (2). Over time, alternative treatments have been advocated to provide a time and cost-efficient treatment for individuals who are otherwise medically compromised or unwilling to undergo additional surgical procedures. A great deal of confusion and debate exists among clinicians as to what is the best treatment option in cases where maxillary atrophy exists. In order to support the clinician in the decision-making process and to inform the patient more extensively on the available treatment options, we provided a brief narrative review of the literature, clinical indications, as well as common complications of the most common treatment options for oral rehabilitation of the upper jaw. The paper also introduced a novel decision-making tool for guiding the selection of the most appropriate treatment for oral rehabilitation based on patients’ residual bone height, width, and quality.
Materials and Methods
This study is a review article based on PubMed and Scopus that was done by reviewing articles from 2000 to 2022. Keywords used in the search included “Dental Implants” and “Atrophic Maxilla”, “all-on-four”, “Tuberosity Implants”, and “Bone Grafting”.
Results
Bone Atrophy
Since the discovery of the osseointegration phenomenon, endosseous dental implants have been used for oral rehabilitation of total or partial edentulous jaws in cases where sufficient bone volumes are present. However, there are restrictions on placing regular implants where insufficient bone volumes exist. In edentulous jaws, the available bone might become insufficient because of bone atrophy, sinus pneumatization, dental trauma, extractions, periodontal disease, or any combination of these (3,4). In these challenging cases, regular dental treatment may no longer be available or appropriate. Generally, the patterns of bone loss in atrophic jaws are predictable, and bone loss in the anterior as well as the posterior maxilla involves a combination of horizontal and vertical hard tissue loss. Accordingly, a thorough understanding of the anatomical consequences of bone atrophy is essential for clinicians. In 1988, Cawood and Howell investigated the bone resorption patterns in the maxilla and suggested a pathophysiological classification for atrophic ridges (5).
Treatment Selections
In normal circumstances, standard axial implants are used whenever possible. Treatment choices for edentulous maxillae with the insufficient bone for implant placement comprise two broad classifications: bone defect compensation by bone augmentation techniques and modified implant designs for specific situations to utilize the remaining bone, including short implant, all-on-four implant, all-on-six implant, zygomatic implant (ZI), and tilted implant (1). In order to make a clinical decision, decide between these treatment options, and plan the appropriate implant number, position, and prostheses, some factors have to be taken into consideration, including the residual bony anatomy, remaining bone volume and quality, skeletal maxillomandibular relationship, scientific evidence, the experience of the clinicians and, increasingly, and the patient’s demands and expectations. The common treatment options for upper jaw rehabilitation are based on the quantitative and qualitative characteristics of the bone, and different techniques relating to these characteristics are listed below:
1. Standard Dental Implants
Standard-length dental implants are defined as a type of dental implant with an intraosseous length of primarily more than 8 mm. When investigating the differential success rate of the posterior and anterior maxilla, the posterior maxilla is known as the most problematic part of the alveolus for implant placement due to the anatomical features, masticatory dynamics, and functional challenges (6). The two general types are axial and tilted implants. In a systematic review, Del Fabbro et al reported that there is no statistically significant difference between axial and tilted implants regarding failure rate and peri-implant bone loss (7). To ensure acceptable success rates, some investigators reported the minimal bone height for a standard implant in the posterior region to be at least 10 mm in height and 6 mm in width (8).
a. Tuberosity Implants
In this technique, the implant is placed on an incline in the maxillary tuberosity region posterior to the maxillary sinus without sinus invasion.
In a systematic review of tuberosity dental implants, 289 implants with tuberosity implant lengths ranging from 10-14 mm and 10°-35° angulation were placed in a total of 113 patients who were followed for 6–144 months. The overall survival rate of implants placed in the tuberosity region was 94.63% with seven reports of failures (i.e., complete implant removal) in maxillary tuberosity (9). Since the bone in this area is cancellous and primarily type III and IV, immediate loading is not recommended (10). Although modern surface treatments reduce the need for bicortical anchorage and the risk of tuberosity fracture, some studies reported the achievement of bicortical fixation for bone of low density (11,12). Special care must be given to the region posterior and medial to the tuberosity considering the maxillary artery and its branches, specifically the greater palatine artery (10).
b. Pterygoid Implants
A pterygoid implant is a 10–20 mm implant (implants as long as 7 or 8.5 mm were also placed in this region) anchored in the pyramidal process of the palatine bone and the pterygoid process of the sphenoid bone with an angulation between 35°and 55° (9). Placed in dense cortical bone with a reported success rate of 90.7% and similar marginal bone loss levels to those of conventional implants, pterygoid implant appear to be a more predictable alternative for the treatment of patients with insufficient bone volume in the maxillary region than tuberosity implants (13).
With regards to complications, peri-surgical bleedings were relatively easy to manage with local hemostatic methods, although a rare but possible complication with pterygoid implants is severe bleeding due to the proximity of the internal maxillary artery, which runs 1 cm above the pterygomaxillary suture (14). Additionally, a minimum mouth opening of 35 mm seemed necessary for the correct angulation in the posterior region (13).
c. The All-on-4® Treatment Concept
This treatment concept was first introduced in the 1990s with the aim of immediate function and negating the need for any grafting techniques or additional surgery. A total of four implants with two axial implants placed anteriorly and two posterior implants distally tilted between 30° and 45° have proven to be reliable for even distribution of occlusal forces and reduction of cantilever extensions even in cases of bone atrophy (15,16). The use of tilted implants is a non-grafting way to manage limited bone height by allowing for increased length using tilted implants. To ensure optimal three-dimensional (3D) implant positioning for anatomical structures and prosthetic parameters, computer-assisted implant placement for tilted implants is highly recommended (17).
First, the all-on-four treatment was developed for the mandible, and this technique was also advocated for the atrophic edentulous maxilla. The all-on-four treatment concept appeared to be a safe and predictable treatment option in patients exhibiting ridges classified as IV, V, and VI according to Cawood and Howell classification (18). The mandatory bone volume for this treatment is 5 mm in width and 10 mm in height from canine to canine. In most difficult cases, rehabilitation is possible with standard all-on-four (e.g., the insertion of implants with dehiscences, fenestrations, trans-sinus, or pterygoid), and hybrid all-on-four and extra-maxillary ZIs are only indicated for extreme bone atrophies (19) Depending on the anatomical structure, implant inclination can vary from 30 to 45 degrees (20). An excellent cumulative survival rate of up to 99% for implants (21) and a prosthetic survival of 95% after 10 years of follow-up have been reported (22). Moreover, detachment of an element of the definitive prosthesis (most common), surgical guide fractures, and low primary stability were frequently reported concerning technical and prosthetic complications (23). Only a small number of biological complications (e.g., peri-implantitis) were reported after a mean follow-up of two years (20). However, this technique is highly dependent on a period of training and acquisition of both surgical and restorative skills (19).
Recently, in a comparative study, the all-on-four model has been simulated, and von Mises stresses have been studied in five different loading modes (24). When simulated under different loads, both models exhibited the distribution of similar stress patterns, indicating that the all-on-four method was the therapeutic choice for the atrophic edentulous ridges that increased the overall longevity of the prosthesis and greatly minimized the stress distribution.
d. The All-on-6 Treatment Concept
In 2014, Agliardi et al (25) stated that six implants in the edentulous maxilla could provide a profoundly cost- and time-effective alternative to bone grafts for the immediate restoration of the atrophic edentulous maxilla with reduced patient morbidity. This treatment concept benefits from two axial and four tilted implants. When the 5-year clinical and radiological outcomes of the two techniques (All-on-4® and All-on-6) were compared, no statistically significant difference was observed regarding technical and biological complications and marginal bone loss between the two groups. However, a slightly higher complication rate and a higher implant failure rate were reported for the first group and the latter group, respectively (18). Bhering et al stated that the six-implant design has more favorable biomechanical aspects such as lower stress on the implants, abutments, and bone supports compared to the all-on-four concept which results in better clinical outcomes (26).
2. Bone Grafting Techniques in Conjunction With Endo-osseous Implants
Over the decades, in cases where standard implant placement was contraindicated, one approach was to utilize different types of alveolar ridge augmentation which was considered the gold standard treatment option (1). Figure 1 shows a severely atrophic maxilla treated with a combination of grafting techniques. The standard implants were inserted with a several-month delay (Figure 2). Bone augmentation can also be advocated as a facultative indication in less atrophic ridges (Cawood and Howell class IV) with simultaneous dental implant placement (where short and/or narrow and/or tilted implants are alternatives). This was based on the fact that sufficient bone volume at edentulous sites ensures the long-term success rate of dental implants (27). Various grafting techniques have been proposed and advocated prior to (staged approach) or simultaneously with endo-osseous implants, thus aiming to increase bone volume. The goal is to provide a suitable foundation for dental implant placement as well as provide soft tissue support for optimal esthetic results (28). The overall survival rates of dental implants placed in the reconstructed maxilla are significantly lower than those placed in native bone (29); however, some reported no significant difference when comparing the two (30).
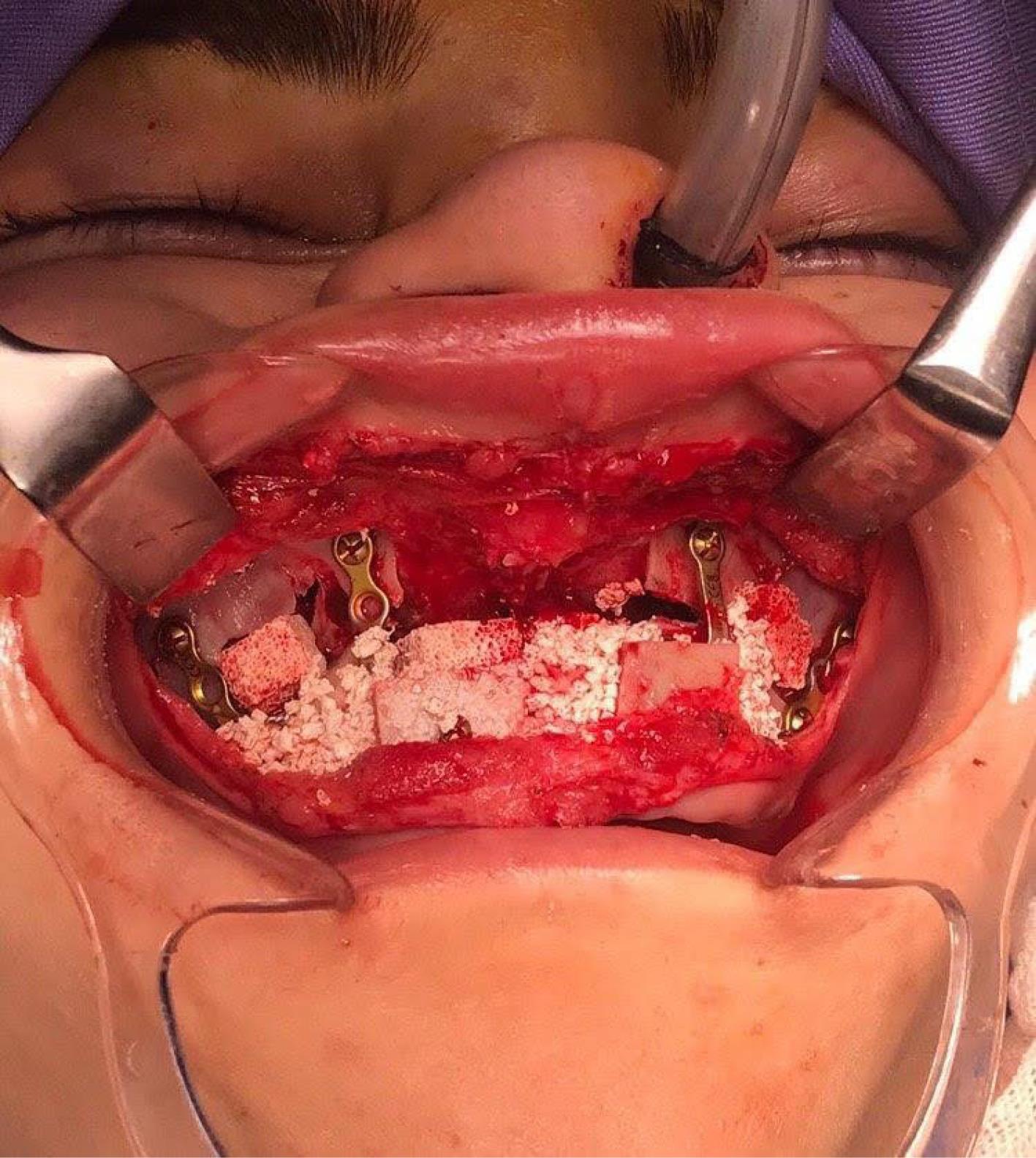
Figure 1.
A Severely Atrophic Maxilla Was Treated with a Combination of Grafting Techniques
.
A Severely Atrophic Maxilla Was Treated with a Combination of Grafting Techniques
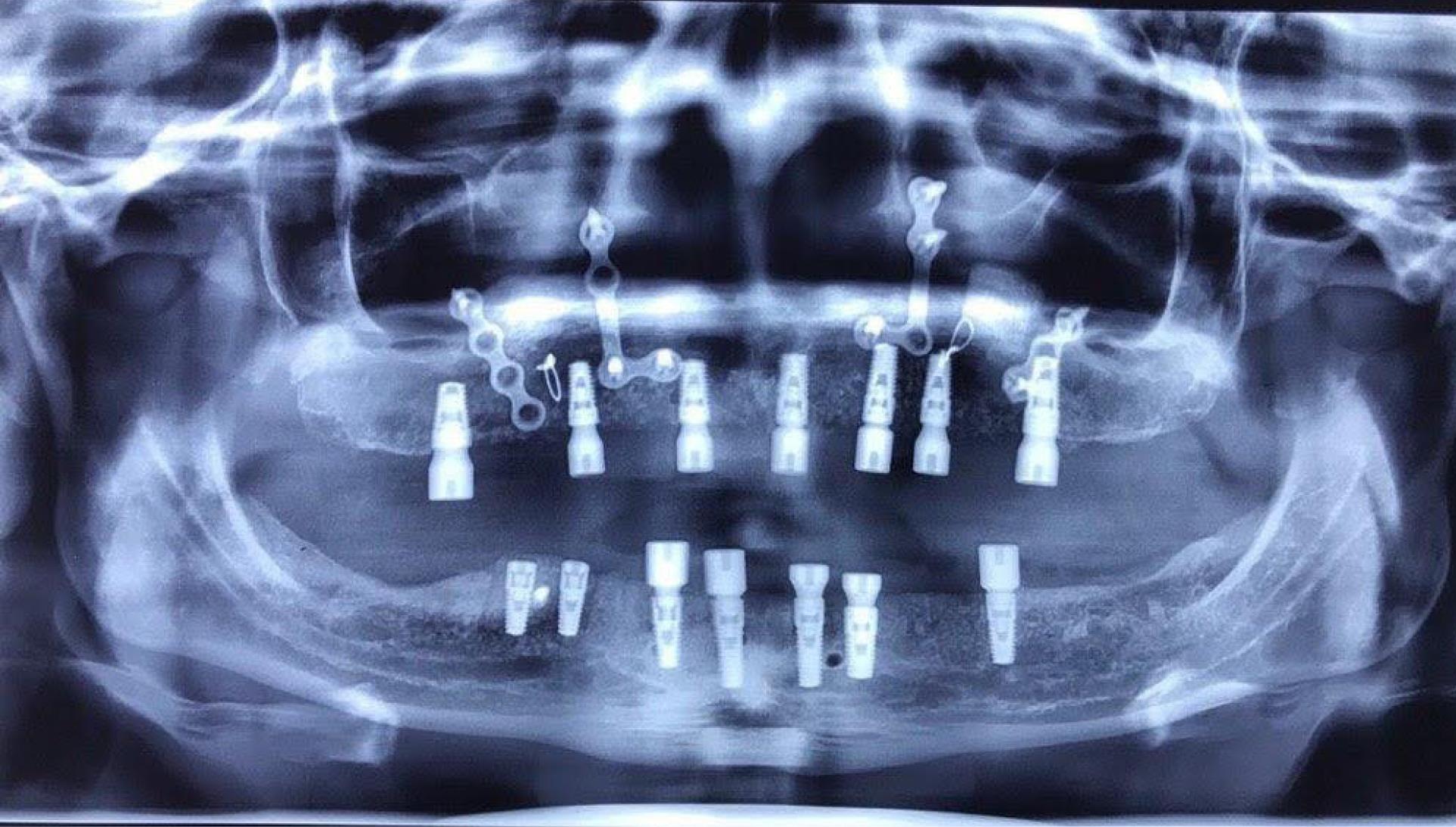
Figure 2.
The Standard Implants Were Inserted With a Several-Month Delay
.
The Standard Implants Were Inserted With a Several-Month Delay
An updated review illustrated that a narrow implant is a reliable treatment option with a good survival rate, an acceptable success rate, and a minimum bone loss (31). This study investigated 1245 implants in seven clinical trials, three randomized clinical trials, three cohort studies, and two case series, and the survival rate of narrow implants was 97%.
Two general methods have been advocated. First, dental implant placement simultaneous with bone grafting can be a safe and predictable surgical technique where adequate primary stability is achieved (32). Second, residual bone is very atrophic and does not provide sufficient primary stability, therefore implants are inserted with a 4-12 month delay based on the graft material used (33). In such severely atrophic cases, vast quantities of bone are often needed to place conventional dental implants, and onlay grafts are mostly used for such big regenerations (34).
The most popular surgical procedures to obtain bone augmentation for the atrophic maxilla include onlay block grafts, sinus floor elevation, guided bone regeneration (GBR), distraction osteogenesis (DO), and interposition grafts. In severe atrophic cases, a combination of techniques might be advocated.
a. Onlay Block Grafts
Historically, this bone augmentation technique has been chosen for vertical and horizontal bone defects with heights less than 5 mm (Cawood and Howell class IV-VI) (35) and/or widths less than 4 mm or less than 5 mm in the aesthetic areas with a high labial line (36). Among grafting materials, onlay grafts provide a more favorable environment for implantation, especially in horizontal deficiencies. High success rates and evidence of bone gain were found with this technique in several systematic reviews (4,30,37). A systematic review reported a survival rate ranging from 96.9% to 100% for lateral augmentation procedures and 89.5% to 100% for vertical augmentation. This technique is associated with relevant morbidity and several complications, including mucosal dehiscence, bone graft, membrane exposures, graft failures, and neurosensory alterations (30). Long-term bone resorption with this technique has been acknowledged, especially in cases of autologous iliac blocks. A biological limitation with onlay graft materials is the low increase in height. Troeltzsch et al (38) in their systematic review reported that the mean vertical augmentation gain was 3.7 mm and 5 mm for particulate onlay grafts and block onlay grafts, respectively, which is probably due to the limitations of angiogenesis. Nonetheless, this technique necessitates extensive soft tissue manipulations to keep the grafts covered and prevent dehiscence. In cases of autologous bone blocks, additional considerations include donor site morbidity, and complications (39). Figures 3 and 4 show the bone harvesting from the iliac crest. Increased morbidity, resorption of a significant part of the graft, or its exposure from the vertical gain are higher compared to the treatment of horizontal deficiencies (40).

Figure 3.
Bone Harvesting from the Iliac Crest
.
Bone Harvesting from the Iliac Crest

Figure 4.
Bone Harvesting From the Iliac Crest
.
Bone Harvesting From the Iliac Crest
b. Sinus Floor Elevation
This procedure is advocated to compensate for sinus pneumatization. It is based on GBR principles and considers the Schneiderian membrane as a natural inborn barrier. Apical elevation of this membrane, mostly in conjunction with bone materials, stimulates bone formation (13). The aim is a vertical augmentation in free-end maxillae with 5-9 mm gained height, and the two widely used techniques include direct and indirect methods. Sinus augmentation and elevation may be performed with or without grafting biomaterials. Ortega-Mejia et al (41) reported better clinical outcomes regarding implant survival, bone gain, and bone height when using platelet-rich plasma in maxillary sinus augmentation. As reported by a systematic review, the survival rates of implants after a minimum of three years of loading were 97.2% and 93.7% for the transrectal approach and lateral window, respectively (42). Complications associated with sinus lift procedures include membrane perforation and hemorrhage, and infection with iatrogenic perforation was the most frequent complication. This occurs in 10%-20% of cases using a lateral approach. Postsurgical sinusitis is rare and may occur in only 3% and 1% of cases following lateral and transrectal augmentation, respectively. There were also rare but catastrophic incidences of the spread of infection to intracranial structures via the cavernous sinus. Furthermore, long healing periods of bone formation are another major shortcoming of this technique (13).
Concerning the two used approaches, a remarkable survival rate of 95.5% with a low complication rate of 4.7% has been reported for the lateral window approach. Likewise, based on remaining bone and bone quality, an initial ridge with 5 mm in height was mostly considered the threshold for the possibility of simultaneous implant placement (43); nevertheless, several favorable outcomes were reported for a 2-4 mm ridge and simultaneous implant placement (44,45). Therefore, the conclusion relies on the possibility of achieving primary stability. In case the clinician preferred a two-stage procedure, the average time between the lifting procedure and implantation was 5.6 to 6.6 months for autografts and bone substitutes, respectively (43).
When a minimal bone height and satisfactory primary stability exist, utilizing the indirect technique (i.e., transcrestal approach) can be a reliable and less invasive approach compared to the lateral window technique (1). According to the treatment concept by Thoma et al (46), the transrectal sinus elevation approach can be the selected treatment when vertical ridge dimensions exceed 8 mm, and when standard implants are the preferred option. In case of peri-implantation complications such as Schneiderian membrane perforation and insufficient primary stability, the indirect technique might be switched to direct to avoid aborting surgery (32).
c. Guided Bone Regeneration
This approach relies on using barrier membranes for space preservation over horizontal or vertical bony defects to keep specific cell types, including rapidly proliferating epithelium and connective tissue cells away and differentially promoting the ingrowth of osteogenic cells from the host site. The most frequent complication of this technique is premature membrane exposure (up to 38%) and the possibility of subsequent infection, which results in regenerated bone loss (13-47). GBR through non-resorbable membranes appeared to be a robust and predictable procedure for bone augmentation; however, it is highly technique-sensitive and strictly dependent on the expertise of the surgeon. Two different approaches have been advocated in this regard: utilization of either a resorbable member such as collagen membrane or a non-resorbable membrane such as polytetrafluoroethylene titanium-reinforced membrane. For vertical ridge augmentation in both approaches, the membrane is supported by a titanium mesh or a titanium osteosynthesis plate as a space maintainer and allows for undisturbed consolidation of the underlying bone (48). Early or late membrane exposure after GBR procedures leads to contamination and infection of the biomaterial, exerting a detrimental impact on the success of bone augmentation.
d. Distraction Osteogenesis
First introduced in 1996 by Chin and Toth (49), DO was used to reconstruct vertical or horizontal bony defects. Although this technique allows the alveolar ridge to be augmented through new bone formation (osteogenesis) and a significant increase in the surrounding soft tissue (histogenesis), it does not require the interposition of a bone graft by the formal addition of GBR (50). The primary indication of this technique is in the edentulous zone including three or more missing teeth with a minimum of 6–7 mm residual bone height and at least a 4 mm vertical defect when measured from the adjacent bony walls. In moderate atrophies, DO is first performed and then followed by an onlay bone graft, whereas in severe atrophies, a primary onlay bone graft might be followed by DO after a four-month healing period (1). The suggested survival rates for DO are similar to those reported for other augmentation techniques, but unacceptably high complication rates have been also reported (50). Another review reported that 8% of cases underwent partial relapse of the initial bone height, 8% reported a change of the distraction vector, 3% of cases indicated basal bone or segment fracture, and 2% exhibited fracture of the distraction device. Additionally, several incomplete distraction outcomes, transient paresthesia, and total failure were also reported (29). Breakage of internal maxillary distractors was a noticeable and frequent complication, and to prevent this phenomenon, any unnecessary and frequent bending for adaptation to the bone surface should be avoided during the advancement and retention periods (51). Generally, DO is not the treatment of choice for the correction of narrow ridges (13).
e. Interpositional Grafts (Le Fort I Interposition in the Maxilla)
Introduced in 1987 by Keller et al (39), this technique can provide large quantities of bone required for implantation in the severely atrophic maxilla, along with re-establishing a favorable intermaxillary relationship by repositioning the maxilla both forwards and downwards with the graft secured between both the nasal and sinus floors and maxilla (39). A two-staged implant placement protocol is preferred with this technique. In the original technique, the osteotomy lines went through the sinus and were cut through the sinus membrane due to a large amount of needed bone, and the iliac crest bone was mainly used as the donor site (52). However, in a recent modification suggested by Terheyden (53), nasal and sinus floor membrane elevation precedes the down fracture, leaving the sinus floor implant in a more favorable position for healing. This creates a recipient site closed from all sides that can be filled with particulate grafts and/or bone substitutes instead of iliac grafts. In 2016, a meta-analysis reported a survival rate of 89.6% for implantation after Le Fort I interpositional grafting in edentulous upper jaws (54). However higher survival rates (a 10-year survival of 95.1%) were further reported following the new modifications. Furthermore, vertical bone augmentation in the anterior maxilla through this technique is limited to a 2-4 mm gain of height due to the rigidity of the palatal soft tissue (39).
The review by Roccuzzo et al (55) reported the use of the sandwich technique for increasing the mandibular vertical ridge augmentation and indicated that the survival rate after a mean follow-up of 3.7 years is 94%, which is acceptable. The available clinical data showed that the present technique is a reliable option for the treatment, and the reported complications are mostly transient and provide favorable conditions for subsequent implant placement.
f. Subperiosteal Implants
First introduced by Dahl et al (56), subperiosteal implants were designated for oral rehabilitation in both jaws although the most successful results are obtained in the lower jaw. Known complications with the sub-periosteal device in the upper jaw are bone resorption and fibrous encapsulation of the implant (57). Furthermore, sinus perforation and sinusitis are other possible complications with this treatment option (58). Figures 5, 6, and 7 present the subperiosteal implants placed in an atrophic edentulous maxilla.
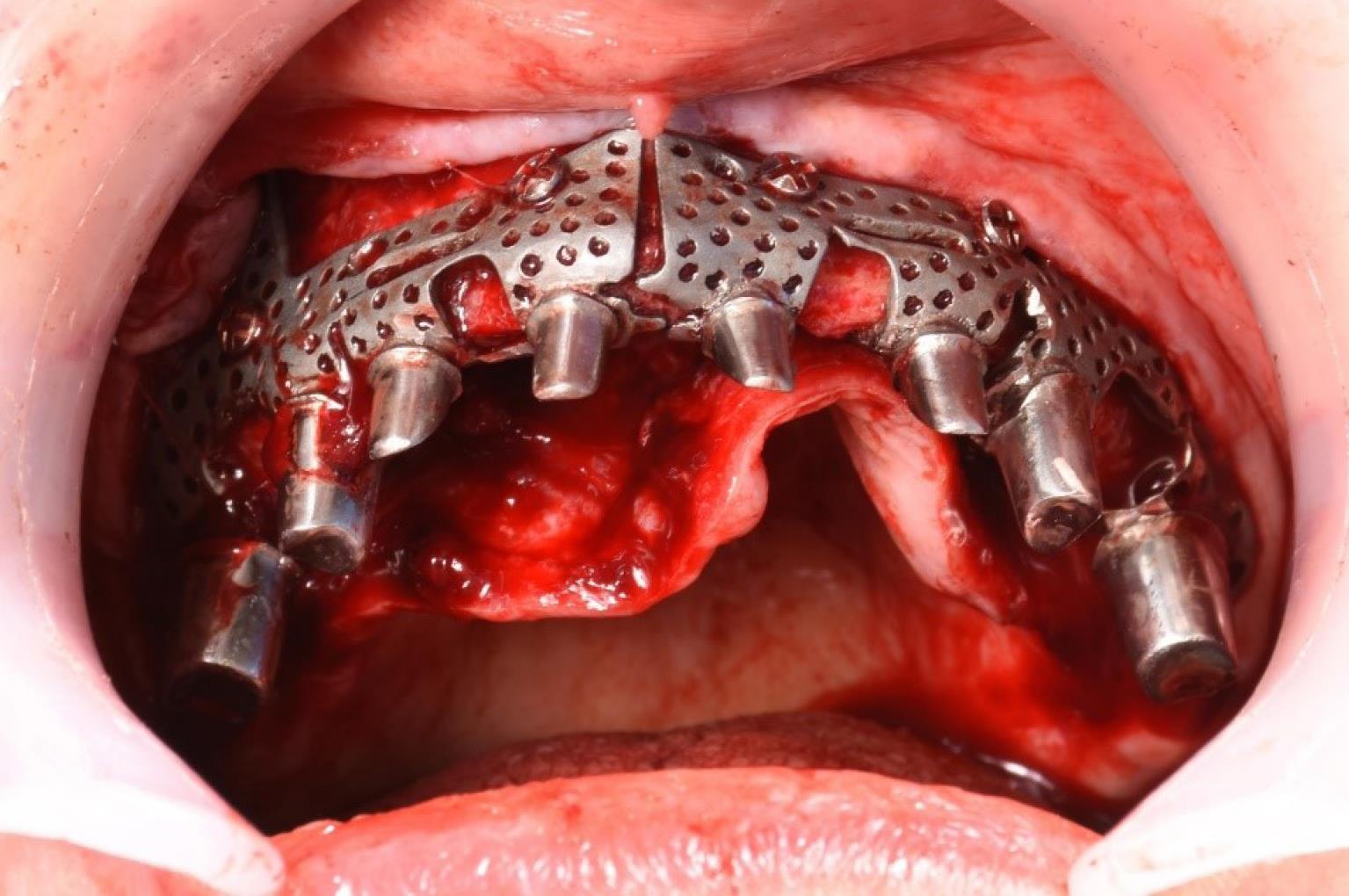
Figure 5.
The subperiosteal implants were placed in an atrophic edentulous maxilla
.
The subperiosteal implants were placed in an atrophic edentulous maxilla

Figure 6.
The subperiosteal implants were placed in an atrophic edentulous maxilla
.
The subperiosteal implants were placed in an atrophic edentulous maxilla
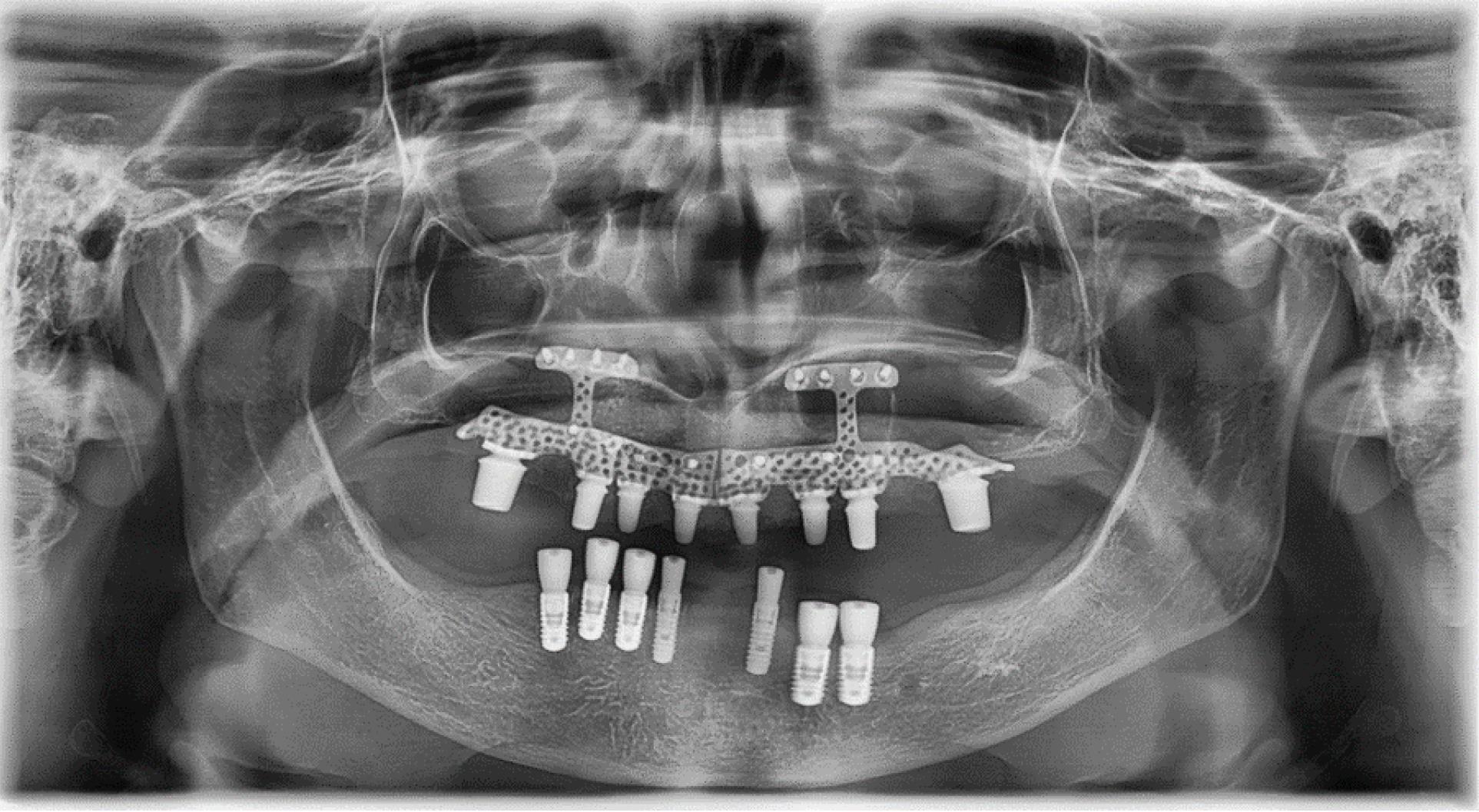
Figure 7.
The radiography of the subperiosteal implants placed in an atrophic edentulous maxilla
.
The radiography of the subperiosteal implants placed in an atrophic edentulous maxilla
g. Short Implants (in Combination With Other Implant Options)
Short implants (5 mm to 10 mm in length) are used in the atrophic maxilla because they do not need complicated bone grafting procedures while presenting survival rates similar to that of grafting techniques with regular implants. This treatment is recommended when the height of residual bone is higher than 6 mm, and there is enough width to place at least an implant with 5 mm in diameter (59). Likewise, short implants can be utilized with a more favorable prosthetic design and lower complication rate when compared with sinus lift/bone augmentation procedures with regular implants (60). Short implants with lengths less than 5-6 mm in conjunction with sinus floor elevation techniques significantly diminished survival rates; hence, using short implants was usually reported when a residual alveolar height is more than 6 mm with sufficient width (61). It should be noted that the failure rate of short implants in the posterior region of the maxilla, which has poor bone quality and may fail to achieve cortical bone engagement, is apparently higher than in the anterior area. Therefore, surface-treated short implants have been introduced to overcome this challenge (62).
h. Zygomatic Implants
The treatment outcomes, survival rates, and complications following oral rehabilitation with ZIs have been reported in several systematic reviews. Moreover, meta-analyses involving short-term and long-term non-comparative articles have demonstrated that using zygoma bone as an anchorage appears to be a promising alternative to significant bone augmentation procedures in the severely atrophic maxilla, even with low bone quality, especially in patients whose bone grafts cannot be harvested and in situations where there is insufficient primary stability and/or implant placement, or utilization can only be undertaken after several months delay. A survival rate ranging from 95.2% to 100% has been reported for ZIs in atrophic maxillas (63-66) although this number was lower for patients with resected maxillas (78.57%). They were indicated in cases with residual bone height coronal to the maxillary sinus less than 2–4 mm (67,68). ZIs must have a minimum of 8-10 mm bone-implant contact within zygoma bone even in atrophic jaws with insufficient crestal bone which provides adequate primary stability (69). This treatment option does not lack complications, but the majority of ZIs are mild and facile to manage and rarely catastrophic (65). A relatively uncommon (15%) but significant problem associated with ZI placement is sinusitis; however, the initial modifications such as avoiding sinus entry or membrane perforation have dramatically reduced the rate of sinusitis and further oroantral fistula formation which possibly necessitate ZI removal. Furthermore, any sinus symptoms must be treated before ZI placement. Over time, the modifications of ZIs emerged more on locating an exteriorized position by avoiding sinus invasion, and latterly an extra maxillary protocol was advocated which provided more convenient prosthetic rehabilitations while avoiding sinus encroachment (70,71). Regarding ZI placement, the clinical expertise of the surgeon is critical for success and minimizing complications.
Generally, the combined option (two ZIs with standard implants) was preferred due to lower costs and lower risk of serious complications such as orbital penetration during surgical placement (72). The preferred anterior implants in conjunction with a posterior zygoma implant are standard-length implants with a minimum length of 10 mm. If the remained anterior bone precludes placement of standard-length implants, the zygoma quad will be preferred (73).
There is a controversy over the use of two short implants ( < 10 mm) in the anterior maxilla in conjunction with two posterior ZIs or using the zygoma quad. Some state that the zygoma quad was the choice in patients with severe anterior maxilla bone deficiencies in which there is not enough bone in the anterior maxillary region to allow the placement of at least two short implants and in patients requiring additional advanced bone-grafting procedures in the anterior region to place standard length implants (3). On the other hand, some advocate that it is prudent to perform a zygoma quad when placing conventional implants of at least 10 mm in the anterior maxilla is not possible (74).
h1. Extramaxillary ZIs
In cases where the residual ridge does not meet the previously mentioned protocol for the standard All-on-4, the ZI placement is needed that consists of two types:the hybrid designated All-on-4 and All-on-4 extramaxilla.
h1.1. The Hybrid Designated All-on-4
This is a combination of the conventional All-on-4® technique with extra maxillary ZIs indicated for cases with C-VI classes according to Cawood and Howell classification which have maintained the bone proximal to the midline (75). In cases when extensive prosthetic flanges are required, the hygienic maintenance of the prosthesis might be challenging (18).
h.1.2. All-on-4 Extramaxilla
Endline cases with more than C-VI class of Cawood, and Howel classification are those who were indicated to use this protocol. Special care should be given to the infraorbital foramen and the base of the orbit when placing extra-maxillary ZIs (75,76).
Discussion
Bone deficiency for implant placement is a significant challenge among clinicians. Due to the advancement of implant placement techniques in the atrophic edentulous maxilla, areas that previously could only be managed with removable dentures can now be rehabilitated with an implant-supported prosthesis with or without grafting with high success rates (77). Over the decades, in cases where standard implant placement was contraindicated, one approach was to utilize different types of alveolar ridge augmentation, and autogenous bone was considered the gold standard treatment option in areas such as the sinus and nasal lifting procedures, inter-positional bone grafting in conjunction with a Le Fort I procedure, and onlay grafts (1-29). Grafting techniques are often demanding for both patients and surgeons. Likewise, they are associated with a prolonged treatment time, increased financial cost, and higher complication risks, especially in medically compromised patients. In the last decades, several non-grafting alternative options have been reported such as ZIs, short implants, tilted implants, and the like. Oral rehabilitation in the upper jaw should follow a comprehensive assessment and examination of the patient’s quality and dimensions of residual bone (78). Figure 8 displays the classification of treatment options for edentulous maxilla rehabilitation. The clinical decision between grafting versus non-grafting options is associated with several factors, including surgeon expertise, scientific evidence, and the patient’s increasing preferences.
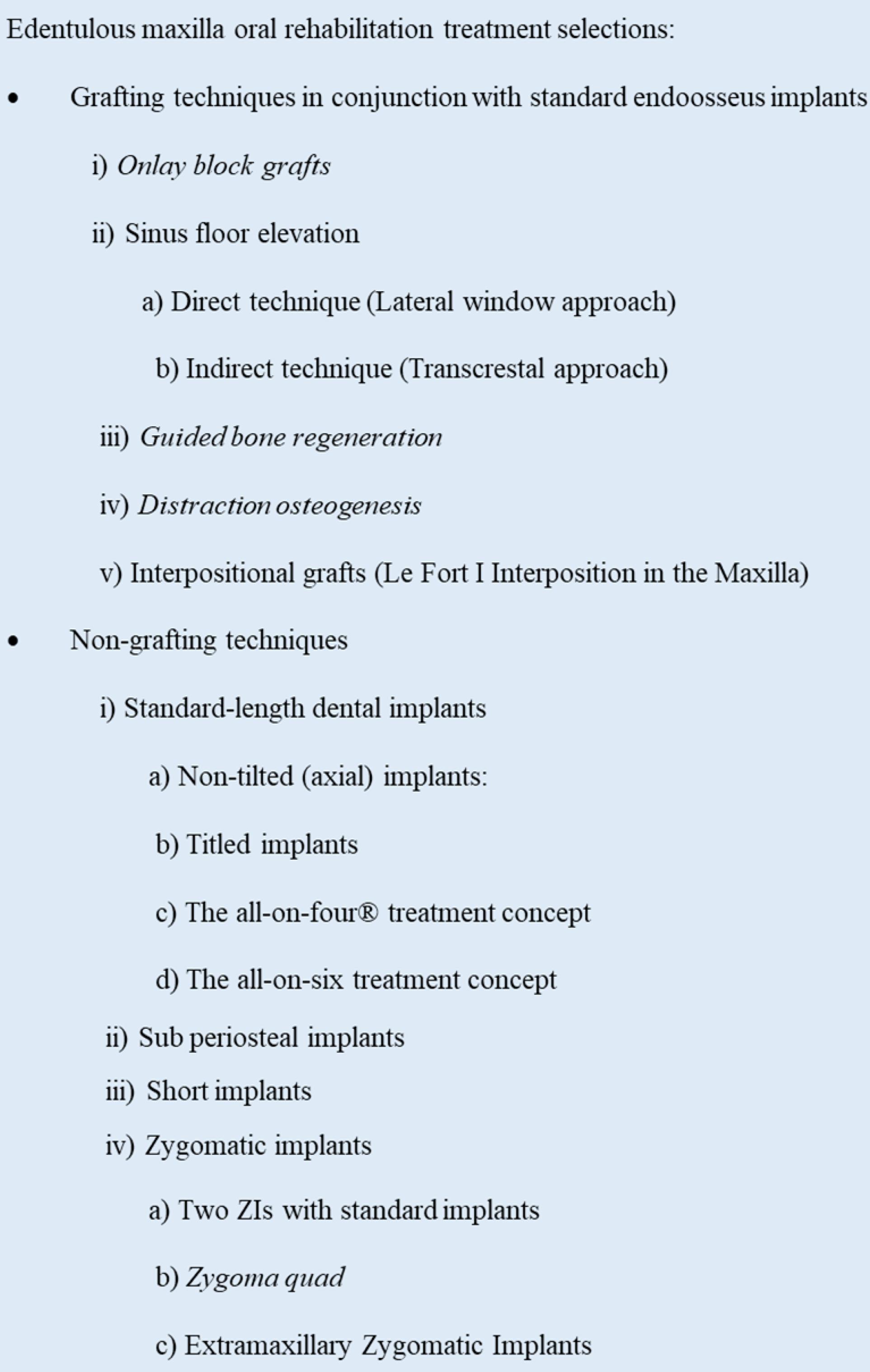
Figure 8.
The Classification of Treatment Options for Edentulous Maxilla Rehabilitation
.
The Classification of Treatment Options for Edentulous Maxilla Rehabilitation
Tilted Standard Length Dental Implants vs Standard Implants with Grafting Techniques in Atrophic Maxilla
As a result of tooth loss combined with sinus pneumatization, there is usually sufficient cortical bone in the anterior regions of the maxilla but the insufficient bone in the premolar and molar regions (79). The adoption of tilted implants as an alternative to bone grafting procedures has been proposed in recent years. Tilted implants allow for conventional-length implants with the engagement of as much cortical bone as possible in the atrophic alveolar bone. They also reduce the posterior cantilever length and enhance load distribution by increasing the inter-implant space. Tilted implants have several biomechanical advantages and make immediate implant placement possible in edentulous cases with atrophic ridges. It should be noted that there was no statistically significant difference between straight/axial and tilted implants in terms of implant success, as observed in a systematic review with meta-analysis (42). A minimum height of 6 mm and width of 5 mm in the anterior maxillary seem to be necessary for successful results. Furthermore, a promising short-term survival rate was reported for different systems using tilted implants such as all-on-four, all-on-six, and the like; however, further studies are required for long-term assessments (21).
Subperiosteal Implants vs Standard Implants with Grafting Techniques in Atrophic Maxilla
Nowadays, sub-periosteal implants are rarely used for the rehabilitation of a severely atrophied maxilla. This treatment has now been widely replaced by ZIs that yield more reliable and tangible results (80). The relatively high failure rate of this treatment in the atrophic edentulous maxilla is attributed to the negative impact of gravity on the bone-implant contact zone and difficulties in placing subperiosteal implant devices on a cortical bone basis (81). Owing to 3D surgical planning and 3D printing of appropriate materials, there is a possibility of new interest in these devices, but currently, there are not much data in this regard to reach a conclusion.
Short Implants vs Standard Implants with Grafting Techniques in Atrophic Maxilla
Several systematic reviews and meta-analyses have compared the survival/implant failure of short implants (5-8.5 mm) in the pristine bone to longer implants with sinus lifting procedures, finding no statistically significant difference between the two groups but suggesting similar survival rates. Short implants were associated with less post-surgical complication and lower marginal bone loss around the implant site (60,78,82,83). When considering peri-surgical complications, conventional implants with augmentation expose patients to a three times higher risk of complications compared to short implants. Moreover, despite yielding tangible outcomes, nasal and sinus lifting procedures are associated with sinusitis, fistulae, implant/graft loss, osteomyelitis, and other issues that are detrimental to patient well-being. Whenever applicable, short implants are a more beneficial option, especially in patients who are medically or financially compromised or unwilling to undergo additional surgical procedures (46).
A recent systematic review has indicated that studies using sandwich techniques demonstrated significant survival in most short-length implants compared with regular-sized implants and augmented bone over 5 years (84). Short implants consistently showed minor changes in marginal bone level than regular implants did. Additionally, a systematic review examining the survival and success rates of implants placed with autogenous intraoral onlay bone grafts demonstrated that the survival and success rates of dental implants placed in onlay bone grafts are similar to those of short implants placed in the native bone while introducing more challenges and morbidity. Therefore, inadequate bone and short implants are more feasible treatment options than those implants placed in conjunction with onlay grafts (30).
ZIs Versus Grafting Techniques
In cases where limited amounts of bone regeneration are needed, grafting materials with simultaneous standard implant placement for single implants can be a reliable and predictable choice (33). Considering all potential complications and low patient satisfaction, formal bone grafting techniques lack simultaneous placement, and their primary stability or immediate reconstruction should be replaced with an alternative treatment with lower costs, fewer complications, shortened time for rehabilitation, and higher survival rates. Therefore, ZIs have been introduced as alternatives to formal grafting techniques due to their advantages. Different ZI placement techniques are present which provide a predictable and efficient way to rehabilitate the severely atrophic maxilla with reduced levels of complications. Quad zygomas are the first treatment choice in severe maxillary atrophy with inadequate bone volume for the placement of conventional implants anteriorly and posteriorly (68) and are a rescue option in grafting failures (73). Nonetheless, complications can be present, and the provision of ZI is highly user and technique sensitive (85).
Shortcomings and Strengths of Non-grafting Techniques
The main shortcoming of this study was the lack of longer-term clinical and laboratory studies covering 10 years and above to determine long-term outcomes of the non-grafting technique. It should be noted that non-grafting techniques, especially ZIs, require special precautions while performing surgery, which might be time-consuming. They also require a defined period of training and understanding and have a formidable learning curve (85).
Following non-grafting solutions for maxillary rehabilitation, temporary prosthetic restorations are mostly made and immediately start functioning, releasing patients from remaining edentulous and enabling them phonetically, aesthetically, and functionally (73-86).
Authors’ Contribution
Conceptualization: Shaqayeq Ramezanzade, Seied Omid Keyhan, Hamid Reza Fallahi.
Data curation: Seied Omid Keyhan, Hamid Reza Fallahi.
Investigation: Shaqayeq Ramezanzade.
Methodology: Shaqayeq Ramezanzade, Mahsa Aeinehvand, Arash Abbasi.
Project administration: Seied Omid Keyhan.
Supervision: Zohaib Khurshid, Seied Omid Keyhan, Hamid Reza Fallahi.
Writing–original draft: Shaqayeq Ramezanzade, Mahsa Aeinehvand, Arash Abbasi.
Writing–review & editing: Zohaib Khurshid, Seied Omid Keyhan, Hamid Reza Fallahi.
Competing Interests
None.
Ethical Approval
Not applicable.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Ali SA, Karthigeyan S, Deivanai M, Kumar A. Implant rehabilitation for atrophic maxilla: a review. J Indian Prosthodont Soc 2014; 14(3):196-207. doi: 10.1007/s13191-014-0360-4 [Crossref] [ Google Scholar]
- Aparicio C, Manresa C, Francisco K, Claros P, Alández J, González-Martín O. Zygomatic implants: indications, techniques and outcomes, and the zygomatic success code. Periodontol 2000 2014; 66(1):41-58. doi: 10.1111/prd.12038 [Crossref] [ Google Scholar]
- Aeran A, Srivastava R, Palekar U, Choukse V, Jain R. Zygomatic implants–a review. NJDSR 2016; 1(4):19-23. [ Google Scholar]
- Esposito M, Grusovin MG, Coulthard P, Worthington HV. The efficacy of various bone augmentation procedures for dental implants: a Cochrane systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants 2006; 21(5):696-710. [ Google Scholar]
- Cawood JI, Howell RA. A classification of the edentulous jaws. Int J Oral Maxillofac Surg 1988; 17(4):232-6. doi: 10.1016/s0901-5027(88)80047-x [Crossref] [ Google Scholar]
- Nevins M, Fiorellini JP. Placement of maxillary posterior implants. In: Nevins M, Mellonig JT, eds. Implant Therapy, Clinical Approaches and Evidence of Success, Vol 2. Chicago:.
- Quintessence, 1998:153-169.
- Del Fabbro M, Bellini CM, Romeo D, Francetti L. Tilted implants for the rehabilitation of edentulous jaws: a systematic review. Clin Implant Dent Relat Res 2012; 14(4):612-21. doi: 10.1111/j.1708-8208.2010.00288.x [Crossref] [ Google Scholar]
- ten Bruggenkate CM, van den Bergh JP. Maxillary sinus floor elevation: a valuable pre-prosthetic procedure. Periodontol 2000 1998; 17:176-82. doi: 10.1111/j.1600-0757.1998.tb00133.x [Crossref] [ Google Scholar]
- Lopes LF, da Silva VF, Santiago JF Jr, Panzarini SR, Pellizzer EP. Placement of dental implants in the maxillary tuberosity: a systematic review. Int J Oral Maxillofac Surg 2015; 44(2):229-38. doi: 10.1016/j.ijom.2014.08.005 [Crossref] [ Google Scholar]
- Ridell A, Gröndahl K, Sennerby L. Placement of Brånemark implants in the maxillary tuber region: anatomical considerations, surgical technique and long-term results. Clin Oral Implants Res 2009; 20(1):94-8. doi: 10.1111/j.1600-0501.2007.01491.x [Crossref] [ Google Scholar]
- Goiato MC, dos Santos DM, Santiago JF Jr, Moreno A, Pellizzer EP. Longevity of dental implants in type IV bone: a systematic review. Int J Oral Maxillofac Surg 2014; 43(9):1108-16. doi: 10.1016/j.ijom.2014.02.016 [Crossref] [ Google Scholar]
- Nocini PF, Albanese M, Fior A, De Santis D. Implant placement in the maxillary tuberosity: the Summers’ technique performed with modified osteotomes. Clin Oral Implants Res 2000; 11(3):273-8. doi: 10.1034/j.1600-0501.2000.011003273.x [Crossref] [ Google Scholar]
- Pommer B, Zechner W, Watzek G, Palmer R. To graft or not to graft? Evidence-based guide to decision making in oral bone graft surgery. In: Zorzi A, and Joao Batista de Miranda JB, eds. Bone Grafting. IntechOpen; 2012. p. 1-25. 10.5772/30989.
- Candel E, Peñarrocha D, Peñarrocha M. Rehabilitation of the atrophic posterior maxilla with pterygoid implants: a review. J Oral Implantol 2012; 38 Spec No:461-6. doi: 10.1563/aaid-joi-d-10-00200 [Crossref] [ Google Scholar]
- Maló P, Rangert B, Nobre M. All-on-4 immediate-function concept with Brånemark System implants for completely edentulous maxillae: a 1-year retrospective clinical study. Clin Implant Dent Relat Res 2005; 7 Suppl 1:S88-94. doi: 10.1111/j.1708-8208.2005.tb00080.x [Crossref] [ Google Scholar]
- Malo P, de Araújo Nobre M, Lopes A. Immediate rehabilitation of completely edentulous arches with a four-implant prosthesis concept in difficult conditions: an open cohort study with a mean follow-up of 2 years. Int J Oral Maxillofac Implants 2012; 27(5):1177-90. [ Google Scholar]
- Jung RE, Schneider D, Ganeles J, Wismeijer D, Zwahlen M, Hämmerle CH. Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implants 2009; 24 Suppl:92-109. [ Google Scholar]
- Tallarico M, Meloni SM, Canullo L, Caneva M, Polizzi G. Five-year results of a randomized controlled trial comparing patients rehabilitated with immediately loaded maxillary cross-arch fixed dental prosthesis supported by four or six implants placed using guided surgery. Clin Implant Dent Relat Res 2016; 18(5):965-72. doi: 10.1111/cid.12380 [Crossref] [ Google Scholar]
- Maló P, Nunes M, de Araújo Nobre M, Lopes A, Ferro A. Extramaxillary zygomatic implants. In: Chow J, ed. Zygomatic Implants. Cham: Springer; 2020. p. 87-107. 10.1007/978-3-030-29264-5_6.
- Soto-Penaloza D, Zaragozí-Alonso R, Penarrocha-Diago M, Penarrocha-Diago M. The all-on-four treatment concept: Systematic review. J Clin Exp Dent 2017; 9(3):e474-e88. doi: 10.4317/jced.53613 [Crossref] [ Google Scholar]
- Patzelt SB, Bahat O, Reynolds MA, Strub JR. The all-on-four treatment concept: a systematic review. Clin Implant Dent Relat Res 2014; 16(6):836-55. doi: 10.1111/cid.12068 [Crossref] [ Google Scholar]
- Heydecke G, Zwahlen M, Nicol A, Nisand D, Payer M, Renouard F. What is the optimal number of implants for fixed reconstructions: a systematic review. Clin Oral Implants Res 2012; 23 Suppl 6:217-28. doi: 10.1111/j.1600-0501.2012.02548.x [Crossref] [ Google Scholar]
- Lopes A, Maló P, de Araújo Nobre M, Sanchez-Fernández E. The NobelGuide® All-on-4® treatment concept for rehabilitation of edentulous jaws: a prospective report on medium- and long-term outcomes. Clin Implant Dent Relat Res 2015; 17 Suppl 2:e406-16. doi: 10.1111/cid.12260 [Crossref] [ Google Scholar]
- Hegde P, Shenoy S, Rodrigues S, Shetty T, Pai U, Saldhana S. A study to compare the stress patterns in the edentulous mandibular bone around the two implant retained over denture and the prosthesis restored with all-on-four concept using the three dimensional finite element analysis. Indian J Forensic Med Toxicol 2020; 14(1):130-3. doi: 10.37506/ijfmt.v14i1.27 [Crossref] [ Google Scholar]
- Agliardi EL, Pozzi A, Stappert CF, Benzi R, Romeo D, Gherlone E. Immediate fixed rehabilitation of the edentulous maxilla: a prospective clinical and radiological study after 3 years of loading. Clin Implant Dent Relat Res 2014; 16(2):292-302. doi: 10.1111/j.1708-8208.2012.00482.x [Crossref] [ Google Scholar]
- Bhering CL, Mesquita MF, Kemmoku DT, Noritomi PY, Consani RL, Barão VA. Comparison between all-on-four and all-on-six treatment concepts and framework material on stress distribution in atrophic maxilla: a prototyping guided 3D-FEA study. Mater Sci Eng C Mater Biol Appl 2016; 69:715-25. doi: 10.1016/j.msec.2016.07.059 [Crossref] [ Google Scholar]
- opez MA, Andreasi Bassi M, Confalone L, Carinci F. Regeneration of atrophic crestal ridges with resorbable lamina: technical note. J Biol Regul Homeost Agents 2015; 29(3 Suppl 1):97-100. [ Google Scholar]
- Baj A, Trapella G, Lauritano D, Candotto V, Mancini GE, Giannì AB. An overview on bone reconstruction of atrophic maxilla: success parameters and critical issues. J Biol Regul Homeost Agents 2016; 30(2 Suppl 1):209-15. [ Google Scholar]
- Chiapasco M, Casentini P, Zaniboni M. Bone augmentation procedures in implant dentistry. Int J Oral Maxillofac Implants 2009; 24 Suppl:237-59. [ Google Scholar]
- Aloy-Prósper A, Peñarrocha-Oltra D, Peñarrocha-Diago M, Peñarrocha-Diago M. The outcome of intraoral onlay block bone grafts on alveolar ridge augmentations: a systematic review. Med Oral Patol Oral Cir Bucal 2015; 20(2):e251-8. doi: 10.4317/medoral.20194 [Crossref] [ Google Scholar]
- González-Valls G, Roca-Millan E, Céspedes-Sánchez JM, González-Navarro B, Torrejon-Moya A, López-López J. Narrow diameter dental implants as an alternative treatment for atrophic alveolar ridges systematic review and meta-analysis. Materials (Basel) 2021; 14(12):3234. doi: 10.3390/ma14123234 [Crossref] [ Google Scholar]
- Jensen SS, Terheyden H. Bone augmentation procedures in localized defects in the alveolar ridge: clinical results with different bone grafts and bone-substitute materials. Database of Abstracts of Reviews of Effects (DARE): Quality-Assessed Reviews [Internet]. York, UK: Centre for Reviews and Dissemination; 1995.
- Starch-Jensen T, Jensen JD. Maxillary sinus floor augmentation: a review of selected treatment modalities. J Oral Maxillofac Res 2017; 8(3):e3. doi: 10.5037/jomr.2017.8303 [Crossref] [ Google Scholar]
- Bedrossian E, Stumpel L 3rd, Beckely ML, Indresano T. The zygomatic implant: preliminary data on treatment of severely resorbed maxillae A clinical report. Int J Oral Maxillofac Implants 2002; 17(6):861-5. [ Google Scholar]
- Chiapasco M, Gatti C, Gatti F. Immediate loading of dental implants placed in severely resorbed edentulous mandibles reconstructed with autogenous calvarial grafts. Clin Oral Implants Res 2007; 18(1):13-20. doi: 10.1111/j.1600-0501.2006.01293.x [Crossref] [ Google Scholar]
- von Arx T, Buser D. Horizontal ridge augmentation using autogenous block grafts and the guided bone regeneration technique with collagen membranes: a clinical study with 42 patients. Clin Oral Implants Res 2006; 17(4):359-66. doi: 10.1111/j.1600-0501.2005.01234.x [Crossref] [ Google Scholar]
- Kuchler U, von Arx T. Horizontal ridge augmentation in conjunction with or prior to implant placement in the anterior maxilla: a systematic review. Int J Oral Maxillofac Implants 2014; 29 Suppl:14-24. doi: 10.11607/jomi.2014suppl.g1.1 [Crossref] [ Google Scholar]
- Troeltzsch M, Troeltzsch M, Kauffmann P, Gruber R, Brockmeyer P, Moser N. Clinical efficacy of grafting materials in alveolar ridge augmentation: a systematic review. J Craniomaxillofac Surg 2016; 44(10):1618-29. doi: 10.1016/j.jcms.2016.07.028 [Crossref] [ Google Scholar]
- Terheyden H. Interpositional bone grafts: sandwich interposition in the lateral mandible and Le Fort I interposition in the maxilla. In: Artzi Z, ed. Bone Augmentation by Anatomical Region: Techniques and Decision‐Making. Wiley; 2020. p. 453-69.
- Roccuzzo M, Ramieri G, Spada MC, Bianchi SD, Berrone S. Vertical alveolar ridge augmentation by means of a titanium mesh and autogenous bone grafts. Clin Oral Implants Res 2004; 15(1):73-81. doi: 10.1111/j.1600-0501.2004.00998.x [Crossref] [ Google Scholar]
- Ortega-Mejia H, Estrugo-Devesa A, Saka-Herrán C, Ayuso-Montero R, López-López J, Velasco-Ortega E. Platelet-rich plasma in maxillary sinus augmentation: systematic review. Materials (Basel) 2020; 13(3):622. doi: 10.3390/ma13030622 [Crossref] [ Google Scholar]
- Del Fabbro M, Wallace SS, Testori T. Long-term implant survival in the grafted maxillary sinus: a systematic review. Int J Periodontics Restorative Dent 2013; 33(6):773-83. doi: 10.11607/prd.1288 [Crossref] [ Google Scholar]
- Balshi TJ, Wolfinger GJ. Management of the posterior maxilla in the compromised patient: historical, current, and future perspectives. Periodontol 2000 2003; 33:67-81. doi: 10.1046/j.0906-6713.2002.03306.x [Crossref] [ Google Scholar]
- Mangano C, Scarano A, Perrotti V, Iezzi G, Piattelli A. Maxillary sinus augmentation with a porous synthetic hydroxyapatite and bovine-derived hydroxyapatite: a comparative clinical and histologic study. Int J Oral Maxillofac Implants 2007; 22(6):980-6. [ Google Scholar]
- Hämmerle CH, Jung RE, Feloutzis A. A systematic review of the survival of implants in bone sites augmented with barrier membranes (guided bone regeneration) in partially edentulous patients. J Clin Periodontol 2002; 29 Suppl 3:226-31. doi: 10.1034/j.1600-051x.29.s3.14.x [Crossref] [ Google Scholar]
- Thoma DS, Cha JK, Jung UW. Treatment concepts for the posterior maxilla and mandible: short implants versus long implants in augmented bone. J Periodontal Implant Sci 2017; 47(1):2-12. doi: 10.5051/jpis.2017.47.1.2 [Crossref] [ Google Scholar]
- Block MS, Haggerty CJ, Fisher GR. Nongrafting implant options for restoration of the edentulous maxilla. J Oral Maxillofac Surg 2009; 67(4):872-81. doi: 10.1016/j.joms.2008.10.008 [Crossref] [ Google Scholar]
- Cucchi A, Vignudelli E, Napolitano A, Marchetti C, Corinaldesi G. Evaluation of complication rates and vertical bone gain after guided bone regeneration with non-resorbable membranes versus titanium meshes and resorbable membranes A randomized clinical trial. Clin Implant Dent Relat Res 2017; 19(5):821-32. doi: 10.1111/cid.12520 [Crossref] [ Google Scholar]
- Chin M, Toth BA. Distraction osteogenesis in maxillofacial surgery using internal devices: review of five cases. J Oral Maxillofac Surg 1996; 54(1):45-53. doi: 10.1016/s0278-2391(96)90303-1 [Crossref] [ Google Scholar]
- Ugurlu F, Sener BC, Dergin G, Garip H. Potential complications and precautions in vertical alveolar distraction osteogenesis: a retrospective study of 40 patients. J Craniomaxillofac Surg 2013; 41(7):569-73. doi: 10.1016/j.jcms.2012.11.028 [Crossref] [ Google Scholar]
- Aikawa T, Iida S, Isomura ET, Namikawa M, Matsuoka Y, Yamada C. Breakage of internal maxillary distractor: considerable complication of maxillary distraction osteogenesis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 106(1):e1-7. doi: 10.1016/j.tripleo.2008.03.035 [Crossref] [ Google Scholar]
- Spencer KR. Implant based rehabilitation options for the atrophic edentulous jaw. Aust Dent J 2018; 63 Suppl 1:S100-S7. doi: 10.1111/adj.12595 [Crossref] [ Google Scholar]
- Terheyden H. A new technique of Le Fort I interpositional grafting for dental implants. Int J Oral Maxillofac Surg 2017; 46(1):53-4. doi: 10.1016/j.ijom.2017.02.197 [Crossref] [ Google Scholar]
- Aghaloo TL, Misch C, Lin GH, Iacono VJ, Wang HL. Bone augmentation of the edentulous maxilla for implant placement: a systematic review. Int J Oral Maxillofac Implants 2016; 31 Suppl:s19-30. doi: 10.11607/jomi.16suppl.g1 [Crossref] [ Google Scholar]
- Roccuzzo A, Marchese S, Worsaae N, Jensen SS. The sandwich osteotomy technique to treat vertical alveolar bone defects prior to implant placement: a systematic review. Clin Oral Investig 2020; 24(3):1073-89. doi: 10.1007/s00784-019-03183-6 [Crossref] [ Google Scholar]
- Dahl G. Dental implants and superplants. Rassegna Trimestrale Odont 1956; 4:25-36. [ Google Scholar]
- Takaoka K, Segawa E, Noguchi K, Kishimoto H, Urade M. Maxillary subperiosteal implantitis that caused severe bone resorption of the maxilla with perforation of the maxillary sinus and sinusitis: a case report. Open J Stomatol 2013; 3(3):33704. doi: 10.4236/ojst.2013.33039 [Crossref] [ Google Scholar]
- Nguyen TM, Caruhel JB, Khonsari RH. A subperiosteal maxillary implant causing severe osteolysis. J Stomatol Oral Maxillofac Surg 2018; 119(6):523-5. doi: 10.1016/j.jormas.2018.06.007 [Crossref] [ Google Scholar]
- Nisand D, Renouard F. Short implant in limited bone volume. Periodontol 2000 2014; 66(1):72-96. doi: 10.1111/prd.12053 [Crossref] [ Google Scholar]
- Merli M, Moscatelli M, Pagliaro U, Mariotti G, Merli I, Nieri M. Implant prosthetic rehabilitation in partially edentulous patients with bone atrophy An umbrella review based on systematic reviews of randomised controlled trials. Eur J Oral Implantol 2018; 11(3):261-80. [ Google Scholar]
- Pjetursson BE, Ignjatovic D, Matuliene G, Brägger U, Schmidlin K, Lang NP. Transalveolar maxillary sinus floor elevation using osteotomes with or without grafting material Part II: radiographic tissue remodeling. Clin Oral Implants Res 2009; 20(7):677-83. doi: 10.1111/j.1600-0501.2009.01721.x [Crossref] [ Google Scholar]
- Nedir R, Bischof M, Briaux JM, Beyer S, Szmukler-Moncler S, Bernard JP. A 7-year life table analysis from a prospective study on ITI implants with special emphasis on the use of short implants Results from a private practice. Clin Oral Implants Res 2004; 15(2):150-7. doi: 10.1111/j.1600-0501.2004.00978.x [Crossref] [ Google Scholar]
- Chrcanovic BR, Abreu MH. Survival and complications of zygomatic implants: a systematic review. Oral Maxillofac Surg 2013; 17(2):81-93. doi: 10.1007/s10006-012-0331-z [Crossref] [ Google Scholar]
- Chrcanovic BR, Albrektsson T, Wennerberg A. Survival and complications of zygomatic implants: an updated systematic review. J Oral Maxillofac Surg 2016; 74(10):1949-64. doi: 10.1016/j.joms.2016.06.166 [Crossref] [ Google Scholar]
- Tuminelli FJ, Walter LR, Neugarten J, Bedrossian E. Immediate loading of zygomatic implants: a systematic review of implant survival, prosthesis survival and potential complications. Eur J Oral Implantol 2017; 10 Suppl 1:79-87. [ Google Scholar]
- Wang F, Monje A, Lin GH, Wu Y, Monje F, Wang HL. Reliability of four zygomatic implant-supported prostheses for the rehabilitation of the atrophic maxilla: a systematic review. Int J Oral Maxillofac Implants 2015; 30(2):293-8. doi: 10.11607/jomi.3691 [Crossref] [ Google Scholar]
- Davó R, Malevez C, López-Orellana C, Pastor-Beviá F, Rojas J. Sinus reactions to immediately loaded zygoma implants: a clinical and radiological study. Eur J Oral Implantol 2008; 1(1):53-60. [ Google Scholar]
- Davó R, Malevez C, Rojas J, Rodríguez J, Regolf J. Clinical outcome of 42 patients treated with 81 immediately loaded zygomatic implants: a 12- to 42-month retrospective study. Eur J Oral Implantol 2008; 9 Suppl 1(2):141-50. [ Google Scholar]
- Dominguez EA, Guerrero C, Shehata E, Van Sickels JE. Zygoma implants or sinus lift for the atrophic maxilla with a dentate mandible: which is the better option?. Dent Clin North Am 2019; 63(3):499-513. doi: 10.1016/j.cden.2019.02.013 [Crossref] [ Google Scholar]
- Chow J, Wat P, Hui E, Lee P, Li W. A new method to eliminate the risk of maxillary sinusitis with zygomatic implants. Int J Oral Maxillofac Implants 2010; 25(6):1233-40. [ Google Scholar]
- Malevez C. Zygomatic implants after 20 years: systematic overview and global perspective. In: Chow J, ed. Zygomatic Implants. Cham: Springer; 2020. p. 5-15. 10.1007/978-3-030-29264-5_2.
- Kahnberg KE, Henry PJ, Hirsch JM, Ohrnell LO, Andreasson L, Brånemark PI. Clinical evaluation of the zygoma implant: 3-year follow-up at 16 clinics. J Oral Maxillofac Surg 2007; 65(10):2033-8. doi: 10.1016/j.joms.2007.05.013 [Crossref] [ Google Scholar]
- Davó R, David L. Quad zygoma: technique and realities. Oral Maxillofac Surg Clin North Am 2019; 31(2):285-97. doi: 10.1016/j.coms.2018.12.006 [Crossref] [ Google Scholar]
- Davó R, Maté Sánchez de Val JE. Quad zygoma: immediate function in the severely atrophic maxilla. In: Chow J, ed. Zygomatic Implants. Cham: Springer; 2020. p. 109-27. 10.1007/978-3-030-29264-5_7.
- Agliardi EL, Romeo D, Panigatti S, de Araújo Nobre M, Maló P. Immediate full-arch rehabilitation of the severely atrophic maxilla supported by zygomatic implants: a prospective clinical study with minimum follow-up of 6 years. Int J Oral Maxillofac Surg 2017; 46(12):1592-9. doi: 10.1016/j.ijom.2017.05.023 [Crossref] [ Google Scholar]
- Maló P, de Araujo Nobre M, Lopes I. A new approach to rehabilitate the severely atrophic maxilla using extramaxillary anchored implants in immediate function: a pilot study. J Prosthet Dent 2008; 100(5):354-66. doi: 10.1016/s0022-3913(08)60237-1 [Crossref] [ Google Scholar]
- Li J, Wang HL. Common implant-related advanced bone grafting complications: classification, etiology, and management. Implant Dent 2008; 17(4):389-401. doi: 10.1097/ID.0b013e31818c4992 [Crossref] [ Google Scholar]
- Fan T, Li Y, Deng WW, Wu T, Zhang W. Short implants (5 to 8 mm) versus longer implants ( > 8 mm) with sinus lifting in atrophic posterior maxilla: a meta-analysis of RCTs. Clin Implant Dent Relat Res 2017; 19(1):207-15. doi: 10.1111/cid.12432 [Crossref] [ Google Scholar]
- Albrektsson T, Brånemark PI, Eriksson A, Lindström J. The preformed autologous bone graft An experimental study in the rabbit. Scand J Plast Reconstr Surg 1978; 12(3):215-23. doi: 10.3109/02844317809012997 [Crossref] [ Google Scholar]
- Fernández H, Gómez-Delgado A, Trujillo-Saldarriaga S, Varón-Cardona D, Castro-Núñez J. Zygomatic implants for the management of the severely atrophied maxilla: a retrospective analysis of 244 implants. J Oral Maxillofac Surg 2014; 72(5):887-91. doi: 10.1016/j.joms.2013.12.029 [Crossref] [ Google Scholar]
- Linkow LI, Ghalili R. Critical design errors in maxillary subperiosteal implants. J Oral Implantol 1998; 24(4):198-205. doi: 10.1563/1548-1336(1998)024<0198:cdeims>2.3.co;2 [Crossref] [ Google Scholar]
- Toti P, Marchionni S, Menchini-Fabris GB, Marconcini S, Covani U, Barone A. Surgical techniques used in the rehabilitation of partially edentulous patients with atrophic posterior mandibles: a systematic review and meta-analysis of randomized controlled clinical trials. J Craniomaxillofac Surg 2017; 45(8):1236-45. doi: 10.1016/j.jcms.2017.04.011 [Crossref] [ Google Scholar]
- Esposito M, Felice P, Worthington HV. Interventions for replacing missing teeth: augmentation procedures of the maxillary sinus. Cochrane Database Syst Rev. 2014(5):CD008397. 10.1002/14651858.CD008397.pub2.
- Terheyden H, Meijer GJ, Raghoebar GM. Vertical bone augmentation and regular implants versus short implants in the vertically deficient posterior mandible: a systematic review and meta-analysis of randomized studies. Int J Oral Maxillofac Surg 2021; 50(9):1249-58. doi: 10.1016/j.ijom.2021.01.005 [Crossref] [ Google Scholar]
- Rodríguez-Chessa JG, Olate S, Netto HD, Shibli J, de Moraes M, Mazzonetto R. Treatment of atrophic maxilla with zygomatic implants in 29 consecutives patients. Int J Clin Exp Med 2014; 7(2):426-30. [ Google Scholar]
- Durkan R, Oyar P, Deste G. Maxillary and mandibular all-on-four implant designs: a review. Niger J Clin Pract 2019; 22(8):1033-40. doi: 10.4103/njcp.njcp_273_18 [Crossref] [ Google Scholar]